No products in the cart.
Description
Rheumatoid arthritis, No
Indications
Indications
Trophoblastic tumors; acute leukemia (especially lymphoblastic and myeloblastic variants); neuroleukemia; non-Hodgkin’s lymphomas (including lymphosarcoma); breast cancer, squamous cell cancer of the head and neck, lung cancer, skin cancer, cervical cancer, vulvar cancer, esophageal cancer, bladder cancer, testicular cancer, ovarian cancer, penile cancer, retinoblastoma, medulloblastoma; osteogenic sarcoma and soft tissue sarcoma; mycosis fungoides (advanced stages);
Severe forms of psoriasis, psoriatic arthritis, rheumatoid arthritis, juvenile chronic arthritis, dermatomyositis, systemic lupus erythematosus, ankylosing spondylitis (if standard therapy is ineffective).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Antitumor agent, antimetabolite
Pharmacological action
Antitumor, cytostatic agent of the group of antimetabolites – folic acid analogues.
Inhibits dihydrofolate reductase, which is involved in the reduction of dihydrofolic acid to tetrahydrofolic acid (a carrier of carbon fragments necessary for the synthesis of purine nucleotides and their derivatives).
Inhibits DNA synthesis, repair and cell mitosis (in S-phase). Tissues with high cell proliferation are especially sensitive to the action of methotrexate: tumor tissue, bone marrow, epithelial cells of the mucous membranes, embryonic cells.
The mechanism of action in rheumatoid arthritis is associated with the immunomodulatory and anti-inflammatory effect of the drug and is due to the induction of apoptosis of rapidly proliferating cells (activated T-lymphocytes, fibroblasts, synoviocytes), inhibition of the synthesis of anti-inflammatory cytokines (interleukin (IL)-1, tumor necrosis factor alpha), increased synthesis of anti-inflammatory cytokines IL-4, IL-10 and suppression of activity metalloproteinases.
In patients with rheumatoid arthritis, the use of methotrexate reduces symptoms of inflammation (pain, swelling, stiffness), but there is limited research on long-term use (regarding the ability to maintain remission in rheumatoid arthritis).
In psoriasis, the growth rate of keratinocytes in psoriatic plaques increases compared to normal proliferation of skin cells. This difference in cell proliferation is the basis for the use of methotrexate to treat psoriasis.
Pharmacokinetics
With intramuscular administration, Cmax of methotrexate in blood plasma is achieved within 30-60 minutes. Systemic absorption of methotrexate after injection under the skin of the abdomen and thigh is the same. After intravenous administration, it is quickly distributed within a volume equivalent to the total volume of body fluids. Initial Vd is 0.18 l/kg (18% of body weight), the equilibrium volume of distribution is 0.4-0.8 l/kg (40-80% of body weight). 50-60% of methotrexate circulating in the vascular bed is associated with proteins (mainly albumin). Competitive displacement is possible when used simultaneously with sulfonamides, salicylates, tetracyclines, chloramphenicols, and phenytoin. Methotrexate does not cross the BBB when used in therapeutic doses. High concentrations of methotrexate in the central nervous system can be achieved with intrathecal administration. Methotrexate undergoes hepatic and intracellular metabolism to form a pharmacologically active polyglutamine form, which also inhibits dihydrofolate reductase and thymidine synthesis. Small amounts of methotrexate polyglutamate may remain in tissues for a long period of time. The persistence and prolongation of action of the active metabolites of methotrexate vary depending on the type of cells, tissues and tumors. The average T1/2 values when using methotrexate at a dose of less than 30 mg/m2 are 6-7 hours. In patients receiving high doses of methotrexate, T1/2 is 8-17 hours. In chronic renal failure, both phases of methotrexate elimination can be significantly prolonged. It is excreted primarily by the kidneys unchanged through glomerular filtration and tubular secretion (with intravenous administration, 80-90% is excreted within 24 hours), up to 10% is excreted with bile (followed by reabsorption in the intestine). Methotrexate accumulates in the liver, kidneys and organs over several weeks or months. With repeated administration, it accumulates in tissues in the form of polyglutamates.
Special instructions
Special instructions
Methotrexate should not be used for ascites, pleural effusion, gastric and duodenal ulcers, ulcerative colitis, gout or nephropathy (including a history).
It is not recommended for use in patients with chickenpox (including recent or after contact with sick people), herpes zoster and other acute infectious diseases.
Before starting therapy and during treatment, the peripheral blood picture, liver and kidney function, and chest x-ray should be monitored.
When treating rheumatoid arthritis or psoriasis, a complete general blood test should be done at least once a month, and laboratory tests of liver or kidney function at least once every 1-2 months.
When used for psoriasis, local treatment of the disease should not be interrupted. In case of overdose, it is recommended to use calcium folinate (but no later than after 4 hours).
When conducting combination antitumor therapy, special caution should be exercised when using methotrexate in high doses simultaneously with drugs that have a nephrotoxic effect (for example, cisplatin).
It is not recommended to vaccinate patients and their families.
Caution should be used when combining methotrexate (even in low doses) with acetylsalicylic acid.
Experimental studies have established the carcinogenic and mutagenic effects of methotrexate.
Methotrexate is a cytotoxic agent and must be handled with caution. Methotrexate should be prescribed by a doctor who has experience in its use and is familiar with the properties and characteristics of the action of methotrexate. Before prescribing methotrexate, you should ensure that it is possible to determine its plasma concentration.
Taking into account the possibility of developing severe toxic reactions, incl. with a fatal outcome, the doctor is obliged to inform the patient in detail about the possible risk and the necessary precautions. Methotrexate, especially in medium and high doses, should be used only in patients with potentially life-threatening malignancies. Cases of fatal toxicity have been described during methotrexate therapy. Discontinuation of methotrexate does not always lead to complete resolution of adverse events.
During treatment with methotrexate, patients should be under close medical supervision in order to promptly identify signs of possible toxicity and adverse effects.
Because of the potential for serious (and potentially fatal) toxic reactions, methotrexate should only be used in patients with severe, persistent and disabling psoriasis that is not responsive to other treatments. Patients receiving methotrexate treatment should be closely monitored to identify and evaluate signs of possible toxic effects or adverse reactions with minimal delay.
Before starting treatment with methotrexate or when resuming therapy after a break, it is necessary to conduct a clinical blood test with counting the leukocyte formula and platelet count, assess the activity of liver transaminases, the concentration of bilirubin, blood plasma albumin, the concentration of uric acid in the blood plasma, kidney function (urea nitrogen, creatinine clearance and/or plasma creatinine), as well as an X-ray examination of the chest organs. If there are clinical indications, studies are prescribed to exclude tuberculosis and viral hepatitis.
Prescribing high doses of methotrexate is possible only if the concentration of creatinine in the blood plasma is normal. If an increase in creatinine concentration is observed, the dose of methotrexate should be reduced; if the creatinine concentration increases by more than 2 mg/dL, methotrexate should not be used. Before combination therapy, including treatment with high-dose methotrexate, the white blood cell and platelet counts should be above the minimum values specified in the treatment protocol (white blood cell count from 1000 to 1500/μl, platelet count from 50,000 to 100,000/μl).
Leukopenia and thrombocytopenia, as a rule, develop within 4 to 14 days from the moment of methotrexate administration. Sometimes the development of a second leukopenic phase is observed, developing in a period of 12 to 21 days.
In elderly patients, the development of megaloblastic anemia has been described during prolonged therapy with methotrexate.
During treatment with methotrexate, the following studies are carried out (monthly for the first 6 months, then at least every 3 months; with increasing doses, it is advisable to increase the frequency of examinations):
Examination of the oral cavity and pharynx to identify changes in the mucous membranes.
Blood test to determine the leukocyte formula and platelet count. Even when used in normal therapeutic doses, methotrexate can suddenly cause suppression of hematopoiesis. If there is a significant decrease in the number of leukocytes or platelets, treatment with methotrexate is stopped immediately and symptomatic supportive therapy is prescribed. Patients should be instructed to immediately report any signs and symptoms indicating an infection to their physician. During concomitant therapy or previous therapy with hematotoxic drugs (for example, leflunomide), radiation therapy, it is necessary to carefully monitor the number of leukocytes and platelets in the blood. If necessary, it is advisable to perform a bone marrow biopsy.
Functional liver tests. Long-term use of methotrexate may result in the development of acute hepatitis and chronic hepatotoxicity (liver fibrosis and cirrhosis). Particular attention should be paid to identifying signs of liver damage. Treatment with methotrexate should not be started or should be suspended if abnormal liver function tests or liver biopsy are detected. During methotrexate therapy, a 2-3-fold transient increase in the activity of liver transaminases is possible, usually asymptomatic. As a rule, this is not a reason to change the treatment regimen; usually the indicators normalize within 2 weeks, after which treatment can be resumed according to the doctor’s decision. However, if a persistent increase in the activity of liver transaminases is detected, it is necessary to reduce the dose or discontinue treatment with methotrexate. Since methotrexate has a toxic effect on the liver, other hepatotoxic drugs should not be used during treatment unless clearly necessary. Ethanol consumption should also be avoided or greatly reduced. Liver enzyme activity should be especially closely monitored in patients receiving concomitant therapy with other hepatotoxic and hematotoxic drugs (in particular, leflunomide).
In case of long-term treatment, especially severe forms of psoriasis, including psoriatic arthritis, due to the possible hepatotoxic effect of methotrexate, given that fibrotic and/or cirrhotic changes can develop against the background of normal liver tests, a liver biopsy is necessary in the following cases:
in patients without risk factors until the total cumulative dose reaches 1.0-1.5 g;
in the presence of risk factors such as alcohol abuse, persistent elevation of liver transaminases, chronic viral hepatitis, family history of liver disease, as well as for patients with less significant risk factors such as diabetes mellitus, obesity, history of exposure to hepatotoxic drugs/chemicals, a liver biopsy should be performed 2-4 months after the start of treatment. After reaching a total cumulative dose of 1.0-1.5 g, a repeat liver biopsy is recommended.
Liver biopsy is not indicated in elderly patients; in patients with active acute diseases (for example, respiratory system); in patients with contraindications to liver biopsy (for example, unstable hemodynamics, changes in coagulogram parameters); in patients with a poor prognosis for life expectancy.
If liver biopsy reveals only mild changes (grade I, II or IIIa on the Roenigk scale), continued methotrexate therapy may be possible, subject to careful monitoring of the patient’s condition. Methotrexate should be discontinued if moderate or severe changes are detected (grades IIIb and IV according to the Roenigk scale), or if a liver biopsy is refused in a patient who has a persistent increase in liver transaminases. If moderate fibrosis or cirrhosis of the liver is detected, methotrexate should be discontinued; in case of minimal fibrosis, a repeat liver biopsy is recommended after 6 months. Changes such as fatty liver or mild inflammation of the portal veins are often detected on liver biopsy in patients receiving methotrexate. Although the detection of such changes is usually not a reason to make a decision about the inappropriateness or discontinuation of methotrexate therapy, caution should be exercised when treating such patients.
Renal function tests and urine examination. Since methotrexate is excreted primarily by the kidneys, patients with impaired renal function may experience increased plasma concentrations of methotrexate, which may result in severe adverse reactions. It is necessary to carefully monitor the condition of patients who may have impaired renal function (for example, elderly patients). This is especially important in the case of concomitant therapy with drugs that reduce the excretion of methotrexate, have an adverse effect on the kidneys (in particular, NSAIDs) or on the hematopoietic system. Cases of severe side effects have been described in patients taking NSAIDs during therapy with methotrexate (especially in high doses), including cases of severe suppression of bone marrow hematopoiesis, aplastic anemia, gastrointestinal damage and death. During methotrexate infusion, urine output and pH should also be monitored. To reduce renal toxicity and to prevent renal failure during treatment with high-dose methotrexate, adequate IV fluid supply and urine alkalinization (pH > 7) are absolutely necessary. Treatment with methotrexate may worsen renal function with increases in certain laboratory parameters (creatinine, urea, serum uric acid), which may lead to acute renal failure with oliguria/anuria. This is likely due to precipitation of methotrexate and its metabolites in the renal tubules.
Examination of the respiratory system. It is necessary to closely monitor symptoms of possible development of pulmonary function disorders and, if necessary, prescribe appropriate tests to monitor pulmonary function. The appearance of corresponding symptoms (especially a dry, nonproductive cough) or the development of nonspecific pneumonitis during treatment with methotrexate may indicate a potential danger of lung damage. In such cases, methotrexate should be discontinued and the patient should be carefully examined. Although the clinical presentation may vary, typical cases of respiratory symptoms caused by methotrexate include fever, cough with dyspnea, hypoxemia, and pulmonary infiltrates on x-ray. Lung damage caused by the use of methotrexate can occur regardless of how long it has been used or the doses used (cases of lung damage have been described when using methotrexate in low doses, including 7.5 mg/week). In differential diagnosis, the infectious nature of the disease should be excluded. During methotrexate therapy, the development of potentially dangerous (even fatal) opportunistic infections, including Pneumocystis pneumonia, is possible. If respiratory symptoms develop in a patient receiving methotrexate, pneumonia caused by Pneumocystis jirovecii should be excluded.
If the dose of methotrexate is increased, the frequency of examinations should be increased.
Due to the immunosuppressive effect of methotrexate, it is necessary to avoid immunization (unless approved by the physician) immediately during treatment and in the interval from 3 to 12 months after stopping the use of methotrexate; Family members living with the patient should refuse immunization with oral polio vaccine (the patient should avoid contact with people who have received the polio vaccine or wear a protective mask covering the nose and mouth). Also, due to the possible effect of methotrexate on the immune system, the results of assessing the effectiveness of vaccines and tests (immunological procedures for recording an immune response) may be distorted.
If stomatitis or diarrhea, hemoptysis, melena, or blood in the stool occur during methotrexate therapy, the drug must be discontinued immediately due to the high risk of potentially fatal complications, such as hemorrhagic enteritis and perforation of the intestinal wall.
Symptoms such as fever, sore throat, flu-like symptoms, ulceration of the oral mucosa, severe general weakness, hemoptysis, hemorrhagic rash may be harbingers of the development of life-threatening complications.
If a patient is diagnosed with conditions leading to the accumulation of a significant amount of fluid in the body cavities (hydrothorax, ascites), given the prolongation of the half-life of the drug in such patients, methotrexate therapy should be carried out with caution; before starting therapy, the fluid should be evacuated by drainage, or the use of methotrexate should be discontinued.
Particular caution should be observed when treating patients with insulin-dependent diabetes mellitus, as cases of the development of liver cirrhosis without a previous increase in the activity of liver transaminases have been described.
Like other cytotoxic drugs, methotrexate can cause the development of tumor lysis syndrome in patients with rapidly growing malignant neoplasms. To prevent the development of this complication, it is necessary to take appropriate supportive care measures.
The use of methotrexate in combination with radiation therapy may lead to an increased risk of developing soft tissue necrosis or osteonecrosis.
The condition of patients with previous radiation therapy, as well as impaired general condition, should be especially carefully monitored.
Dehydration can also potentiate the toxic effects of methotrexate, therefore, if conditions develop that can lead to dehydration (severe vomiting, diarrhea), methotrexate therapy should be interrupted until these conditions resolve. Cases of the development of leukoencephalopathy in patients receiving therapy with high doses of methotrexate, including orally, in combination with calcium folinate (without previous radiation therapy to the head area) have been described.
When using methotrexate for acute lymphocytic leukemia, pain in the left epigastric region may occur due to the development of an inflammatory process in the splenic capsule against the background of the breakdown of tumor cells.
It is recommended that methotrexate treatment be interrupted 1 week before surgery and restarted 1 or 2 weeks after surgery.
Particular caution should be exercised when using methotrexate in patients with active infections. The use of methotrexate in patients with immunodeficiency syndrome is contraindicated.
When body temperature rises (more than 38 °C), the elimination of methotrexate slows down significantly.
Methotrexate may increase the risk of developing neoplasms (mainly lymphomas). Malignant lymphomas can also develop in patients receiving low-dose methotrexate. In such cases, methotrexate should be discontinued. If spontaneous regression of lymphoma is not observed, therapy with other cytotoxic drugs is prescribed.
Before starting treatment with methotrexate, pregnancy must be excluded. Methotrexate has an embryotoxic effect, promotes abortion and the formation of fetal development abnormalities. Methotrexate therapy is accompanied by inhibition of spermatogenesis and oogenesis, which can lead to decreased fertility. After discontinuation of methotrexate therapy, these effects spontaneously regress. During methotrexate therapy and for 6 months after its completion, patients are recommended to use contraception. Patients of reproductive age, as well as their partners, should be informed about the possible effect of methotrexate on reproduction and fetal development. Men of reproductive age should be warned about the risks; fatherhood is not recommended during treatment and for 6 months after discontinuation of methotrexate. Since irreversible infertility may develop during treatment, men should consider cryopreserving sperm in a bank before starting treatment.
The use of methotrexate increases the likelihood of developing dermatitis and skin burns under the influence of solar and ultraviolet irradiation. Do not expose unprotected skin to sunlight for too long or overuse a UV lamp (photosensitization reaction is possible). In patients with psoriasis, an exacerbation of the disease may occur due to UV irradiation during treatment with the drug.
During therapy with high doses, precipitation of methotrexate or its metabolites in the renal tubules may occur. In such cases, to prevent this complication, it is recommended to carry out infusion therapy and alkalization of urine until a pH of 6.5-7.0 is achieved through oral or intravenous administration of sodium bicarbonate or acetazolamide.
During therapy with methotrexate, exacerbation of chronic viral hepatitis (reactivation of the hepatitis B or C virus) is possible. Cases of reactivation of the hepatitis B virus after discontinuation of methotrexate have also been described. If it is necessary to prescribe methotrexate to a patient with a history of viral hepatitis, a thorough clinical and laboratory examination should be performed.
The presence of pleural effusion, ascites, gastrointestinal obstruction, concomitant cisplatin therapy, dehydration, impaired liver function or decreased urine pH slows down the elimination of methotrexate, which may result in an increase in its concentration in the blood plasma. It is extremely important to detect the accumulation of methotrexate in the body during the first 48 hours, since the development of irreversible consequences of its toxicity is possible.
Particular caution should be exercised when using methotrexate in elderly patients, and their condition should be monitored more frequently than younger patients for early signs of treatment toxicity.
Pediatric patients with acute lymphoblastic leukemia may develop severe neurotoxicity when using medium (1 g/m2) doses of methotrexate, which most often manifests clinically as a generalized or partial epileptic seizure. The development of leukoencephalopathy and/or microangiospatic calcifications during instrumental studies in such patients has been described.
When using high doses of methotrexate, the development of transient acute neurological symptoms has been described, which can manifest itself incl. changes in behavior, local disturbances of the sensory organs (including short-term blindness) and the motor system, impaired reflexes. The exact reasons for the development of these adverse reactions are unknown.
When using methotrexate at a dose higher than 100 mg/m2, it is necessary to use “rescue therapy” with calcium folinate 42-48 hours after administration of methotrexate. The dose of calcium folinate is determined depending on the size of the dose of methotrexate used and the duration of its infusion.
Methotrexate concentrations should be determined after 24, 48, 72 hours and, if necessary, over a long period of time, to determine the optimal duration of calcium folinate therapy. The use of methotrexate together with red blood cell infusion (within 24 hours) requires careful monitoring of the patient’s condition, as the plasma concentration of methotrexate may increase.
Measures should be taken to prevent methotrexate solutions from coming into contact with the skin and mucous membranes. If methotrexate accidentally comes into contact with the skin or mucous membranes, immediately wash the affected area with plenty of water.
Impact on the ability to drive vehicles and machinery
Due to the potential for side effects of methotrexate, such as drowsiness, headache and confusion, caution should be exercised when engaging in potentially hazardous activities that require increased concentration and psychomotor speed.
If the described adverse events occur, you should refrain from performing these activities.
Active ingredient
Active ingredient
Methotrexate
Composition
Composition
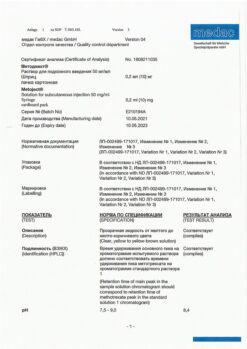
Active substance: methotrexate
Excipients: sodium chloride, sodium hydroxide, water for injection.
Pregnancy
Pregnancy
Methotrexate is contraindicated for use during pregnancy. If necessary, use during lactation should stop breastfeeding.
Women of childbearing potential should use reliable methods of contraception while using methotrexate.
Experimental studies have established the embryotoxic and teratogenic effects of methotrexate.
Contraindications
Contraindications
Hypersensitivity to methotrexate; severe renal failure; severe liver failure; alcohol abuse; a history of hematopoietic system disorders (in particular, bone marrow hypoplasia, leukopenia, thrombocytopenia or clinically significant anemia); immunodeficiency; severe acute and chronic infectious diseases such as tuberculosis and HIV infection; concomitant vaccination with live vaccines; oral ulcers, gastrointestinal ulcers in the active phase; simultaneous use of methotrexate at a dose of ≥15 mg/week. with acetylsalicylic acid; pregnancy; breastfeeding period.
With caution: if patients have impaired liver and kidney function, diabetes mellitus, obesity, previous therapy with hepatotoxic drugs, dehydration, ascites, suppression of bone marrow hematopoiesis, pleural or peritoneal effusion, parasitic and infectious diseases of a viral, fungal or bacterial nature – the risk of developing a severe generalized disease (currently or recently suffered, including recent contact with a patient) – simple herpes, herpes zoster (viremic phase), chicken pox, measles, amebiasis, strongyloidiasis (established or suspected), gout (including a history) or urate nephrourolithiasis (including a history), infection and inflammation of the oral mucosa, vomiting, diarrhea, gastric and duodenal ulcers, ulcerative colitis, obstructive gastrointestinal diseases, previous chemotherapy or radiation therapy, asthenia, aciduria (urine pH less than 7), in children and elderly patients.
Side Effects
Side Effects
From the digestive system: possible ulcerative stomatitis, anorexia, gingivitis, pharyngitis, nausea; rarely – diarrhea, melena, enteritis, pancreatitis; in some cases (with long-term daily use) – liver necrosis, cirrhosis, fatty atrophy, periportal liver fibrosis.
From the hematopoietic system: leukopenia, anemia, thrombocytopenia.
From the side of the central nervous system: feeling of fatigue, dizziness; rarely – headache, aphasia, drowsiness, convulsions.
From the reproductive system: disorders of oogenesis and spermatogenesis, oligospermia, menstrual irregularities, decreased libido, impotence.
From the urinary system: hematuria, cystitis, severe renal dysfunction.
Allergic reactions: chills, decreased resistance to infection; rarely – urticaria, toxic epidermal necrolysis, Stevens-Johnson syndrome.
Dermatological reactions: skin rash, photosensitivity, pigmentation disorders, telangiectasia, acne, furunculosis.
From the cardiovascular system: infrequently – vasculitis; rarely – pericarditis, pericardial effusion, cardiac tamponade, decreased blood pressure, thromboembolic complications (including cerebral vascular thrombosis and arterial thrombosis, thrombophlebitis, deep vein thrombosis, retinal vein thrombosis, pulmonary embolism).
From the blood and lymphatic system: often – leukopenia, thrombocytopenia, anemia; uncommon – pancytopenia, agranulocytosis, hematopoietic disorders; rarely – megaloblastic anemia; very rarely – severe suppression of bone marrow function, aplastic anemia, enlarged lymph nodes, lymphoproliferative diseases (partially reversible), eosinophilia, neutropenia. The first signs of these complications, which are life-threatening, are fever, sore throat, mouth ulcers, flu-like symptoms, nosebleeds and skin hemorrhages. Methotrexate should be stopped immediately if the blood cell count decreases significantly.
From the immune system: uncommon – allergic reactions, anaphylactic shock, immunosuppression.
Infectious diseases: very rarely – sepsis, opportunistic infections (in some cases can be fatal), infections caused by Cytomegalovirus; frequency unknown – cases of nocardiosis, histoplasmosis and cryptococcal fungal infections, disseminated form of herpes simplex have been reported.
From the nervous system: often – headache, increased fatigue, drowsiness; infrequently – depression, confusion, dizziness, convulsions; rarely – mood changes; very rarely – pain, muscle weakness or paresthesia in the extremities, impaired taste (metallic taste), acute aseptic meningitis with meningism (paralysis, vomiting), insomnia; frequency unknown – ringing in the ears.
From the organ of vision: rarely – severe visual impairment; very rarely – conjunctivitis, retinopathy.
Benign, malignant and unspecified neoplasms: uncommon – isolated cases of lymphomas that regress when treatment with methotrexate is stopped.
From the respiratory system: often – pulmonary complications due to interstitial pneumonitis/alveolitis, incl. fatal – regardless of the dose and duration of treatment with methotrexate (typical symptoms: malaise, dry non-productive cough, shortness of breath, progressing to shortness of breath at rest, chest pain, fever. If the above adverse reactions are suspected, the use of methotrexate is stopped immediately, it is necessary to exclude infections, including pneumonia); uncommon – pulmonary fibrosis; rarely – pharyngitis, apnea, bronchial asthma, shortness of breath, abnormal results of instrumental studies of pulmonary function; very rarely – pneumonia caused by Pneumocystis carinii and other lung infections, difficulty breathing, chronic obstructive pulmonary disease, pleural effusion.
From the digestive system: very often – loss of appetite, nausea, vomiting (especially during the first 24-48 hours after administration of methotrexate), abdominal pain, inflammation and ulcers in the mucous membrane of the mouth and throat, stomatitis, dyspepsia; often – diarrhea (especially in the first 24-48 hours after using methotrexate); infrequently – ulcers, bleeding of the gastrointestinal tract; rarely – enteritis, melena, gingivitis, malabsorption syndrome; very rarely – vomiting with blood, toxic megacolon.
From the liver and biliary tract: very often – increased activity of liver enzymes (ALT, AST), increased alkaline phosphatase activity, increased bilirubin concentration; infrequently – hepatic steatosis, liver fibrosis, liver cirrhosis (may appear even if regularly detected when monitoring normal values of liver transaminases); rarely – acute hepatitis and hepatotoxicity; very rarely – reactivation of chronic hepatitis, acute liver dystrophy, liver failure (the most common is hepatitis caused by the herpes simplex virus and accompanied by liver failure).
From the skin and subcutaneous tissues: often – exanthema, erythema, itching; uncommon – urticaria, photosensitivity, increased skin pigmentation, hair loss, abnormal wound healing, enlarged rheumatic nodes, herpes zoster, painful manifestations of psoriatic plaques (exacerbation of plaque psoriasis may occur with UV radiation therapy and simultaneous use of methotrexate), severe toxic reactions, vasculitis, allergic vasculitis, skin rashes herpetiformis, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome); rarely – changes in nail pigmentation, onycholysis, petechiae, ecchymoses, erythema multiforme, erythematous skin rash; very rarely – acute paronychia, furunculosis, telangiectasia, hidradenitis.
From the musculoskeletal system: infrequently – arthralgia, myalgia, osteoporosis; rarely – stress fractures, osteonecrosis.
From the urinary system: infrequently – inflammation and ulceration of the bladder (possibly with hematuria), dysuria; rarely – renal failure, oliguria, anuria, azotemia; very rarely – proteinuria.
From the reproductive system: infrequently – vaginitis; rarely – oligospermia, menstrual irregularities; very rarely – decreased libido, impotence, vaginal discharge, infertility, gynecomastia; frequency unknown – disturbance of oogenesis and spermatogenesis, teratogenic effect.
From the endocrine system: frequency unknown – diabetes mellitus, metabolic disorders.
Local reactions: with intramuscular injection, infrequently – burning or tissue damage (formation of sterile abscesses, destruction of fatty deposits) at the injection site.
Very rare: fever. Generally, methotrexate is well tolerated when administered subcutaneously; to date, only mild local reactions have been reported, which have decreased during treatment.
Other: uncommon – decreased serum albumin concentration, hypogammaglobulinemia; rarely – fever.
The frequency and severity of adverse reactions of methotrexate depend on the dose and frequency of use. Since severe adverse reactions can occur at low doses, it is extremely important that patients undergo medical examination regularly and at short intervals.
Interaction
Interaction
When used simultaneously with vitamin preparations containing folic acid or its derivatives, the effectiveness of methotrexate may be reduced.
The simultaneous use of NSAIDs in high doses can lead to an increase in the concentration of methotrexate in plasma and to a prolongation of its T1/2, as well as an increase in the concentration of methotrexate not bound to plasma albumin, which in turn increases the toxic effects of methotrexate (primarily on the gastrointestinal tract and hematopoietic system).
When used simultaneously with penicillins, methotrexate (even in low doses) may increase its toxic effects.
When used simultaneously with sulfonamides, especially with co-trimoxazole, there is a risk of increased myelosuppressive effects.
When using nitrous oxide in patients receiving methotrexate, severe unpredictable myelodepression and stomatitis may develop.
When used simultaneously with methotrexate, valproic acid may reduce its concentration in the blood plasma.
Cholestyramine binds methotrexate, reduces its enterohepatic recirculation, which leads to a decrease in its concentration in the blood plasma.
When used simultaneously with mercaptopurine, it is possible to increase its bioavailability due to impaired metabolism during the “first pass” through the liver.
Neomycin and paromomycin reduce the absorption of methotrexate from the gastrointestinal tract.
In patients receiving omeprazole, increased plasma concentrations of methotrexate are possible.
When used simultaneously with probenecid, a 3-4-fold increase in the concentration of methotrexate in the blood plasma is possible due to a decrease in its renal excretion.
When methotrexate is used concomitantly with retinoids, the risk of hepatotoxicity may increase.
Salicylates potentiate the effect of methotrexate due to a decrease in its renal excretion.
After a course of treatment with tetracycline, methotrexate, used even in low doses, can have a toxic effect.
With sequential administration of methotrexate and fluorouracil, synergistic action is possible; fluorouracil administered before methotrexate may reduce its toxicity.
Cisplatin is nephrotoxic and may therefore reduce the renal excretion of methotrexate, resulting in increased toxicity.
The likelihood of hepatotoxicity from methotrexate increases with regular alcohol consumption and concomitant use of other hepatotoxic drugs.
With combination therapy of methotrexate and leflunomide, the incidence of pancytopenia and hepatotoxic effects increases.
There may be increased toxicity when using cyclosporine in patients receiving methotrexate.
The simultaneous use of indirect anticoagulants and lipid-lowering drugs (colestyramine) increases the toxicity of methotrexate.
During treatment with methotrexate, you should avoid excessive consumption of drinks containing caffeine and theophylline (coffee, sweet drinks containing caffeine, black tea).
Methotrexate reduces the clearance of theophylline.
Methotrexate should not be mixed with other drugs or solvents.
Manufacturer
Manufacturer
Oncotech Pharma Production GmbH, Germany
Additional information
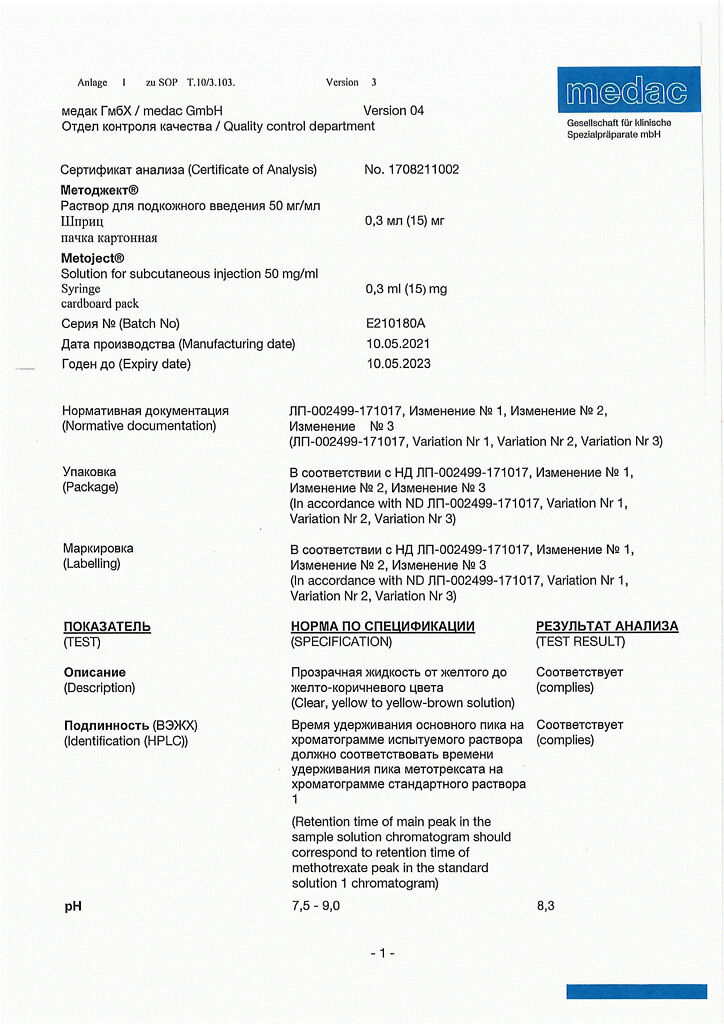
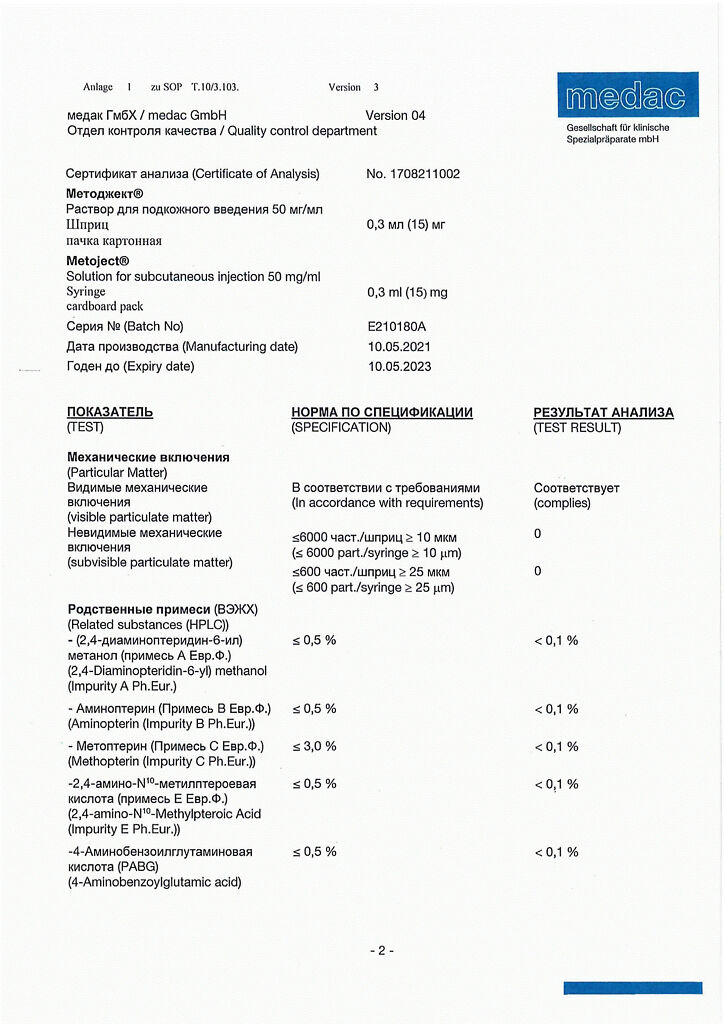
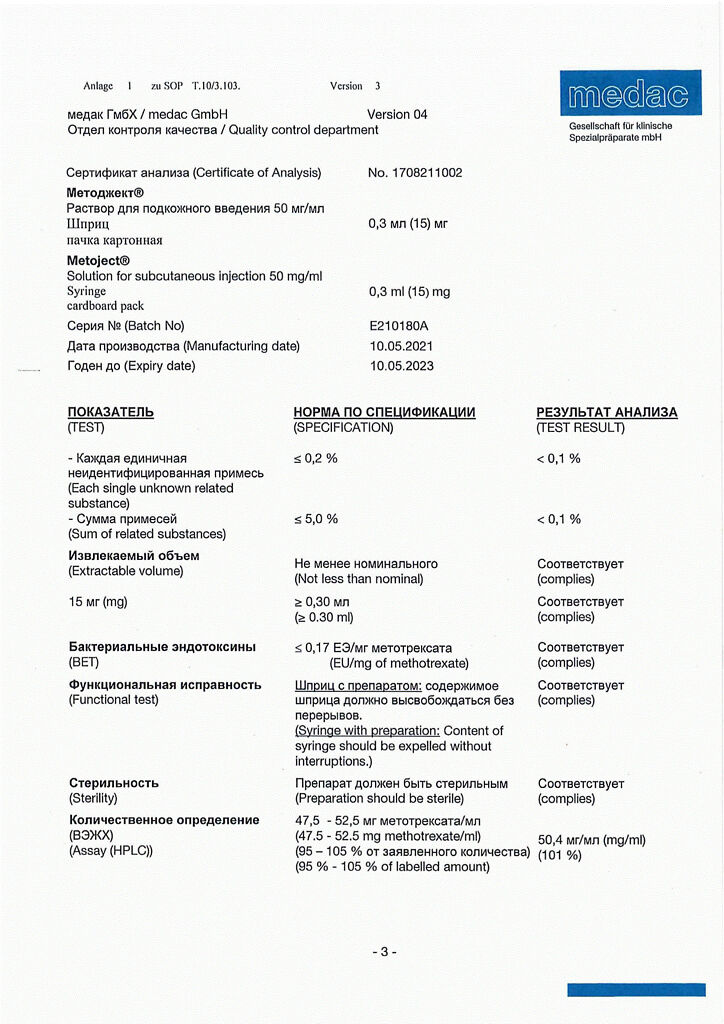
| Manufacturer | Onkotek Pharma Production GmbH, Germany |
|---|---|
| Medication form | suspension |
| Brand | Onkotek Pharma Production GmbH |
Other forms…
Related products
Buy Metoject, 50 mg/ml suspension 0.3 ml with delivery to USA, UK, Europe and over 120 other countries.