No products in the cart.
Metglyb, 2.5mg+400 mg 40 pcs
€10.18 €8.91
Description
A fixed combination of two oral hypoglycemic agents of different pharmacological groups: metformin and glibenclamide.
Metformin belongs to the group of biguanides and reduces both basal and postprandial plasma glucose. Metformin does not stimulate insulin secretion and therefore does not cause hypoglycemia.
It has 4 mechanisms of action:
– reduces glucose production by the liver by inhibiting gluconeogenesis and glycogenolysis;
– increases peripheral receptor sensitivity to insulin, glucose consumption and utilization by cells in the muscles;
– delays glucose absorption in the gastrointestinal tract;
– stabilizes or reduces body weight in patients with diabetes.
The drug also has beneficial effects on blood lipid composition, reducing total cholesterol, low-density lipoproteins (LDL) and triglycerides.
Glibenclamide belongs to the group of sulfonylurea derivatives of II generation. Glucose content when taking glibenclamide decreases as a result of stimulation of insulin secretion by pancreatic β-cells. Metformin and glibenclamide have different mechanisms of action, but mutually complement the hypoglycemic activity of each other. The combination of the two hypoglycemic agents has a synergistic effect in reducing glucose.
Indications
Indications
Type 2 diabetes mellitus in adults:
– if diet therapy, physical exercise and previous monotherapy with metformin or sulfonylurea derivatives are ineffective;
– to replace previous therapy with two drugs (metformin and a sulfonylurea derivative) in patients with stable and well-controlled glycemic levels.
Pharmacological effect
Pharmacological effect
A fixed combination of two oral hypoglycemic agents of different pharmacological groups: metformin and glibenclamide.
Metformin belongs to the group of biguanides and reduces the content of both basal and postprandial glucose in the blood plasma. Metformin does not stimulate insulin secretion and therefore does not cause hypoglycemia.
Has 4 mechanisms of action:
– reduces the production of glucose by the liver by inhibiting gluconeogenesis and glycogenolysis;
– increases the sensitivity of peripheral receptors to insulin, the consumption and utilization of glucose by cells in the muscles;
– delays the absorption of glucose in the gastrointestinal tract;
– stabilizes or reduces body weight in patients with diabetes.
The drug also has a beneficial effect on blood lipids, reducing the content of total cholesterol, low-density lipoproteins (LDL) and triglycerides.
Glibenclamide belongs to the group of sulfonylurea derivatives of the second generation. Glucose content when taking glibenclamide decreases as a result of stimulation of insulin secretion by pancreatic β-cells. Metformin and glibenclamide have different mechanisms of action, but complement each other’s hypoglycemic activity. The combination of two hypoglycemic agents has a synergistic effect in reducing glucose levels.
Special instructions
Special instructions
Treatment with Metglib® is carried out only under the supervision of a doctor!
When taking the drug, you must strictly follow your doctor’s recommendations regarding diet and self-monitoring of blood glucose concentrations.
It is necessary to regularly monitor the level of glycemia on an empty stomach and after meals. Lactic acidosis
Active ingredient
Active ingredient
Glibenclamide, Metformin
Composition
Composition
1 tablet contains:
active substances:
metformin hydrochloride 400 mg,
glibenclamide 2.5 mg;
excipients:
calcium hydrogen phosphate dihydrate 50 mg,
corn starch 45 mg,
croscarmellose sodium 12 mg,
sodium stearyl fumarate 3 mg,
povidone 52 mg,
microcrystalline cellulose 35.5 mg;
film cover:
Opadry orange 20 mg, including: [hypromellose (hydroxypropyl methylcellulose) 6.75 mg,
hyprolose (hydroxypropylcellulose) 6.75 mg,
talc 4 mg,
titanium dioxide 2.236 mg,
iron dye red oxide 0.044 mg,
iron dye yellow oxide 0.22 mg].
Contraindications
Contraindications
– hypersensitivity to metformin, glibenclamide or other sulfonylurea derivatives, as well as to other components of the drug Metglib;
– diabetes mellitus type 1;
– diabetic ketoacidosis, diabetic precoma, diabetic coma;
– renal failure or impaired renal function (creatinine clearance less than 60 ml/min);
– acute conditions that can lead to changes in kidney function: dehydration, severe infection, shock, intravascular administration of iodine-containing contrast agents;
– acute or chronic diseases that are accompanied by tissue hypoxia: cardiac or respiratory failure, recent myocardial infarction;
– liver failure;
– porphyria;
-pregnancy, breastfeeding period;
– simultaneous use of miconazole;
– infectious diseases, major surgical interventions, injuries, extensive burns and other conditions requiring insulin therapy;
– chronic alcoholism, acute alcohol intoxication;
– lactic acidosis (including history);
– adherence to a hypocaloric diet (less than 1000 kcal/day);
– children under 18 years of age.
It is not recommended to use the drug in people over 60 years of age who perform heavy physical work, which is associated with an increased risk of developing lactic acidosis.
With caution:
– febrile syndrome;
– adrenal insufficiency;
– hypofunction of the anterior pituitary gland;
– diseases of the thyroid gland (with uncompensated impairment of its function);
– in elderly people over 70 years of age due to the risk of developing hypoglycemia.
Side Effects
Side Effects
During treatment with Metglib®, the following side effects may occur. WHO classification of the incidence of side effects:
very often – ≥1/10 prescriptions (>10%)
often – from ≥1/100 to 1% and
infrequently – from ≥1/1000 to 0.1% and
rarely – from ≥1/10000 to 0.01% and
very rarely –
Classification of undesirable side reactions in accordance with damage to organs and organ systems (medical dictionary for regulatory activities Med-DRA).
– Blood and lymphatic system disorders:
These adverse events disappear after discontinuation of the drug.
Rarely: leukopenia and thrombocytopenia.
Very rare: agranulocytosis, hemolytic anemia, bone marrow aplasia and pancytopenia.
– Immune system disorders:
Very rare: anaphylactic shock.
Cross-hypersensitivity reactions to sulfonamides and their derivatives may occur.
– Metabolic and nutritional disorders: Hypoglycemia.
Rarely: attacks of hepatic porphyria and cutaneous porphyria.
Very rare: lactic acidosis.
Decreased absorption of vitamin B12, accompanied by a decrease in its concentration in the blood serum with long-term use of metformin. When megaloblastic anemia is detected, the possibility of such an etiology must be taken into account. Disulfiram-like reaction when drinking ethanol.
– Nervous system disorders:
Common: taste disturbance (“metallic” taste in the mouth).
Visual disturbances: At the beginning of treatment, temporary visual disturbances may occur due to a decrease in blood glucose.
– Gastrointestinal disorders:
Very common: nausea, vomiting, diarrhea, abdominal pain and lack of appetite. These symptoms are more common at the beginning of treatment and in most cases go away on their own. To prevent the development of these symptoms, it is recommended to take the drug in 2 or 3 doses; Slowly increasing the dose of the drug also improves its tolerability.
– Disorders of the liver and biliary tract:
Very rare: abnormal liver function tests or hepatitis requiring discontinuation of treatment.
Disorders of the skin and subcutaneous tissues:
Rarely: skin reactions such as: itching, urticaria, maculopapular rash.
Very rare: cutaneous or visceral allergic vasculitis, erythema multiforme, exfoliative dermatitis, photosensitivity.
– Laboratory and instrumental data:
Uncommon: moderate to moderate increases in serum urea and creatinine concentrations.
Very rare: hyponatremia.
Interaction
Interaction
Contraindicated combinations:
Associated with the use of glibenclamide
Miconazole can provoke the development of hypoglycemia (up to the development of coma).
Associated with metformin use
Iodinated contrast media: Depending on renal function, the drug should be discontinued 48 hours before or after intravenous administration of iodinated contrast media.
Combinations not recommended: Related to the use of sulfonylurea derivatives
Ethanol: A disulfiram-like reaction (ethanol intolerance) is very rarely observed when taking ethanol and glibenclamide simultaneously. Ethanol may increase the hypoglycemic effect (by inhibiting compensatory reactions or delaying its metabolic inactivation), which may contribute to the development of hypoglycemic coma. During treatment with Metglib®, you should avoid drinking alcoholic beverages and medications containing ethanol. Phenylbutazone increases the hypoglycemic effect of sulfonylurea derivatives (by replacing sulfonylurea derivatives at protein binding sites and/or reducing their excretion). It is preferable to use other anti-inflammatory drugs that exhibit less interaction, or to warn the patient about the need to self-monitor glycemic levels; If necessary, the dose should be adjusted when using an anti-inflammatory drug together and after its discontinuation.
Associated with the use of glibenclamide
Bosentan in combination with glibenclamide increases the risk of hepatotoxicity.
It is recommended to avoid taking these drugs together. The hypoglycemic effect of glibenclamide may also be reduced.
Associated with metformin use
Ethanol: The risk of developing lactic acidosis increases with acute alcohol intoxication, especially in cases of fasting or poor nutrition or liver failure. During treatment with Metglib®, you should avoid drinking alcoholic beverages and medications containing ethanol.
Overdose
Overdose
In case of overdose, hypoglycemia may develop due to the presence of a sulfonylurea derivative in the drug.
Mild to moderate symptoms of hypoglycemia without loss of consciousness or neurological manifestations can be corrected by immediate consumption of sugar.
It is necessary to adjust the dose and/or change the diet. The occurrence of severe hypoglycemic reactions in patients with diabetes mellitus, accompanied by coma, paroxysm or other neurological disorders, requires emergency medical care.
Intravenous administration of dextrose solution is necessary immediately after diagnosis or suspicion of hypoglycemia, before hospitalization of the patient. After regaining consciousness, it is necessary to give the patient food rich in easily digestible carbohydrates (to avoid re-development of hypoglycemia).
Plasma clearance of glibenclamide may be increased in patients with liver disease. Since glibenclamide actively binds to blood proteins, the drug is not excreted during dialysis.
Long-term overdose or the presence of associated risk factors can provoke the development of lactic acidosis, since the drug contains metformin.
Lactic acidosis is a medical emergency; Treatment of lactic acidosis should be carried out in a hospital. The most effective treatment method for removing lactate and metformin is hemodialysis.
Storage conditions
Storage conditions
It is necessary to store in a well-ventilated, dry place, protected from light and out of reach of children, at a temperature not exceeding 30 ºС.
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
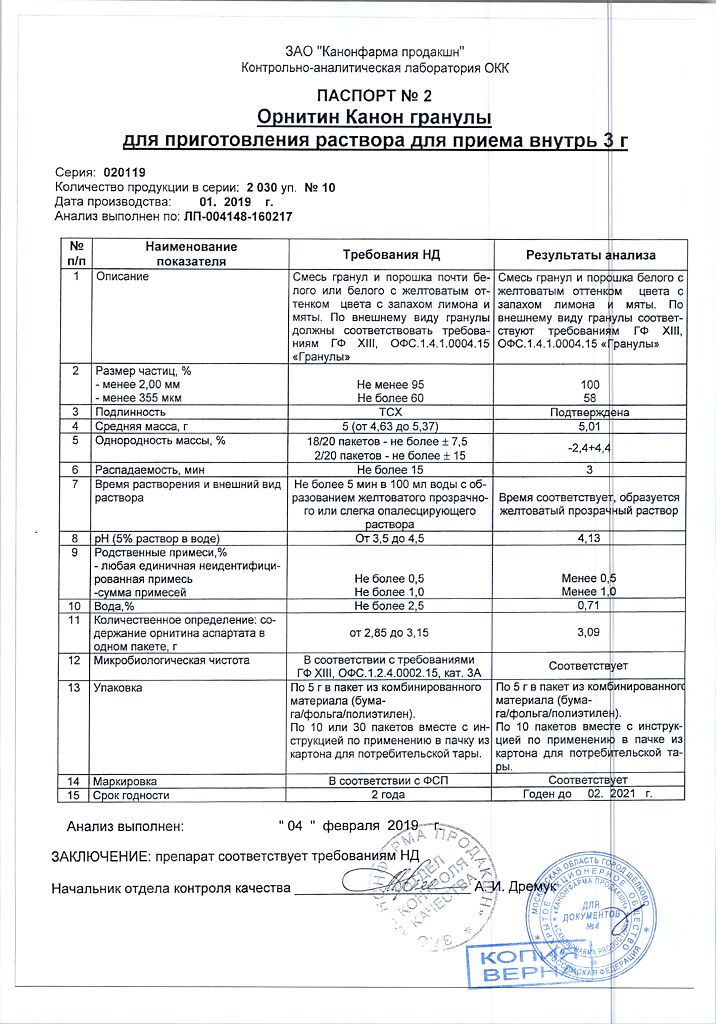
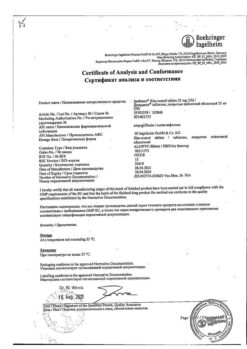
Kanonpharma production CJSC, Russia
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | Should be stored in a well-ventilated, dry, protected from light and out of the reach of children, at a temperature not exceeding 30 ºC. |
| Manufacturer | Kanonfarma Production ZAO, Russia |
| Medication form | pills |
| Brand | Kanonfarma Production ZAO |
Related products
Buy Metglyb, 2.5mg+400 mg 40 pcs with delivery to USA, UK, Europe and over 120 other countries.