No products in the cart.
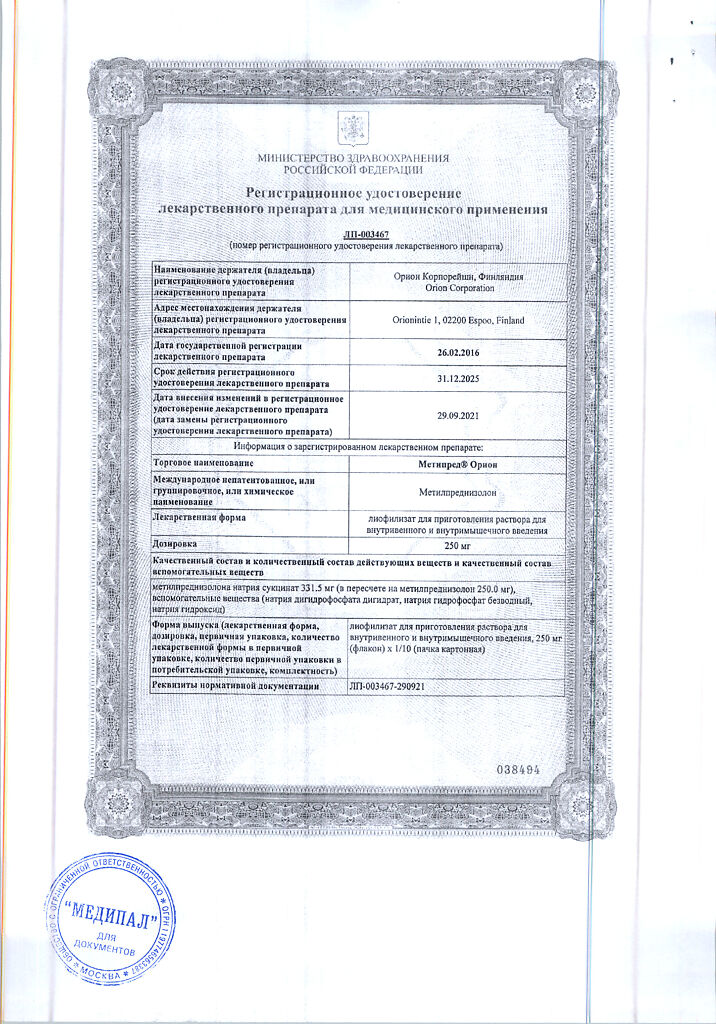
Metipred Orion, lyophilizate 250 mg
€1.00
Out of stock
(E-mail when Stock is available)
Description
METIPRED is a synthetic GCS. It has anti-inflammatory, anti-allergic, immunosuppressive effect, increases sensitivity of beta-adrenoreceptors to endogenous catecholamines.
Interacts with specific cytoplasmic receptors (receptors for GCS are in all tissues, especially in liver) with the formation of complex, inducing protein formation (including enzymes regulating vital processes in cells).
Effects of methylprednisolone on protein metabolism: reduces the number of globulins in the plasma, increases the synthesis of albumins in the liver and kidneys (with an increase in the ratio albumin/globulin), reduces synthesis and increases catabolism of protein in muscle tissue.
Effects of methylprednisolone on lipid metabolism: increases the synthesis of higher fatty acids and triglycerides, redistributes fat (fat accumulation occurs primarily in the shoulder girdle, face and abdomen), leads to hypercholesterolemia.
Impact of methylprednisolone on carbohydrate metabolism: increases absorption of carbohydrates from gastrointestinal tract, increases activity of glucose-6-phosphatase (increases glucose flow from liver into blood), increases activity of phosphoenolpyruvate carboxylase and synthesis of aminotransferases (activates gluconeogenesis), promotes hyperglycemia.
Effect of methylprednisolone on water-electrolyte metabolism: it retains sodium and water in the body, stimulates potassium excretion (mineralocorticoid activity), reduces absorption of calcium from the gastrointestinal tract, reduces bone mineralization.
Anti-inflammatory activity is associated with inhibition of release of inflammatory mediators by eosinophils and mast cells, induction of lipocortin formation and reduction in number of mast cells producing hyaluronic acid, reduction of capillary permeability, stabilization of cell membranes (especially lysosomal) and organelle membranes. It acts on all stages of the inflammatory process: it inhibits the synthesis of prostaglandins at the level of arachidonic acid (lipokortin inhibits phospholipase A2, inhibits arachidonic acid liberation and inhibits the biosynthesis of endoperoxides, leukotrienes, contributing, among others, to the inflammatory processes.Inhibits the synthesis of pro-inflammatory cytokines (including interleukin 1, tumor necrosis factor alpha), increases resistance of cell membrane to the action of various damaging factors.
Immunosuppressive effect is caused by involution of lymphoid tissue, inhibition of lymphocyte proliferation (especially T-lymphocytes), suppression of B-cell migration and interaction between T- and B-lymphocytes, inhibition of cytokine release (interleukin-1, 2, interferon gamma) from lymphocytes and macrophages and reduction of antibody formation.
Antianallergic action results from reduction of synthesis and secretion of allergy mediators, inhibition of histamine and other bioactive substances release from sensitized mast cells and basophils, reduction of circulating basophils, T- and B-lymphocytes, mast cells number, suppression of lymphoid and connective tissue development, reduction of effector cells sensitivity to allergy mediators, suppression of antibody formation, change in the body immune response.
In obstructive respiratory tract diseases the action is mainly caused by inhibition of inflammatory processes, prevention or reduction of mucous membrane edema, decrease of eosinophilic infiltration of submucous layer of bronchial epithelium and deposition of circulating immune complexes in bronchial mucosa, and also inhibition of erosion and mucosa desquamation. It increases sensitivity of small and medium caliber bronchial beta-adrenoreceptors to endogenous catecholamines and exogenous sympathomimetics, decreases mucus viscosity by reducing its production.
Inhibits the synthesis and secretion of ACTH and secondary – the synthesis of endogenous GCS.
Inhibits connective tissue reactions during the inflammatory process and reduces the possibility of scar tissue formation.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
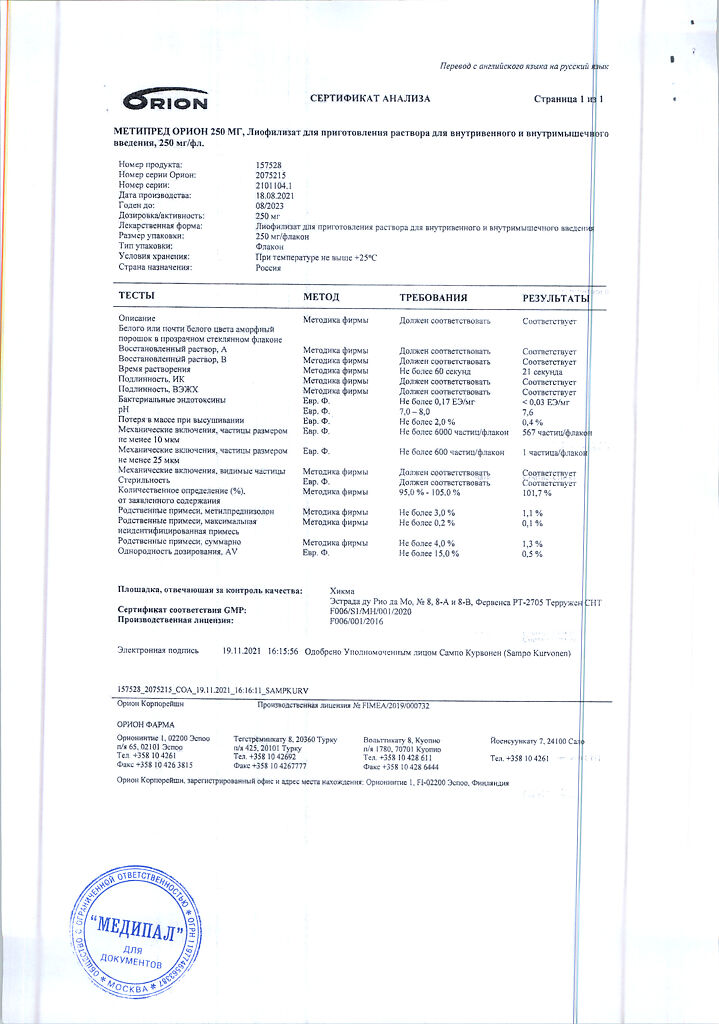
1 vial contains:
The active ingredient:
methylprednisolone sodium succinate (in terms of methylprednisolone) 250 mg;
Auxiliary substance:
sodium hydroxide – 12.5 mg;
Solvent:
water for injection.
How to take, the dosage
How to take, the dosage
V/v (as slow trickle injections or infusions), i.m.
Preparation of the solution. Solution for injection is prepared by adding the solvent to the bottle with lyophilizate just before use. The prepared solution contains 62.5 mg/ml of methylprednisolone.
As additional therapy for life-threatening conditions, 30 mg/kg is administered by IV for at least 30 minutes. This dose may be repeated every 4-6 hours for not more than 48 hours.
Pulse therapy in the treatment of diseases in which GCS therapy is effective, in exacerbations of the disease and/or when standard therapy is ineffective.
Recommended therapy regimens
Rheumatic diseases. 1 g/day v/v for 1-4 days or 1 g/month v/v for 6 months.
Systemic lupus erythematosus. 1 g/day v/v for 3 days.
Multiple sclerosis. 1 g/day v/v for 3 or 5 days.
Oedematous conditions (e.g., glomerulonephritis, lupus nephritis). 30 mg/kg v/v/day for 4 days or 1 g/day for 3, 5, or 7 days.
The above doses should be given for at least 30 minutes, and may be repeated if there is no improvement within a week of treatment or if the patient’s condition requires it.
Oncological diseases in the terminal stage (to improve quality of life). 125 mg/d by IV daily for up to 8 weeks.
Prevention of nausea and vomiting associated with chemotherapy for cancer. In chemotherapy characterized by mild to moderate vomiting, administer 250 mg v/v for at least 5 min for 1 h before administration of the chemotherapeutic drug, at the beginning of chemotherapy, and after its completion. In chemotherapy characterized by a pronounced vomiting effect, administer 250 mg w/in for at least 5 minutes in combination with appropriate doses of metoclopramide or butyrophenone 1 hour before administration of the chemotherapeutic agent, then 250 mg w/in at the beginning of chemotherapy and after its completion.
In other indications, the initial dose is 10-500 mg by IV depending on the nature of the disease. For a short course in severe acute conditions, higher doses may be required. The initial dose not exceeding 250 mg should be administered by IV for at least 5 minutes, doses over 250 mg administered for at least 30 minutes. Subsequent doses are administered by IV or IM, with the length of intervals between doses depending on the patient’s response to therapy and on their clinical condition.
Lower doses (but at least 0.5 mg/kg/day) should be given in children, but the patient’s severity and response to therapy should be the primary consideration when choosing a dose, not age or body weight.
Interaction
Interaction
Simultaneous administration of methylprednisolone:
Special Instructions
Special Instructions
Prepared solution for parenteral administration should be stored at 15° to 20°C and used within 12 h. If the prepared solution is stored in the refrigerator at 2° to 8°C, it can be used within 24 hours.
During treatment with Metipred (especially long-term) it is necessary to monitor the ophthalmologist, BP, water-electrolyte balance, as well as peripheral blood picture and blood glucose concentration.
In order to reduce side effects, antacids may be prescribed, and the intake of potassium into the body may be increased (diet, potassium preparations). Food should be rich in proteins and vitamins, with a restriction of fat, carbohydrates and table salt.
The action of the drug is increased in patients with hypothyroidism and cirrhosis. The drug may aggravate existing emotional instability or psychotic disorders. If a history of psychosis is indicated, Metipred in high doses is prescribed under strict medical supervision.
With caution, use in acute and subacute myocardial infarction due to the possibility of spreading the focus of necrosis, delayed formation of scar tissue and rupture of the heart muscle.
In stressful situations during maintenance treatment (including surgery, trauma, infectious diseases), the drug dose should be adjusted due to increased need for GCS.
In case of abrupt withdrawal, especially if high doses were previously used, withdrawal syndrome (anorexia, nausea, lethargy, generalized musculoskeletal pain, generalized weakness) and exacerbation of the disease for which Metipred was prescribed may occur.
Vaccination should not be performed during treatment with Metipred, because of decreased immune response and, therefore, decreased effectiveness of the vaccine.
When prescribing Metipred for intercurrent infections, septic conditions and tuberculosis, bactericidal antibiotics must be treated at the same time.
In children during long-term treatment with Metipred it is necessary to monitor closely the dynamics of growth and development. Children who have been in contact with patients with measles or chickenpox during treatment are prescribed specific immunoglobulins prophylactically.
Because of the weak mineralocorticoid effect for replacement therapy in adrenal insufficiency Metipred is used in combination with mineralocorticoids.
In patients with diabetes mellitus, blood glucose concentrations should be monitored and the dose of hypoglycemic agents should be adjusted if necessary.
The radiological monitoring of the bone and joint system (images of the spine, hand) is indicated.
Methypred in patients with latent renal and urinary tract infections may cause leukocyturia, which may be of diagnostic value.
Methypred increases metabolites of 11- and 17-oxyketocorticosteroids.
Contraindications
Contraindications
The only contraindication for short-term use for vital signs is hypersensitivity to methylprednisolone or components of the drug.
In children during growth, GCS should be used only for absolute indications and under close medical supervision.
The drug should be prescribed with caution in the following diseases and conditions:
Side effects
Side effects
Endocrine system disorders: decreased glucose tolerance, steroid diabetes mellitus, manifestation of latent diabetes mellitus, depressed adrenal function, Icenko-Cushing’s syndrome (moon-shaped face, pituitary obesity, hirsutism, increased BP, dysmenorrhea, amenorrhea, muscle weakness, stretch marks), delayed sexual development in children.
Digestive system disorders: nausea, vomiting, pancreatitis, steroid gastric and duodenal ulcer, erosive esophagitis, gastrointestinal bleeding, perforation of the gastrointestinal wall, appetite disorders, digestive disorders, flatulence, hiccups; rarely – increased activity of liver transaminases and ALP.
Cardiovascular system disorders: arrhythmias, bradycardia (up to cardiac arrest); in predisposed patients, development or worsening of the severity of heart failure, ECG changes characteristic of hypokalemia, increased BP, hypercoagulation, thrombosis; in patients with acute and subacute myocardial infarction, spread of necrosis focus, slow formation of scar tissue, which can lead to rupture of the heart muscle may occur.
CNS and peripheral nervous system disorders: delirium, disorientation, euphoria, hallucinations, manic-depressive psychosis, depression, paranoia, increased intracranial pressure, nervousness, anxiety, insomnia, dizziness, vertigo, cerebellar pseudotumor, headache, seizures.
Senses: posterior subcapsular cataract, increased intraocular pressure with possible damage to the optic nerve, tendency to develop secondary bacterial, fungal or viral eye infections, trophic changes of the cornea, exophthalmos, sudden vision loss (when parenteral administration in the head, neck, nasal cavities, scalp crystals may deposit the drug in the vessels of the eye).
Metabolism disorders: increased calcium excretion, hypocalcemia, increased body weight, negative nitrogen balance (increased protein breakdown), increased sweating; due to mineralocorticoid activity – fluid and sodium retention (peripheral edema), hypernatremia, hypokalemic syndrome (hypokalemia, arrhythmia, myalgia or muscle spasm, unusual weakness and fatigue).
Muscular system disorders: growth retardation and ossification processes in children (premature closure of epiphyseal growth zones), osteoporosis (very rare – pathological bone fractures, aseptic necrosis of the humeral and femoral head), rupture of muscle tendons, steroid myopathy, reduction of muscle mass (atrophy).
Dermatological reactions: delayed wound healing, petechiae, ecchymoses, skin thinning, hyper- or hypopigmentation, steroid acne, stretch marks, tendency to develop pyoderma and candidiasis.
Allergic reactions: skin rash, itching, anaphylactic shock, local allergic reactions.
Local reactions when parenteral administration: burning, numbness, pain, tingling at the injection site, infection of the injection site; necrosis of surrounding tissues, scar formation at the injection site, skin and subcutaneous tissue atrophy in case of injection (injection into the deltoid muscle is especially dangerous).
Others: development or exacerbation of infections (the appearance of this side effect is promoted by co-administration of immunosuppressants and vaccination), leukocyturia, withdrawal syndrome, “flushes” of blood to the head.
Overdose
Overdose
Similarities
Similarities
Additional information
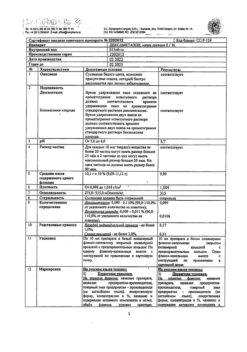
| Shelf life | 5 years |
|---|---|
| Conditions of storage | In a light-protected place at 15-25 °C |
| Manufacturer | Hikma Pharmaceutica (Portugal) S.A., Portugal |
| Medication form | lyophilizate |
| Brand | Hikma Pharmaceutica (Portugal) S.A. |
Other forms…
Related products
Buy Metipred Orion, lyophilizate 250 mg with delivery to USA, UK, Europe and over 120 other countries.