No products in the cart.
Moxonidine Canon, 0.4 mg 14 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
An antihypertensive agent. The mechanism of action of moxonidine is associated mainly with its effect on central parts of BP regulation. Moxonidine is an agonist of mainly imidazoline receptors.
With excitation of the above receptors of the neurons of the solitary tract, moxonidine through the system of inhibitory interneurons promotes inhibition of the activity of the vasomotor center and thus – reduction of descending sympathetic effects on the cardiovascular system. BP (systolic and diastolic) decreases gradually. Moxonidine differs from other sympatholytic hypotensive agents in its lower affinity for α2-adrenoreceptors, which explains the lower probability of sedation and dry mouth.
Moxonidine increases insulin sensitivity index (compared to placebo) by 21% in patients with obesity, insulin resistance and moderate arterial hypertension.
Pharmacokinetics
After oral administration, moxonidine is rapidly and almost completely absorbed in the upper gastrointestinal tract. Absolute bioavailability is approximately 88%. Time to reach Cmax is about 1 hour. Food intake has no effect on the pharmacokinetics of moxonidine. Binding to plasma proteins is 7.2%. The main metabolite of moxonidine is dehydrated moxonidine and guanidine derivatives. The pharmacodynamic activity of dehydrated moxonidine is about 10% compared to moxonidine.
The T1/2 of moxonidine and the metabolite is 2.5 and 5 h, respectively. Within 24 h, more than 90% of moxonidine is excreted by the kidneys (about 78% unchanged and 13% as dehydroromoxonidine, other metabolites in the urine do not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestine.
In comparison with healthy volunteers, patients with arterial hypertension show no changes in the pharmacokinetics of moxonidine.
There were clinically insignificant changes in pharmacokinetic parameters of moxonidine in elderly patients, probably due to decrease of its metabolism intensity and/or slightly higher bioavailability.
The excretion of moxonidine correlates significantly with CK. In patients with moderate renal impairment (CKD 30-60 ml/min), plasma Css and final T1/2 are approximately 2 and 1.5 times higher than in those with normal renal function (CKD greater than 90 ml/min). In patients with severe renal impairment (CKR less than 30 mL/min), plasma Css and final T1/2 are 3 times higher than in patients with normal renal function. Multiple-dose administration of moxonidine leads to predictable cumulation in patients with moderate to severe renal failure. In patients with terminal renal failure (CKD less than 10 ml/min) on hemodialysis, Css in plasma and final T1/2 are 6 and 4 times higher, respectively, than in patients with normal renal function. Plasma Cmax of moxonidine is 1.5-2 times higher in all groups. The dose should be adjusted individually in patients with impaired renal function. Moxonidine is slightly excreted during hemodialysis.
Indications
Indications
Arterial hypertension
Active ingredient
Active ingredient
Composition
Composition
Active substance:
Moxonidine 0.4 mg.
Auxiliary substances:
microcrystalline cellulose,
aerosil A-380,
polyvinylpyrrolidone,
/p>
magnesium stearate,
hydroxypropyl cellulose (clucel),
castor oil,
tween-80.
How to take, the dosage
How to take, the dosage
Ingestion, regardless of meals, with plenty of fluid. In most cases, the initial dose of moxonidine is 0.2 mg per day, in a single dose, preferably in the morning hours. If the therapeutic effect is insufficient, the dose may be increased after 3 weeks of therapy to 0.4 mg per day in 2 doses or a single dose. The maximum daily dose to be divided into 2 doses (morning and evening) is 0.6 mg. The maximum single dose is 0.4 mg.
In elderly patients with normal renal function, the dosing recommendations are the same as for adult patients.
In patients with renal insufficiency (cretinine clearance 30-60 ml per minute) and patients on hemodialysis, the single dose should not exceed 0.2 mg, the maximum daily dose 0.4 mg.
Interaction
Interaction
Moxonidine may be administered with thiazide diuretics and “slow” calcium channel blockers. When co-administration of moxonidine with these and other hypotensive agents, mutual enhancement of moxonidine action occurs.
When prescribing moxonidine with hydrochlorothiazide, glibenclamide (gliburide) or digoxin there is no pharmacokinetic interaction.
Tricyclic antidepressants may decrease the effectiveness of centrally acting antihypertensive agents.
Beta-adrenoblockers increase bradycardia and the severity of the negative ino- and dromotropic effects of moxonidine.
Moxynidine moderately enhances impaired cognitive ability in patients taking lorazepam.
Prescribing moxonidine with benzodiazepines may be accompanied by an increased sedative effect of the latter.
There is no pharmacodynamic interaction when prescribing moxonidine with moclobemide.
Special Instructions
Special Instructions
If it is necessary to cancel simultaneously taken beta-adrenoblockers and moxonidine, first the beta-adrenoblockers and only after several days the moxonidine should be cancelled. It is not recommended to prescribe tricyclic antidepressants simultaneously with moxonidine. Alcohol consumption is excluded during treatment. Regular monitoring of blood pressure, heart rate and ECG is necessary during treatment.
Moxonidine may be prescribed with thiazide diuretics, ACE inhibitors and slow calcium channel blockers.
Moxonidine should be stopped gradually.
Contraindications
Contraindications
Extended bradycardia (less than 50 bpm), CCSU, AV blockade of II and III degree, acute and chronic heart failure, lactation (breast-feeding), children and adolescents under 18 years of age, hypersensitivity to moxonidine.
Side effects
Side effects
Especially at the beginning of therapy the most frequent adverse reactions were: dry mouth, headache, dizziness, asthenia, peripheral edema, allergic reactions, nausea, constipation, somnolence. Their intensity and frequency decrease with repeated administration. Anorexia, parotid gland pain, urinary retention or incontinence, dry eye, orthostatic hypotension, Raynaud’s syndrome, endocrine disorders, cholelithiasis have been reported.
Overdose
Overdose
Symptoms: headache, sedation, drowsiness, excessive BP decrease, dizziness, general weakness, bradycardia, dry mouth, vomiting, fatigue, stomach pain. Short-term elevated BP, tachycardia, and hyperglycemia are also potentially possible.
Treatment: symptomatic. Gastric lavage (immediately after ingestion), administration of activated charcoal and laxatives, symptomatic therapy. In case of BP decrease it is recommended to restore the volume of circulating blood by administering fluids. Bradycardia may be stopped by atropine. Alpha-adrenoreceptor antagonists may reduce or eliminate transient arterial hypertension in moxonidine overdose. Idazoxan (an imidazoline antagonist) is administered as a specific antidote.
Similarities
Similarities
Additional information
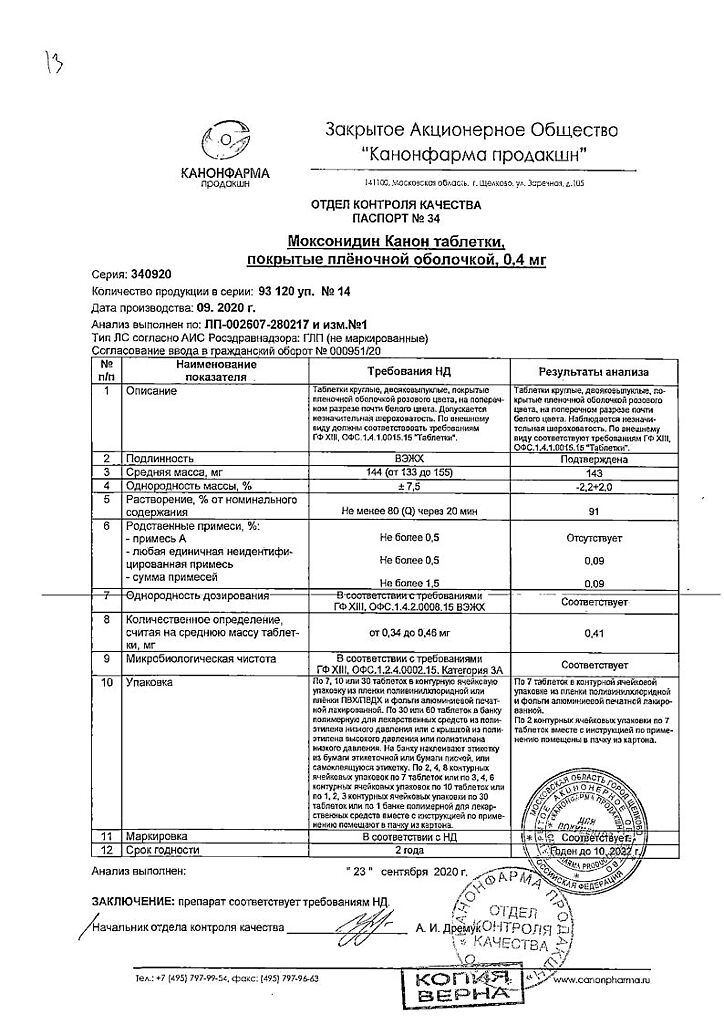
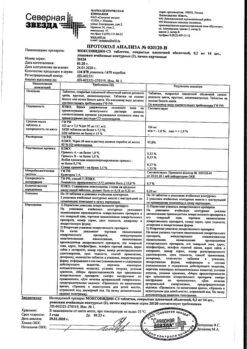
| Shelf life | 2 years |
|---|---|
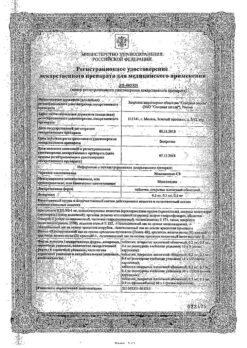
| Manufacturer | Kanonfarma Production ZAO, Russia |
| Medication form | pills |
| Brand | Kanonfarma Production ZAO |
Other forms…
Related products
Buy Moxonidine Canon, 0.4 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.