No products in the cart.
Description
Cancer
- trophoblastic tumors;
- acute lymphoblastic and myeloblastic leukemia;
- neuroleukemia;
- Non-Hodgkin’s lymphoma, including lymphosarcoma;
- osteogenic sarcoma and soft tissue sarcomas;
- fungal mycosis (advanced stages);
.
Indications
Indications
trophoblastic tumors;
acute lymphoblastic and myeloblastic leukemia;
neuroleukemia;
non-Hodgkin’s lymphomas, including lymphosarcoma;
breast cancer, squamous cell cancer of the head and neck, lung cancer, skin cancer, cervical cancer, vulvar cancer, esophageal cancer, kidney cancer, bladder cancer, testicular cancer, ovarian cancer, penile cancer, retinoblastoma, medulloblastoma;
osteogenic sarcoma and soft tissue sarcomas;
mycosis fungoides (advanced stages);
severe forms of psoriasis, psoriatic arthritis, rheumatoid arthritis, dermatomyositis, SLE, ankylosing spondylitis (if standard therapy is ineffective).
Special instructions
Special instructions
Caution should be exercised when using methotrexate.
Dosage forms containing preservatives (benzyl alcohol) cannot be used for intrathecal administration and for high-dose therapy.
When administering high doses of methotrexate, careful monitoring of the patient is necessary for early detection of the first signs of toxic reactions.
High-dose therapy should be carried out only by experienced chemotherapists who can monitor the concentration of methotrexate in the blood plasma in hospital conditions under the cover of calcium folinate.
During therapy with methotrexate in increased and high doses, the pH of the patient’s urine should be monitored: on the day of administration and in the next 2-3 days, the urine reaction should be alkaline. This is achieved by intravenous drip administration of a mixture consisting of 40 ml of 4.2% sodium bicarbonate solution and 400-800 ml of isotonic sodium chloride solution, the day before, on the day of treatment and in the next 2-3 days.
Treatment with methotrexate in increased and high doses should be combined with increased hydration – up to 2 l/day.
Administration of methotrexate at a dose of ≥2 g/m3 should be carried out under the control of its concentration in the blood serum. A decrease in the level of methotrexate in the blood serum 22 hours after administration by 2 times compared to the initial level is considered normal. An increase in creatinine levels by ≥50% of the initial level and/or an increase in bilirubin levels require intensive detoxification therapy.
To treat psoriasis, methotrexate is prescribed only to patients with a severe form of the disease that does not respond to other types of therapy.
To prevent toxicity during treatment with methotrexate, blood tests should be performed periodically (once a week), the content of leukocytes and platelets should be determined, and liver and kidney function tests should be performed.
If diarrhea and ulcerative stomatitis develop, methotrexate therapy should be interrupted to avoid the development of hemorrhagic enteritis and death of the patient due to intestinal perforation.
In patients with impaired liver function, the elimination period of methotrexate is prolonged, so drug therapy should be carried out with extreme caution, with dose reduction.
Renal dysfunction is dose dependent. The risk of impairment is increased in patients with reduced renal function or dehydration, as well as in patients taking other nephrotoxic drugs.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
Some side effects of the drug may negatively affect the ability to drive a car and perform potentially dangerous activities that require increased concentration and speed of psychomotor reactions.
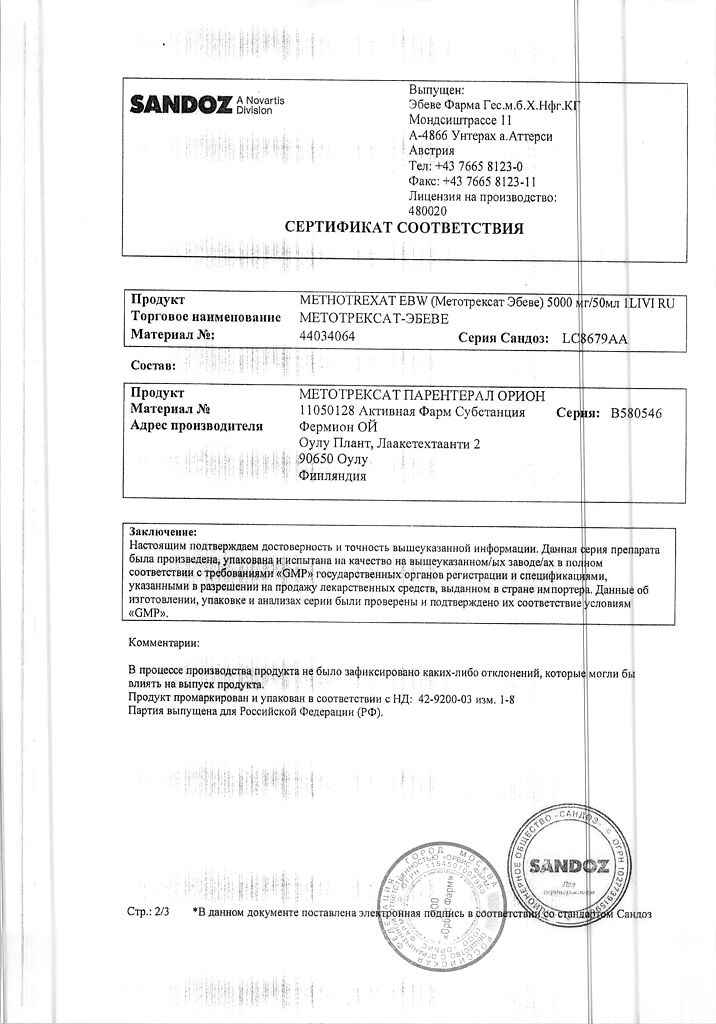
Active ingredient
Active ingredient
Methotrexate
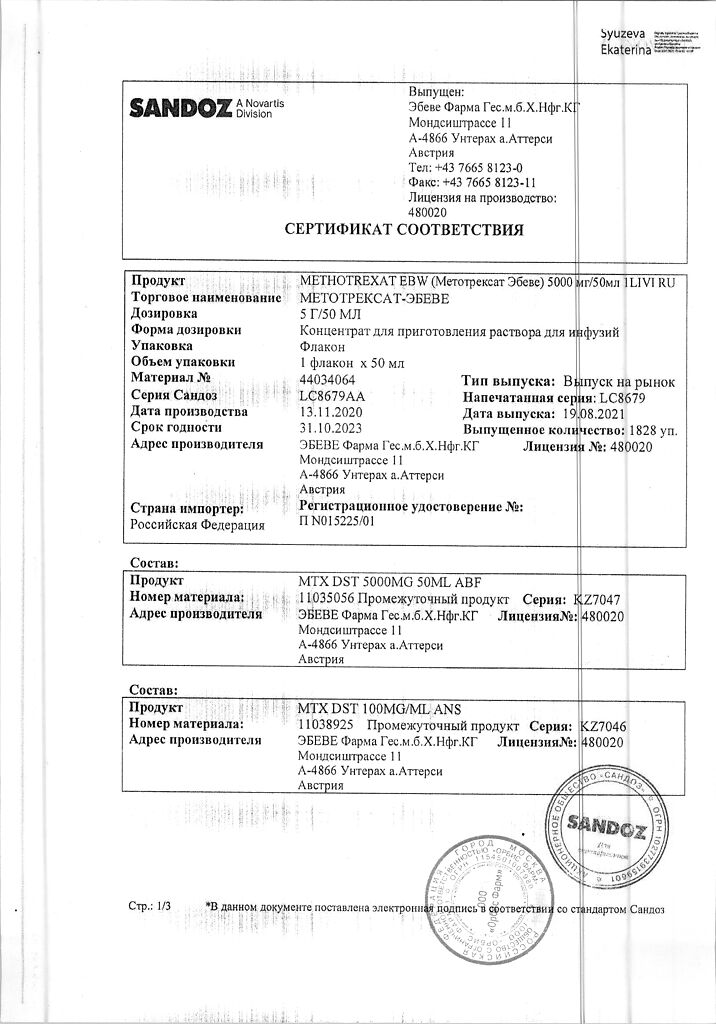
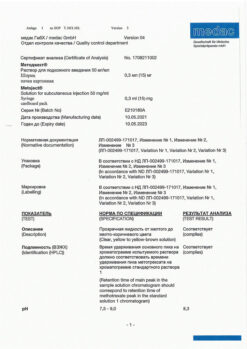
Composition
Composition
1 bottle contains:
Active substance:
methotrexate 5000 mg.
Excipients:
sodium hydroxide – 880.9 mg,
water d/i – 46469.1 mg.
Contraindications
Contraindications
Severe anemia, leukopenia, neutropenia, thrombocytopenia;
renal failure;
liver failure;
pregnancy;
breastfeeding period;
hypersensitivity to methotrexate and/or any other component of the drug.
With caution: the drug should be used for ascites, effusions into the pleural cavity, gastric and duodenal ulcers, ulcerative colitis, dehydration, gout or nephrolithiasis in history, previous radiation therapy or chemotherapy, infectious diseases of a viral, fungal or bacterial nature.
Side Effects
Side Effects
From the hematopoietic system: leukopenia, neutropenia, lymphopenia (especially T-lymphocytes), thrombocytopenia, anemia.
From the digestive system: anorexia, nausea, vomiting, stomatitis, gingivitis, glossitis, pharyngitis; rarely – enteritis, diarrhea, ulcerative lesions of the gastrointestinal tract, gastrointestinal bleeding; in some cases (with long-term daily use) – impaired liver function, increased activity of liver transaminases, periportal fibrosis and cirrhosis of the liver, liver necrosis, fatty liver, pancreatitis.
From the central nervous system and peripheral nervous system: encephalopathy (with the administration of multiple doses intrathecally, radiation therapy in the cranial area), fatigue, weakness, confusion, ataxia, tremor, irritability, convulsions, coma; with intrathecal administration of methotrexate – dizziness, blurred vision, headache, back pain, stiff neck, convulsions, paralysis, hemiparesis.
From the respiratory system: rarely – interstitial pneumonitis, pulmonary fibrosis, exacerbation of pulmonary infections.
From the urinary system: cystitis, nephropathy, renal dysfunction (increased creatinine levels, hematuria).
From the reproductive system: disruption of the process of oogenesis, spermatogenesis, decreased libido/impotence, changes in fertility, teratogenic effects.
From the senses: conjunctivitis, excessive lacrimation, cataracts, photophobia, cortical blindness (when used in high doses), visual impairment.
Dermatological reactions: skin erythema and/or rash, skin itching, telangiectasia, furunculosis, depigmentation or hyperpigmentation, acne, skin peeling, folliculitis, alopecia (rarely), exacerbation of radiation dermatitis.
Allergic reactions: fever, chills, rash, urticaria, anaphylaxis, malignant exudative erythema (Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome), photosensitivity.
Other: immunosuppression (decreased resistance to infectious diseases), malaise, osteoporosis, hyperuricemia, vasculitis, arthralgia/myalgia.
Interaction
Interaction
With the simultaneous use of high doses of methotrexate with various NSAIDs (including aspirin and other salicylates, azapropazone, dichlorfenac, indomethacin and ketoprofen), the toxicity of methotrexate may increase. In some cases, severe toxic effects are possible, sometimes even fatal. Subject to special precautions and appropriate monitoring, the use of methotrexate in low doses (7.5-15 mg per week), particularly in the treatment of rheumatoid arthritis, in combination with NSAIDs is not contraindicated.
When used simultaneously with sulfonamides, sulfonylurea derivatives, phenytoin, phenylbutazone, aminobenzoic acid, probenecid, pyrimethamine or trimethoprim, a number of antibiotics (including penicillin, tetracycline, chloramphenicol), indirect anticoagulants and lipid-lowering drugs (colestyramine), increased toxicity methotrexate. Antibiotics that are poorly absorbed from the gastrointestinal tract (including tetracyclines, chloramphenicol) reduce the absorption of methotrexate and disrupt its metabolism due to suppression of normal intestinal microflora.
When used simultaneously with methotrexate, retinoids, azathioprine, and sulfasalazine increase the risk of developing hepatotoxicity. Parenteral use of acyclovir against the background of intrathecal administration of methotrexate increases the risk of developing neurological disorders.
When using methotrexate simultaneously with multivitamin preparations containing folic acid or its derivatives, the effectiveness of methotrexate therapy may be reduced.
L-asparaginase is an antagonist of methotrexate.
Anesthesia using dinitrogen oxide during methotrexate therapy can lead to the development of unpredictable severe myelosuppression and stomatitis.
When used concomitantly with methotrexate, amiodarone may promote skin ulceration.
Methotrexate reduces the clearance of theophylline.
Skin cancer has been identified in several patients with psoriasis or mycosis fungoides treated with methotrexate in combination with PUVA therapy (methoxsalen and UVB).
Caution should be exercised when using packed red blood cells and methotrexate simultaneously.
Combining methotrexate therapy with radiotherapy may increase the risk of soft tissue necrosis.
Methotrexate may reduce the immunological response to vaccination; when the drug is administered simultaneously with a live vaccine, severe antigenic reactions may develop.
Overdose
Overdose
Treatment: immediately, preferably within the first hour, the introduction of a specific antidote – calcium folinate should be started in a dose equal to or higher than the dose of methotrexate; subsequent doses are administered as needed, depending on the concentration of methotrexate in the blood serum. To prevent precipitation of methotrexate and/or its metabolites in the renal tubules, the body is hydrated and the urine is alkalinized.
In case of overdose with intrathecal administration, repeated lumbar punctures should be performed immediately to ensure rapid drainage of cerebrospinal fluid. Neurosurgical intervention with ventriculolumbar perfusion is possible. All these procedures should be performed against the background of intensive supportive care and systemic administration of calcium folinate in high doses.
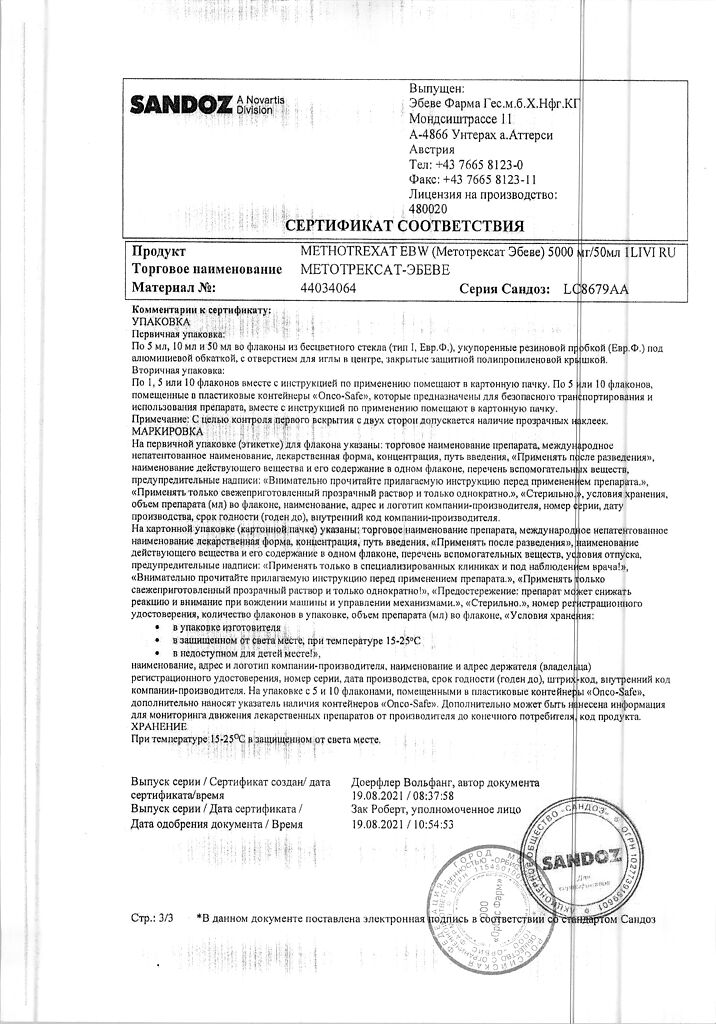
Storage conditions
Storage conditions
Store out of reach of children, protected from light at a temperature not exceeding 25°C.
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Fareva Unterach GmbH, Austria
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | Store out of reach of children, protected from light at a temperature not exceeding 25 ° C. |
| Manufacturer | Fareva Untereh GmbH, Austria |
| Medication form | concentrate for preparation of infusion solution |
| Brand | Fareva Untereh GmbH |
Other forms…
Related products
Buy Methotrexate-Ebeve, 5000 mg/50 ml 50 ml with delivery to USA, UK, Europe and over 120 other countries.