No products in the cart.
Description Pharmacotherapeutic group: ATX: Pharmacodynamics: Pharmacokinetics:
Antitumor agent, antimetabolite
L.01.B.A Folic acid analogues
L.01.B.A.01 Methotrexate
Antitumor drug from the group of antimetabolite analogues of folic acid. Along with antitumor, it has immunosuppressive action.
Inhibits dihydrofolate reductase, which is involved in the reduction of dihydrofolic acid to tetrahydrofolic acid – the carrier of carbon fragments necessary for the synthesis of purine nucleotides and their derivatives.
Inhibits synthesis, DNA repair and cellular mitosis (in S-phase). Tissues with high cell proliferation are especially sensitive to the action of methotrexate: tumor tissue, bone marrow, mucosal epithelial cells, embryonic cells.
. The mechanism of action in rheumatoid arthritis is connected with immunomodulatory and anti-inflammatory action of the preparation and caused by the induction of apoptosis of the rapidly proliferating cells (activated T-lymphocytes, fibroblasts, synoviocytes), Inhibition of synthesis of anti-inflammatory cytokines IL-1 (Interleukin 1), TNF-α (Tumor necrosis factor alpha), enhancement of synthesis of anti-inflammatory cytokines IL-4 (Interleukin 4), IL-10 (Interleukin 10) and suppression of metalloproteinases activity.
In patients with rheumatoid arthritis, methotrexate reduces symptoms of inflammation (pain, swelling, stiffness), but there are limited studies on the long-term use of methotrexate (regarding the ability to maintain remission in rheumatoid arthritis).
The growth rate of keratinocytes in psoriatic plaques is increased in psoriasis compared to normal skin cell proliferation. This difference in cell proliferation is the basis for the use of methotrexate to treat psoriasis.
Absorption and distribution
When administered in m/m, the Cmax of methotrexate in plasma is reached within 30-60 min. Wide interindividual variability ranging from 1 to 3 h is characteristic of patients with leukemia.
The relative bioavailability in patients with rheumatoid arthritis is comparable with intramuscular and subcutaneous administration of the same dose of the drug. Systemic absorption of methotrexate after injection under the skin of the abdomen and thigh is the same.
After intravenous administration, the primary distribution is 0.18 L/kg (18% of body weight). The saturation dose distribution is about 0.4-0.8 L/kg (40% to 80% of body weight).
Binding to plasma proteins is about 50%, mostly to albumin. Competitive displacement is possible in concomitant use with sulphonamides, salicylates, tetracyclines, chloramphenicol, phenytoin.
When taken in therapeutic doses, methotrexate does not penetrate the blood-brain barrier.
Methotrexate undergoes hepatic and intracellular metabolism to form the pharmacologically active polyglutamine form, which also inhibits dihydrofolate reductase and thymidine synthesis.
A small amount of polyglutamate methotrexate can remain in tissues for long periods of time. Retention and prolongation of the action of active metabolites of the drug varies depending on the type of cells, tissues and tumors.
About 10% of injected methotrexate is metabolized in the liver. The main metabolite is 7-hydroxymethotrexate.
The mean T1/2 values when using methotrexate at a dose of less than 30 mg/m2 are 6-7 hours. In patients receiving high doses of methotrexate, the T1/2 is 8 to 17 hours.
80 to 90% of the dose received is eliminated unchanged by glomerular filtration and tubular secretion within 24 hours. Approximately 5-20% of methotrexate and 1-5% of 7-hydromethotrexate are excreted with bile with subsequent reabsorption in the intestine.
Pharmacokinetics in special clinical cases
In chronic renal failure both phases of drug excretion may be significantly prolonged.
Disordered renal function, marked ascites or pleural effusion, and concomitant use of drugs such as weak organic acids, which also undergo tubular secretion, can significantly increase the serum concentration of methotrexate.
According to the distribution, methotrexate is cumulated in the liver, kidney and spleen as polyglutamates and may be retained in these organs for several weeks or months.
.
Indications
Indications
Rheumatoid arthritis in adults;
polyarthritis form of juvenile idiopathic arthritis in case of insufficient therapeutic response to therapy with non-steroidal anti-inflammatory drugs (NSAIDs);
severe psoriasis in adult patients, especially in the form of plaques, in case of ineffectiveness of standard therapy, including phototherapy, PUVA therapy and the use of retinoids;
severe form of psoriatic arthritis in adult patients.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group:
Antitumor agent, antimetabolite
ATX:
L.01.B.A Folic acid analogues
L.01.B.A.01 Methotrexate
Pharmacodynamics:
An antitumor drug from the group of antimetabolites of folic acid analogues. Along with antitumor, it has an immunosuppressive effect.
Inhibits dihydrofolate reductase, which is involved in the reduction of dihydrofolic acid to tetrahydrofolic acid – a transporter of carbon fragments necessary for the synthesis of purine nucleotides and their derivatives.
Inhibits DNA synthesis, repair and cell mitosis (in S-phase). Tissues with high cell proliferation are especially sensitive to the action of methotrexate: tumor tissue, bone marrow, epithelial cells of the mucous membranes, embryonic cells.
The mechanism of action in rheumatoid arthritis is associated with the immunomodulatory and anti-inflammatory effect of the drug and is caused by the induction of apoptosis of rapidly proliferating cells (activated T-lymphocytes, fibroblasts, synoviocytes), inhibition of the synthesis of anti-inflammatory cytokines IL-1 (Interleukin 1), TNF-α (Tumor Necrosis Factor alpha)), increased synthesis of anti-inflammatory cytokines IL-4 (Interleukin 4), IL-10 (Interleukin 10) and suppression of metalloproteinase activity.
In patients with rheumatoid arthritis, the use of methotrexate reduces symptoms of inflammation (pain, swelling, stiffness), but there is limited research on long-term use of methotrexate (regarding the ability to maintain remission in rheumatoid arthritis).
In psoriasis, the growth rate of keratinocytes in psoriatic plaques increases compared to the normal proliferation of skin cells. This difference in cell proliferation is the basis for the use of methotrexate to treat psoriasis.
Pharmacokinetics:
Suction and distribution
With intramuscular administration, Cmax of methotrexate in blood plasma is achieved within 30-60 minutes. Patients with leukemia are characterized by wide interindividual variability ranging from 1 to 3 hours.
Relative bioavailability in patients with rheumatoid arthritis is comparable with intramuscular and subcutaneous administration of the same dose of the drug. Systemic absorption of methotrexate after injection under the skin of the abdomen and thigh is the same.
After intravenous administration, the primary distribution is 0.18 l/kg (18% of body weight). The saturation dose distribution is about 0.4-0.8 l/kg (40%-80% of body weight).
Plasma protein binding is about 50%, mainly with albumin. Competitive displacement is possible when used simultaneously with sulfonamides, salicylates, tetracyclines, chloramphenicol, phenytoin.
When taken in therapeutic doses, methotrexate does not penetrate the blood-brain barrier.
Metabolism
Methotrexate undergoes hepatic and intracellular metabolism to form a pharmacologically active polyglutamine form, which also inhibits dihydrofolate reductase and thymidine synthesis.
Small amounts of methotrexate polyglutamate may remain in tissues for a long period of time. The persistence and prolongation of action of the active metabolites of the drug vary depending on the type of cells, tissues and tumors.
Approximately 10% of administered methotrexate is metabolized in the liver. The main metabolite is 7-hydroxymethotrexate.
Removal
The average T1/2 values when using methotrexate at a dose of less than 30 mg/m2 are 6-7 hours. In patients receiving high doses of methotrexate, T1/2 ranges from 8 to 17 hours.
From 80 to 90% of the received dose is excreted unchanged by glomerular filtration and tubular secretion within 24 hours. Approximately 5-20% of methotrexate and 1-5% of 7-hydromethotrexate are excreted in the bile, followed by reabsorption in the intestine.
Pharmacokinetics in special clinical situations
In chronic renal failure, both phases of drug elimination can be significantly prolonged.
Impaired renal function, severe ascites or pleural effusion, as well as concomitant use of drugs such as weak organic acids, which also undergo tubular secretion, can significantly increase the concentration of methotrexate in the blood serum.
In accordance with the distribution, methotrexate accumulates in the liver, kidneys and spleen in the form of polyglutamates and can remain in these organs for several weeks or months.
Special instructions
Special instructions
If a significant amount of fluid in the pleural cavities or ascites is detected in a patient, the fluid should be evacuated by drainage before starting methotrexate therapy, or the use of methotrexate should be discontinued.
The appearance of symptoms of toxic damage to the digestive system, the earliest of which are stomatitis and diarrhea, requires temporary cessation of methotrexate therapy due to the high risk of developing hemorrhagic enteritis and intestinal perforation with a fatal outcome if therapy is continued. During treatment with methotrexate
Patients should be closely monitored for signs of possible toxicity and adverse effects. Given the risk of severe or even fatal toxic reactions, patients should be thoroughly informed about possible complications and recommended precautions.
Before starting treatment with methotrexate or when resuming therapy after a break, it is necessary to conduct a clinical blood test with counting the leukocyte formula and platelet count, assess the activity of liver enzymes, the concentration of bilirubin, serum albumin, as well as a chest x-ray and renal function tests.
If there are clinical indications, studies are prescribed to exclude tuberculosis and hepatitis.
During treatment with methotrexate (monthly in the first 6 months and at least every 3 months thereafter, and as doses increase, it is advisable to increase the frequency of examinations), the following studies are carried out:
1. Examination of the mouth and throat to identify changes in the mucous membranes.
2. Blood test to determine the leukocyte formula and platelet count.
Even when used in normal therapeutic doses, methotrexate can suddenly cause depression of the hematopoietic system. If there is a significant decrease in the number of leukocytes or platelets, treatment with methotrexate is stopped immediately and symptomatic supportive therapy is prescribed.
Patients should be instructed to immediately report any signs and symptoms indicating an infection to their physician. During concomitant therapy with hematotoxic drugs (for example, leflunomide), it is necessary to carefully monitor the number of leukocytes and platelets in the blood.
During long-term treatment with methotrexate, if necessary, a bone marrow biopsy is advisable.
3. Functional “liver” tests.
Particular attention should be paid to identifying signs of liver damage. Treatment with methotrexate should not be started or should be suspended if any abnormal results of liver function tests or liver biopsy are detected.
Typically, the indicators return to normal within two weeks, after which treatment can be resumed according to the doctor’s decision.
In 13 – 20% of patients, a short-term increase of 2 – 3 times in the activity of liver enzymes was observed. A persistent increase in liver enzyme activity and/or a decrease in serum albumin concentrations may be indicators of severe hepatotoxicity.
Enzyme diagnostics do not in all cases provide adequate prediction of the development of hepatotoxicity detected morphologically; even in the case of normal values of the activity of “liver” enzymes, liver fibrosis, or, much less commonly, liver cirrhosis, can be detected histopathologically.
When using methotrexate for rheumatological indications, there is no reason to perform a liver biopsy to monitor the hepatotoxic effect of the drug.
When treating patients with psoriasis, it is necessary to evaluate the advisability of performing a liver biopsy before or during treatment with methotrexate, based on current scientific recommendations. If biochemical liver function tests or type III collagen propeptide concentrations do not reveal signs of hepatotoxicity, additional studies may be necessary.
Such an assessment should differentiate between patients without risk factors and patients at risk (for example, with a history of alcohol abuse, with persistently elevated liver enzymes, a history of liver disease, a family history of hereditary liver disease, patients with diabetes mellitus, obese patients, as well as previous use of hepatotoxic drugs or contact with hepatotoxic chemicals and receiving long-term treatment with methotrexate in total doses of 1.5 g or more).
In case of persistent increase in the activity of liver enzymes, it is necessary to reduce the dose or stop treatment with methotrexate.
Since methotrexate has a toxic effect on the liver, other hepatotoxic drugs should not be prescribed during treatment with the drug unless clearly necessary.
You should also avoid or greatly reduce your alcohol consumption. The activity of liver enzymes should be especially carefully monitored in patients receiving concomitant therapy with other hepatotoxic and hematotoxic drugs (in particular, leflunomide).
Particular caution should be observed when treating patients with insulin-dependent diabetes mellitus, since cases of the development of liver cirrhosis have been described with a previous periodic increase in the activity of liver enzymes.
4. Renal function tests and urine examination.
If the serum creatinine concentration increases, the dose of methotrextate should be reduced. At creatinine concentration. exceeding 2 mg/dL, the use of methotrexate is contraindicated.
Since methotrexate is excreted primarily by the kidneys, patients with impaired renal function may experience increased concentrations of methotrexate in the blood, which may result in severe adverse reactions. It is necessary to carefully monitor the condition of patients who may have impaired renal function (for example, elderly patients).
This is especially important in the case of concomitant therapy with drugs that reduce the excretion of methotrexate, have an adverse effect on the kidneys (in particular, NSAIDs) or on the hematopoietic system. If there are risk factors such as renal failure. simultaneous use of non-steroidal anti-inflammatory drugs is not recommended.
Dehydration may also potentiate the toxic effects of methotrexate.
5. Study of respiratory function
systems. It is necessary to closely monitor symptoms of possible development of pulmonary function disorders and, if necessary, order a pulmonary function test.
Pulmonary diseases require rapid diagnosis and discontinuation of methotrexate. The appearance of corresponding symptoms (especially a dry, nonproductive cough) or the development of nonspecific pneumonitis during treatment with methotrexate may indicate a potential danger of lung damage. In such cases, methotrexate is discontinued and the patient is carefully examined.
Although the clinical presentation may vary, the typical patient with methotrexate-induced pulmonary disease exhibits fever, cough with dyspnea, hypoxemia, and pulmonary infiltrates on x-ray. In the differential diagnosis, infectious diseases should be excluded. Lung damage can occur during treatment with methotrexate at any dose.
During treatment with methotrexate, opportunistic infections may develop, including pneumonia caused by Pneumocystis carinii, which can be fatal. If the patient exhibits symptoms of pulmonary involvement, pneumonia caused by Pneumocystis carinii should be excluded.
Caution is recommended when treating patients with pulmonary insufficiency.
6. Because methotrexate affects the immune system, it may alter the response to vaccinations and affect the results of immunological tests.
Particular caution is required when treating patients with inactive, chronic infections (such as herpes zoster, tuberculosis, hepatitis B or C) due to their possible activation. During treatment with methotrexate, vaccination with live vaccines should not be performed.
It is recommended that methotrexate treatment be interrupted one week before surgery and restarted one or two weeks after surgery.
When body temperature rises (more than 38°C), the elimination of methotrexate slows down significantly.
Methotrexate may increase the risk of developing neoplasms (mainly lymphomas). Malignant lymphomas can also develop in patients receiving low-dose methotrexate. In such cases, the drug is discontinued. If spontaneous regression of lymphoma is not observed, therapy with cytotoxic drugs is prescribed.
Before starting treatment with Methortritis, pregnancy must be excluded. Methotrexate has an embryotoxic effect, promotes abortion and the formation of fetal development abnormalities.
Methotrexate therapy is accompanied by inhibition of spermatogenesis and oogenesis, which can lead to decreased fertility. After discontinuation of methotrexate therapy, these effects spontaneously regress. During methotrexate therapy and for 6 months after its completion, patients are recommended to use contraception.
Patients of reproductive age, as well as their partners, should be informed about the possible effect of methotrexate on reproduction and fetal development.
During therapy with high doses, precipitation of methotrexate or its metabolites in the renal tubules may occur. In such cases, to prevent this complication, it is recommended to carry out infusion therapy and alkalization of urine until a pH of 6.5-7.0 is achieved through oral or intravenous administration of sodium bicarbonate (5 tablets of 625 mg every 3 hours) or acetazolamide (500 mg orally 4 times a day).
Methotrexate should not be mixed with other medications in the same infusion bag or vial.
When handling methotrexate solution, you must follow the rules for handling cytotoxic substances. Pregnant healthcare workers should not work with the drug.
Measures should be taken to prevent the solution from entering
methotrexate on the skin and mucous membranes. If the drug does get on the skin or mucous membranes, the affected area is immediately washed with plenty of water.
Impact on the ability to drive vehicles. Wed and fur.:
During treatment with Methortritis, you should refrain from driving vehicles or operating other machinery, as side effects from the nervous system (fatigue and dizziness) may occur.
Active ingredient
Active ingredient
Methotrexate
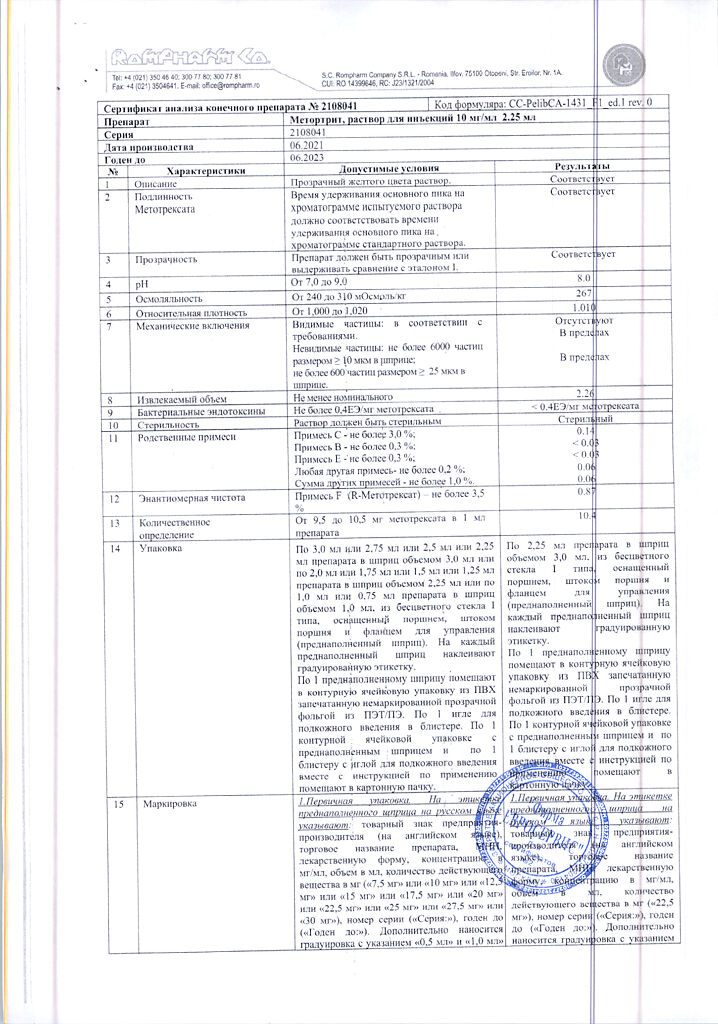
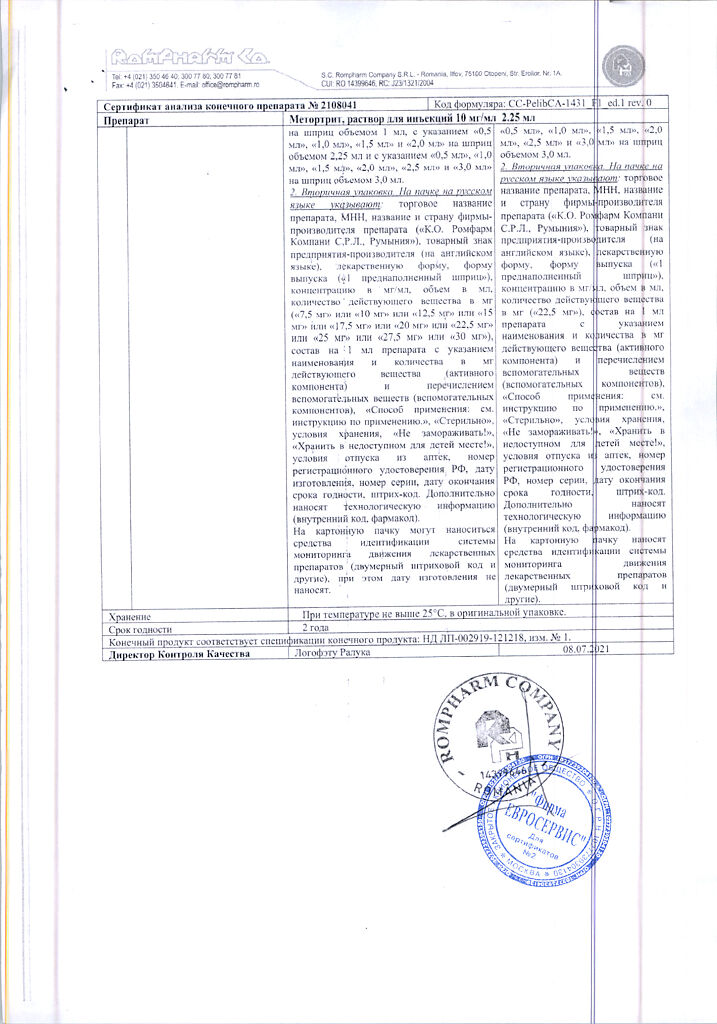
Composition
Composition
For 1 ml of the drug:
active ingredient: methotrexate disodium 10.97 mg in terms of methotrexate 10.00 mg;
auxiliary components:
sodium chloride – 7.00 mg;
2 M sodium hydroxide solution – 1.76 mg (22 µl);
1 M sodium hydroxide solution – up to pH = 8.5 ± 0.1;
water for injection – up to 1.00 ml.
Pregnancy
Pregnancy
Pregnancy
Methotrexate is contraindicated during pregnancy.
Taking methotrexate during pregnancy can cause serious fetal malformations (a 14-fold increase in the incidence of malformations of the skull, cardiovascular system and limbs).
If pregnancy occurs during treatment with methotrexate, it is necessary to consult with specialists regarding the risk of adverse effects of methotrexate on the fetus.
Fertility
Patients of reproductive age (women and men) should use effective contraception during and for at least 6 months after treatment with Methortrit.
Breastfeeding
Methotrexate passes into breast milk in concentrations that are harmful to the baby. Therefore, during treatment with methotrexate, breastfeeding should be stopped.
Contraindications
Contraindications
Hypersensitivity to methotrexate and/or to any other component of the drug;
severe renal failure (creatinine clearance <20 ml/min);
severe liver failure;
alcohol abuse;
a history of hematopoietic system disorders (in particular, bone marrow hypoplasia, leukopenia, thrombocytopenia or clinically significant anemia);
immunodeficiency;
severe acute and chronic infectious diseases such as tuberculosis and HIV infection;
concomitant vaccination with live vaccines;
oral ulcers, gastrointestinal ulcers in the active phase;
simultaneous use of methotrexate at a dose of ≥ 15 mg/week. with acetylsalicylic acid;
pregnancy;
breastfeeding period.
With caution:
The drug should be used with caution if the patient has impaired liver and kidney function, diabetes mellitus, obesity and previous exposure to hepatotoxic drugs, dehydration, suppression of bone marrow hematopoiesis, pleural or peritoneal effusion, parasitic and infectious diseases of viral, fungal or bacterial etiology (currently or recently suffered, including recent contact with a sick person), incl. such as herpes simplex, herpes zoster (viremic form), chickenpox, measles, amoebiasis, strongyloidiasis (established or suspected) due to the risk of developing a severe generalized disease; gout (including a history) or uric nephrourolithiasis (including a history), infection and inflammation of the oral mucosa, vomiting, diarrhea, gastric and duodenal ulcers, ulcerative colitis, obstructive gastrointestinal diseases, previous chemotherapy or radiation therapy, asthenia, aciduria (urine pH less than 7), as well as in children and elderly patients.
Side Effects
Side Effects
In accordance with the WHO classification, undesirable effects are classified according to their frequency of development as follows: very often (≥ 1/10), often (from ≥1/100 to < 1/10), infrequently (from ≥1/1000 to < 1/100), rarely (from ≥1/10,000 to < 1/1000), very rarely (< 1/10 000); frequency unknown - based on available data, it was not possible to determine the frequency of occurrence.
Disorders of the cardiovascular system.
Uncommon: vasculitis (as acute toxic symptoms).
Rarely: pericarditis, pericardial effusion, cardiac tamponade, decreased blood pressure, thromboembolic complications (including cerebral vascular thrombosis and arterial thrombosis, thrombophlebitis, deep vein thrombosis, retinal vein thrombosis, pulmonary embolism).
Blood and lymphatic system disorders:
Common: leukopenia, thrombocytopenia, anemia.
Uncommon: pancytopenia, agranulocytosis, hematopoietic disorders.
Rare: megaloblastic anemia.
Very rare: severe bone marrow suppression, aplastic anemia, enlarged lymph nodes, lymphoproliferative diseases (partially reversible), eosinophilia, neutropenia.
The first signs of these complications, which are life-threatening, are fever, sore throat, mouth ulcers, flu-like symptoms, nosebleeds and skin hemorrhages. Methotrexate should be stopped immediately if the blood cell count decreases significantly.
Immune system disorders:
Uncommon: allergic reactions, anaphylactic shock, immunosuppression.
Infectious and parasitic diseases:
Very rare: sepsis, opportunistic infections (in some cases can be fatal), infections caused by Cytomegalovirus.
Frequency unknown: cases of nocardiosis, histoplasmosis and cryptococcal fungal infections, a disseminated form of herpes simplex, have been reported.
Nervous system disorders:
Common: headache, fatigue, drowsiness.
Uncommon: depression, confusion, dizziness, convulsions.
Rare: mood changes.
Very rare: pain, muscle weakness or paresthesia in the extremities, impaired taste (metallic taste), acute aseptic meningitis with meningism (paralysis, vomiting), insomnia.
Frequency unknown: tinnitus.
Visual disorders:
Rare: severe visual impairment.
Very rare: conjunctivitis, retinopathy.
Benign, malignant and unspecified neoplasms:
Uncommon: isolated cases of lymphomas that
regress when treatment with methotrexate is stopped. A recent clinical trial did not find that methotrexate therapy increased the incidence of lymphoma.
Disorders of the respiratory system, chest and mediastinal organs:
Common: pulmonary complications due to interstitial pneumonitis/alveolitis, including fatal (regardless of the dose and duration of treatment with methotrexate). Typical symptoms: malaise, dry non-productive cough, shortness of breath. progressing to shortness of breath at rest, chest pain, fever.
If such complications are suspected, methotrexate should be stopped immediately and infections (including pneumonia) excluded.
Uncommon: pulmonary fibrosis.
Rarely: pharyngitis, apnea, bronchial asthma, shortness of breath and abnormal results of instrumental pulmonary function tests.
Very rare: pneumonia caused by Pneumocystis carinii and other lung infections, difficulty breathing, chronic obstructive pulmonary disease, pleural effusion.
Gastrointestinal disorders:
Very common: decreased appetite, nausea and vomiting (especially during the first 24-48 hours after administration of methotrexate), abdominal pain, inflammation and ulcers in the mucous membrane of the mouth and throat, stomatitis, dyspepsia.
Common: diarrhea (especially in the first 24-48 hours after using methotrexate).
Uncommon: ulcers and bleeding of the gastrointestinal tract.
Rarely: enteritis, melena, gingivitis, malabsorption syndrome.
Very rare: vomiting blood, toxic megacolon.
Disorders of the liver and biliary tract:
Very often: increased activity of liver enzymes (ALT, AST), increased alkaline phosphatase activity, increased bilirubin concentration.
Uncommon: hepatic steatosis, liver fibrosis, liver cirrhosis (may appear even if regularly detected when monitoring normal values of “liver” transaminases).
Rare: acute hepatitis and hepatotoxicity.
Very rare: reactivation of chronic hepatitis, acute liver dystrophy, liver failure. The most common hepatitis is caused by the herpes simplex virus and is accompanied by liver failure.
Disorders of the skin and subcutaneous tissues:
Common: exanthema, erythema, itching.
Uncommon: urticaria, photosensitivity, increased skin pigmentation, hair loss, abnormal wound healing, enlarged rheumatic nodes, herpes zoster, painful lesions of psoriatic plaques (exacerbation of plaque psoriasis may occur with UV therapy and concomitant use of methotrexate), severe toxic reactions, vasculitis, allergic vasculitis, skin rashes herpetiformis, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome).
Rarely: changes in nail pigmentation, onycholysis, petechiae, ecchymoses, erythema multiforme, erythematous skin rash.
Very rare: acute paronychia, furunculosis, telangiectasia, hidradenitis.
Musculoskeletal and connective tissue disorders:
Uncommon: arthralgia, myalgia, osteoporosis.
Rarely: stress fractures, osteonecrosis.
Renal and urinary tract disorders:
Uncommon: inflammation and ulceration of the bladder, (possibly with
hematuria), dysuria (urination disorder).
Rarely: renal failure, oliguria, anuria, azotemia.
Very rare: proteinuria.
Disorders of the genital organs and breast:
Uncommon: vaginitis (inflammation of the vagina)
Rarely: oligospermia, menstrual irregularities.
Very rare: decreased libido, impotence, vaginal discharge, infertility, gynecomastia.
Frequency unknown: disturbance of oogenesis and spermatogenesis, teratogenic effect.
Endocrine system disorders:
Frequency unknown: diabetes mellitus, metabolic disorders.
General disorders and disorders at the injection site:
Uncommon: with intramuscular administration of methotrexate – burning or tissue damage (formation of sterile abscesses, destruction of fat deposits) at the injection site.
Very rare: fever. Generally, methotrexate is well tolerated when administered subcutaneously; to date, only mild local reactions have been observed, which have decreased during treatment.
Laboratory and instrumental data:
Uncommon: Decreased serum albumin concentration, hypogammaglobulinemia. The frequency and severity of adverse reactions depend on the dose and frequency of use.
Since severe adverse reactions can occur at low doses, it is extremely important that patients undergo medical examination regularly and at short intervals.
Interaction
Interaction
The likelihood of hepatotoxicity from methotrexate increases with regular alcohol consumption and concomitant use of other hepatotoxic drugs.
With combination therapy with methotrexate and leflunomide, the incidence of pancytopenia and hepatotoxic effects increases.
Oral antibiotics (tetracyclines, chloramphenicol and non-absorbable broad-spectrum antibiotics) may reduce the absorption of methotrexate from the gastrointestinal tract and interfere with the enterohepatic circulation due to inhibition of intestinal microflora or suppression of bacterial metabolism.
Penicillins, ciprofloxation. cephalothin, glycopeptides can reduce the renal clearance of methotrexate, as a result of which its concentration in the blood serum may increase and the toxic effect on the hematopoietic system and gastrointestinal tract may increase.
Probenecid, weak organic acids (for example, loop diuretics) and pyrazoles (phenylbutazone) may slow down the elimination of methotrexate, which may result in increased serum concentrations and increased hematological toxicity.
The risk of toxic effects of methotrexate increases in case of combined use with NSAIDs or salicylates (reduced excretion of methotrexate by the renal tubules is possible; caution should be exercised when combining non-steroidal anti-inflammatory drugs with methotrexate).
When concomitant therapy with drugs that may have an adverse effect on the bone marrow (for example, sulfonamides, trimethoprim/sulfamethoxazole, chloramphenicol, pyrimethaminum), the possibility of developing more severe hematological disorders should be taken into account.
With concomitant therapy with drugs that cause folate deficiency (for example, trimethoprim/sulfamethoxazole), the toxic effect of methotrexate may be enhanced.
The simultaneous use of indirect anticoagulants and lipid-lowering drugs (cholestyramia) increases the toxicity of methotrexate.
With the combined use of antirheumatic drugs (for example, gold salts, penicillamines, hydroxychloroquines, azathioprines, cyclosporim) and methotrexate, the toxic effect of the latter is not enhanced. In the case of simultaneous use of sulfasalazine and methotrexate, the effect of the latter may be potentiated due to inhibition of folic acid synthesis.
When methotrexate is co-administered with proton pump inhibitors (e.g. omeprazole or pantoprazole), the renal elimination of methotrexate may be delayed and pantoprazole may inhibit the renal elimination of the 7-hydroxymethotrexate metabolite, which in one case was accompanied by the development of myalgia and tremor.
During treatment with methotrexate, excessive consumption of drinks containing caffeine and theophylline (coffee, sweet drinks containing caffeine, black tea) should be avoided. Methotrexate reduces the clearance of theophylline.
It is necessary to take into account the pharmacokinetic interaction between methotrexate and flucloxacillin and anticonvulsants (the concentration of methotrexate in the blood decreases), 5-fluorouracil (the half-life of 5-fluorouracil increases).
When used together with other cytostatics, the clearance of methotrexate may be reduced.
Concomitant use of vitamin supplements or oral iron supplements containing folic acid may weaken the response to therapy and reduce the toxic effect of methotrexate on the bone marrow.
When mixing solutions of methotrexate with chlorpromazine hydrochloride, droperidol, idarubicin, metoclopramide hydrochloride, heparin, prednisolone sodium phosphate and promethazine hydrochloride, precipitation or turbidity of the solution may occur.
The use of drugs with additive hematotoxic effects (eg, metamizole) increases the likelihood of serious hematotoxic effects of methotrexate.
Due to competitive binding to serum albumin, with simultaneous use of methotrexate with salicylates, pheylbutazone, phenytoin, barbiturates, tranquilizers, oral contraceptives, tetracycline and amidopyrine derivatives, sulfonamides and p-aminobenzoic acid, the toxicity of methotrexate may be increased.
Several patients with psoriasis or mycosis fungoides treated with methotrexate in combination with PUVA therapy (methoxsalen and ultraviolet radiation) have been diagnosed with skin cancer.
Caution should be exercised when administering packed red blood cells and methotrexate simultaneously.
Combination with radiotherapy may increase the risk of soft tissue necrosis. Methotrexate may reduce the immunological response to vaccination. When administered simultaneously with a live vaccine, severe antigenic reactions may develop.
L-asparaginase is an antagonist of methotrexate.
Anesthesia using dinitrogen oxide can lead to the development of unpredictable severe myelosuppression and stomatitis. Amiodarone may promote skin ulceration.
Pharmaceutical incompatibility
Methortrit should not be mixed with other medications or solvents.
Overdose
Overdose
Symptoms: the most commonly observed symptoms are those associated with inhibition of the hematopoietic system.
Treatment: the specific antidote for methotrexate is calcium folinate. It neutralizes adverse toxic effects.
In case of accidental overdose, no later than an hour after the administration of methotrexate, administer calcium folinate (IV or IM) in a dose equal to or higher than the dose of methotrexate. The administration of calcium folinate is continued until the concentration of methotrexate in the blood serum decreases below the level of 10-7 mmol/l.
In case of significant overdose, rehydration of the body and alkalinization of urine (pH more than 7) may be required to prevent precipitation of methotrexate and/or its metabolites in the renal tubules. Hemodialysis and peritoneal dialysis do not improve the elimination of methotrexate.
Intensive intermittent hemodialysis using high-flux dialyzers allows effective clearance of methotrexate.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C, in the original packaging.
Keep out of the reach of children!
Do not freeze!
Shelf life
Shelf life
2 years.
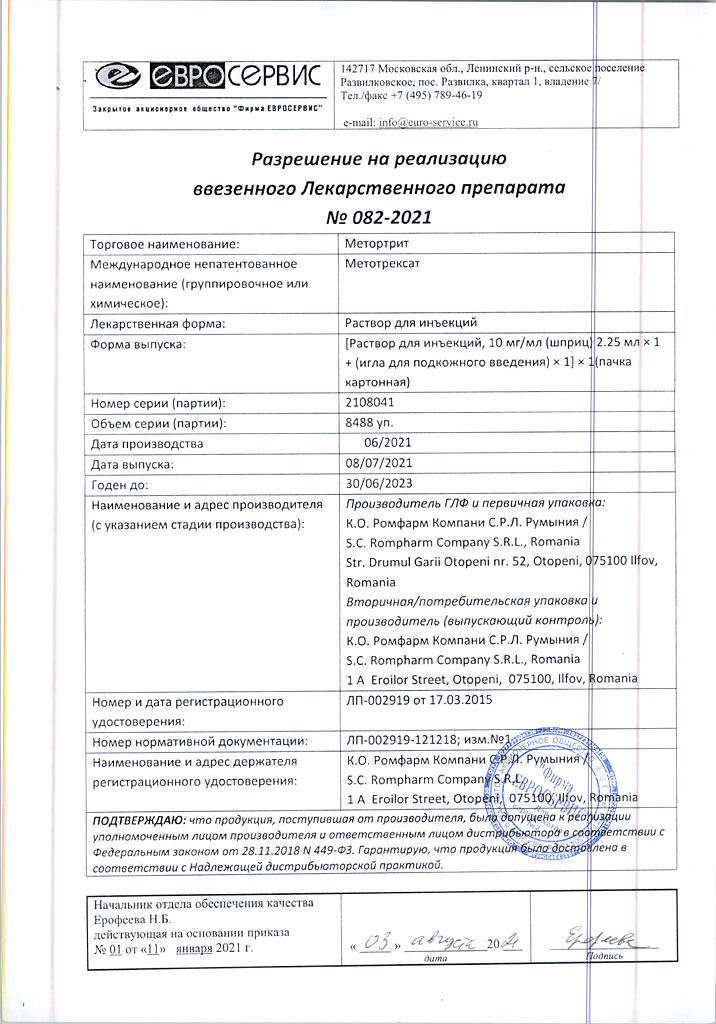
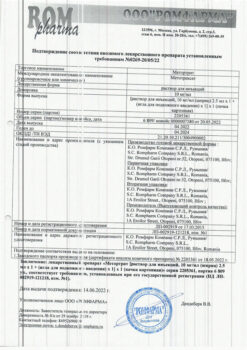
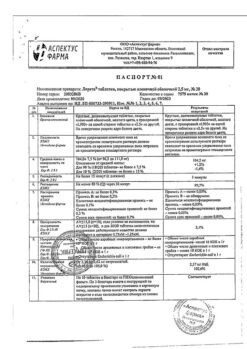
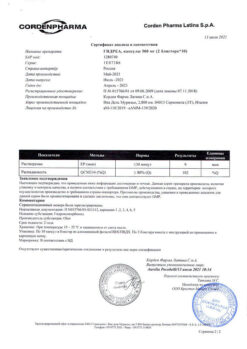
Manufacturer
Manufacturer
K.O.Rompharm Company S.R.L., Romania
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Temperature not exceeding 25°C, in the original package. Store out of the reach of children! Do not freeze! |
| Manufacturer | C.O.Rompharm Company S.R.L., Romania |
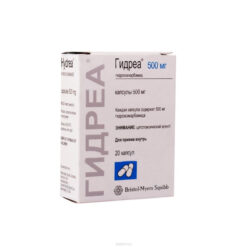
| Medication form | solution for injection |
| Brand | C.O.Rompharm Company S.R.L. |
Other forms…
Related products
Buy Methotrite, 10 mg/ml 2.25 ml with delivery to USA, UK, Europe and over 120 other countries.