No products in the cart.
Metoclopramide, 5 mg/ml 2 ml 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: Antiemetic agent – dopamine receptor blocker central
Code: ATXA03FA
Pharmacodynamics:
The specific blocker of dopamine (D2) and serotonin (5-HT3) receptors inhibits brainstem trigger zone chemoreceptors attenuates sensitivity of visceral nerves transmitting impulses from the stomach and duodenal gatekeeper to the vomiting center.
Through the hypothalamus and the parasympathetic nervous system (innervation of the gastrointestinal tract) it has a regulatory and coordinating effect on the tone and motor activity of the upper gastrointestinal tract (including the tone of the lower esophageal sphincter).
Enhances gastric and intestinal tone accelerates gastric emptying reduces hyperacidic stasis prevents pyloric and esophageal reflux stimulates intestinal peristalsis. Normalizes the separation of bile reduces spasm of the sphincter of Oddi.
Without changing its tone, it eliminates gallbladder dyskinesia. It does not influence the tone of blood vessels in the brain, blood pressure, respiratory function as well as kidney and liver blood formation, secretion of the stomach and pancreas.
Stimulates the secretion of prolactin. Increases tissue sensitivity to acetylcholine (action is independent of vagus innervation but is eliminated by choline blockers). By stimulating aldosterone secretion it increases retention of sodium ions and excretion of potassium ions.
The onset of action on the gastrointestinal tract is noted 1-3 minutes after intravenous administration 10-15 minutes after intramuscular administration and is manifested by accelerated evacuation of gastric contents (approximately from 05-6 hours depending on the route of administration) and antiemetic effect (lasts 12 hours).
Pharmacokinetics:
Indications
Indications
Adults
Prevention of postoperative nausea and vomiting.
Symptomatic treatment of nausea and vomiting including acute migraine. Prevention of nausea and vomiting caused by radiation therapy and chemotherapy.
To enhance peristalsis during gastrointestinal x-ray examinations.
Children
A second-line treatment for postoperative nausea and vomiting.
The second-line prevention of delayed chemotherapy-induced nausea and vomiting.
Active ingredient
Active ingredient
Composition
Composition
Active ingredient:
Metoclopramide hydrochloride monohydrate (in terms of metoclopramide hydrochloride) – 5.0 mg
Auxiliary substances: Anhydrous sodium sulfite, sodium chloride, dihydrate dihydrate (salt of diatrium ethylenediamine-N,N,N’,N’-tetraacetic acid 2-water, (trilon B)), water for injection.
How to take, the dosage
How to take, the dosage
Intravenously or intramuscularly.
Intravenous injections should be given bolus slowly (at least 3 minutes).
Adults
Prevention of postoperative nausea and vomiting
The recommended single dose is 10 mg (1 ampoule).
The second line of treatment for postoperative nausea and vomiting. Second-line prevention of delayed chemotherapy-induced nausea and vomiting
The recommended single dose is 10 mg (1 ampoule) administered up to three times daily.
To enhance peristalsis during gastrointestinal x-ray examinations. As a means to facilitate duodenal probing (to speed up gastric emptying and food movement through the small intestine)
Intravenous bolus slow (at least 3 min) administration of 10-20 mg (1-2 ampoules) 10 min before the study is recommended.
The maximum recommended daily dose is 30 mg or 05 mg/kg.
The period of administration of the drug as an injection should be as short as possible, followed by transition to an oral or rectal dosage form.
Children 1 to 18 years of age
The second-line treatment of postoperative nausea and vomiting. Second-line prevention of delayed chemotherapy-induced nausea and vomiting
The intravenous bolus slow (at least 3 minutes) injection of 01 -015 mg/kg up to 3 times daily is recommended.
The maximum daily dose is 05 mg/kg/day.
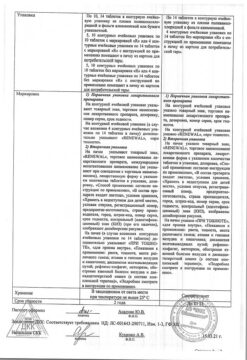
Dosing regimen
Age (years)
Body weight (kg)
Dose (mg)
Frequency
1-3
10-14
1
Up to 3 times a day
/p>
3-5
15-19
2
Up to 3 times a day
5-9
20-29
25
9-18
30-60
5
td>
Up to 3 times a day
15-18
Over 60
10
Up to 3 times a day
To enhance peristalsis during gastrointestinal x-ray examinations. As a means to facilitate duodenal probing (to speed up gastric emptying and food movement through the small intestine)
In children over 15 years of age
A slow bolus of 10-20 mg (1-2 ampoules) intravenously (at least 3 min) 10 min before the examination is recommended.
In children aged 1 to 15 years
A slow (at least 3 min) intravenous bolus injection of 01 mg/kg at 10 min before the study is recommended.
The maximum duration of treatment to prevent postoperative nausea and vomiting is 48 hours.
The maximum duration of treatment for prevention of nausea and vomiting caused by chemotherapy is 5 days.
In order to avoid overdose, a minimum interval of 6 hours between administration should be observed, even in cases of vomiting.
Elderly patients
The dose may need to be reduced in elderly patients due to decreased renal and hepatic function.
Renal failure
In patients with end-stage renal failure (CK less than 15 mL/min), the daily dose should be reduced by 75%.
In patients with moderate to severe renal failure (CKD 15-60 ml/min), the dose should be reduced by 50%.
Hepatic impairment
In patients with severe hepatic impairment, the dose should be reduced by 50%.
Interaction
Interaction
The concomitant use of metoclopramide with levodopa or dopamine receptor agonists is contraindicated due to mutual antagonism.
Alcohol increases the sedative effect of metoclopramide.
Combinations requiring caution
Because of the prokinetic effect of metoclopramide, absorption of some drugs may be impaired.
M-cholinoblockers and morphine derivatives are mutually antagonistic to metoclopramide with respect to effects on gastrointestinal peristalsis. CNS depressant drugs (morphine derivatives tranquilizers H1-histamine receptor blockers antidepressants with sedative effect barbiturates clonidine and other drugs of these groups) can increase sedative effect under the influence of metoclopramide.
Metoclopramide increases the effect of neuroleptics with respect to extrapyramidal symptoms.
In concomitant use of oral metoclopramide and tetrabenazine there is potential for dopamine deficiency which may be accompanied by increased muscle rigidity or muscle spasm with difficulty in speaking or swallowing restlessness tremor involuntary muscle movements including facial muscles.
The use of metoclopramide with serogoninergic drugs such as selective serotonin reuptake inhibitors increases the risk of serotonin syndrome (serotonin intoxication).
Methoclopramide reduces the bioavailability of digoxin. Plasma concentrations of digoxin should be monitored.
Methoclopramide increases the bioavailability of cyclosporine (Cmax by 46 % and exposure by 22 %). Plasma concentrations of cyclosporine should be monitored carefully. The clinical consequences of this interaction have not been established.
The exposure of metoclopramide is increased when used concomitantly with potent CYP2D6 isoenzyme inhibitors such as fluoxetine and paroxetine. Although the clinical significance of such an interaction has not been established, the occurrence of adverse reactions in patients should be monitored.
The concomitant use of metoclopramide with atovachone significantly decreases plasma concentrations of atovachone (approximately 50%). Concomitant use of metoclopramide with atovachone is not recommended.
The concomitant use of metoclopramide with bromocriptine increases the plasma concentration of bromocriptine.
Metoclopramide increases absorption of tetracycline from the small intestine. Metoclopramide enhances absorption of mexiletine and lithium.
Metoclopramide decreases absorption of cimetidine.
Special Instructions
Special Instructions
Caution should be exercised when using metoclopramide in elderly patients.
Nervous system disorders may occur especially in children and young patients and/or when using high doses, usually at the beginning of treatment or after a single use.
The drug should be discontinued immediately if extrapyramidal symptoms occur. Reactions are completely reversible after discontinuation of treatment, but may require symptomatic therapy (benzodiazepines in children and/or anticholinergic anti-Parkinsonian drugs in adults).
In order to avoid an overdose of the drug, a minimum interval of 6 hours between injections of the drug should be observed, even in cases of vomiting.
Long treatment with the drug may lead to the development of tardive dyskinesia potentially irreversible especially in elderly patients. The duration of treatment should not exceed 3 months due to the risk of development of tardive dyskinesia. If there are signs of tardive dyskinesia the treatment should be discontinued.
When using metoclopramide concomitantly with neuroleptics as well as during monotherapy with metoclopramide a neuroleptic malignant syndrome is observed. It is necessary to stop treatment with the drug immediately if symptoms of neuroleptic malignant syndrome appear, and concomitant therapy should be applied.
Cautions are necessary when using in patients with underlying neurologic diseases and in patients taking medications that affect the central nervous system.
Symptoms of Parkinson’s disease may also be noted with use of the drug. There have been reported cases of methemoglobinemia caused by NADN-dependent cytochrome-b5 reductase deficiency. In this case, the use of the drug should be immediately and completely discontinued and appropriate measures should be taken.
Severe cardiovascular adverse events have been reported, including vascular failure, marked bradycardia, cardiac arrest, and prolonged QT interval.
Perhaps caution should be exercised when using in elderly patients with cardiac abnormalities (including prolonged QT interval), patients with poor electrolyte balance, bradycardia, and patients on medications extending the QT interval.
In patients with moderate to severe renal impairment and severe hepatic impairment, reduction of the dose is recommended (see section “Dosage and administration”).
Contraindications
Contraindications
– Hypersensitivity to metoclopramide and drug components;
– gastrointestinal bleeding mechanical intestinal obstruction or perforation of the gastrointestinal wall of states in which stimulation of gastrointestinal peristalsis is a risk;
– confirmed or suspected pheochromocytoma due to risk of severe arterial hypertension;
– tardive dyskinesia that developed after a history of treatment with neuroleptics or metoclopramide;
– epilepsy (increased frequency and severity of seizures); Parkinson’s disease;
– concomitant use with levodopa and dopamine receptor agonists;
– methemoglobinemia due to metoclopramide or a history of cytochrome b5 nicotinamide adenine dinucleotide (NADN) deficiency;
– prolactinoma or prolactin-dependent tumor;
– childhood age less than 1 year;
– period of breastfeeding.
Side effects
Side effects
The incidence of adverse reactions is given according to WHO classification: very common (⥠1/10) common (⥠1/100 – < 1/10) infrequent (⥠1/1000 – < 1/100) rare (⥠1/10000 – < 1/1000) very rare (< 1/10000).
Blood and lymphatic system disorders: frequency unknown – methemoglobinemia probably associated with NADN-dependent cytochrome-b5 reductase enzyme deficiency (especially in infants) sulfhemoglobinemia (most often with simultaneous use of high doses of sulfur-containing drugs) leukopenia neutropenia. agranulocytosis.
The immune system: infrequent hypersensitivity; frequency unknown – anaphylactic reactions (including anaphylactic shock) allergic reactions (urticaria maculopapular rash).
Endocrine system: infrequent – amenorrhea hyperprolactinemia; rarely – galactorrhea; frequency unknown – gynecomastia.
Endocrine disorders during prolonged treatment are associated with hyperprolactinemia (amenorrhea galactorrhea gynecomastia).
Psychiatric disorders: often – depression; infrequently – hallucinations; rarely – confusion.
Nervous system disorders: very common – somnolence; common – asthenia extrapyramidal disorders (especially in children and young patients and/or when exceeding recommended doses of the drug even after a single administration); parkinsonism akathisia; infrequent – dystonia dyskinesia impaired consciousness; rare – convulsions (especially in patients with epilepsy); frequency unknown – late dyskinesia sometimes persistent during or after long-term treatment (especially in older patients) neuroleptic malignant syndrome.
Heart: infrequent bradycardia; frequency unknown – cardiac arrest which may be caused by bradycardia atrioventricular block sinus node blockade prolongation of QT interval on electrocardiogram “pirouette” arrhythmia.
Vascular disorders: often – decreased blood pressure; frequency unknown – cardiogenic shock acute increase of blood pressure in patients with pheochromocytoma.
Gastrointestinal tract: frequent – constipation diarrhea nausea.
Renal and urinary tract disorders: frequency unknown – polyuria urinary incontinence.
Genital and mammary system disorders: frequency unknown – sexual dysfunction priapism.
Unwanted reactions most common with high doses of the drug: extrapyramidal symptoms: acute dystonia and dyskinesia parkinsonian syndrome akathisia developed even after a single dose of the drug especially in children and young patients (see section “Special Precautions”); drowsiness decreased level of consciousness confusion hallucinations.
Overdose
Overdose
Symptoms
Extrapyramidal disorders somnolence decreased level of consciousness confusion hallucinations irritability dizziness bradycardia changes in blood pressure cardiac and respiratory arrest abdominal pain.
Treatment
In case of development of extrapyramidal symptoms caused by overdose or other reason, treatment is symptomatic only (benzodiazepines in children and/or anticholinergic antiparkinsonian drugs in adults). Symptomatic treatment and continuous monitoring of cardiovascular and respiratory function is required, depending on the clinical condition of the patient.
There is no specific antidote.
Pregnancy use
Pregnancy use
Pregnancy
Metoclopramide may be used during pregnancy (1-11 trimesters) only if the potential benefit to the mother exceeds the potential risk to the fetus.
Because of the pharmacological characteristics (similar to other neuroleptics) when using metoclopramide in late pregnancy, the possibility of extrapyramidal symptoms in the neonate cannot be ruled out. Metoclopramide should not be used in late pregnancy (during the third trimester). When using metoclopramide, the condition of the newborn should be monitored.
Breast-feeding period
Metoclopramide is excreted in small amounts with the breast milk. The possibility of adverse reactions in the child cannot be excluded. The use of metoclopramide during breastfeeding is contraindicated. If it is necessary to use the drug during lactation, breastfeeding should be stopped.
Similarities
Similarities
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 ° C. Store out of the reach of children. |
| Manufacturer | Ozon, Russia |
| Medication form | solution |
| Brand | Ozon |
Other forms…
Related products
Buy Metoclopramide, 5 mg/ml 2 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.