No products in the cart.
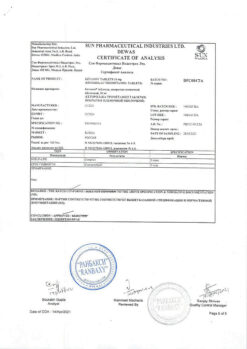
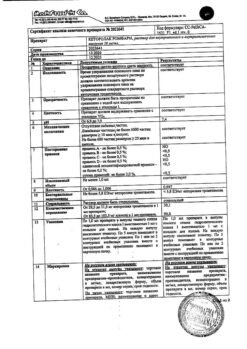
Meloflex Rompharm, 10 mg/ml 1.5 ml 5 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmgroup:
NSAIDs.
Pharm action:
Rompharm Meloflex is an NSAID, refers to enolic acid derivatives and has anti-inflammatory, analgesic and antipyretic effects.
The pronounced anti-inflammatory effect of meloxicam has been established in all standard models of inflammation. The mechanism of action of meloxicam is its ability to inhibit the synthesis of prostaglandins – known mediators of inflammation.
In vivo meloxicam inhibits the synthesis of prostaglandins in the site of inflammation to a greater extent than in the mucosa of the stomach or kidneys. These differences are due to more selective inhibition of cyclooxygenase-2 (COX-2) compared to cyclooxygenase-1 (COX-1). Inhibition of COX-2 is thought to provide the therapeutic effect of NSAIDs, whereas inhibition of the ever-present COX-1 isoenzyme may cause gastric and renal side effects. The selectivity of meloxicam against COX-2 has been confirmed in various test systems, both in vitro and ex vivo. The selective ability of meloxicam to inhibit COX-2 was shown when using human whole blood as a test system in vitro.
Ex vivo it was found that meloxicam (in doses of 7.5 mg and 15 mg) was more active in inhibiting COX-2, having a greater inhibitory effect on lipopolysaccharide-stimulated prostaglandin E2 production (COX-2-controlled response) than on thromboxane production involved in blood clotting (COX-1-controlled response). These effects were dose-dependent. Ex vivo, meloxicam at the recommended doses was shown to have no effect on platelet aggregation and bleeding time, in contrast to indomethacin, diclofenac, ibuprofen and naproxen, which significantly inhibited platelet aggregation and increased bleeding time.
Pharmacokinetics:
Absorption and distribution
Binding to plasma proteins is 99%. Passes through histohematic barriers, penetrates into the synovial fluid. Concentration in synovial fluid is 50% of the concentration in plasma.
Metabolized in the liver to inactive metabolites.
It is excreted through the gut and kidneys (about equal parts), 5% of the daily dose (through the gut) is unchanged. T1/2 – 20 hours. Plasma clearance – on average 8 ml/min (decreases in old age).
Indications
Indications
– osteoarthritis;
– rheumatoid arthritis;
— ankylosing spondylitis (Bechterew’s disease).
Intended for symptomatic therapy, reducing pain and inflammation at the time of use, does not affect the progression of the disease.
Pharmacological effect
Pharmacological effect
Pharmgroup:
NSAIDs.
Pharmaceutical action:
Meloflex Rompharm is an NSAID that belongs to enolic acid derivatives and has anti-inflammatory, analgesic and antipyretic effects.
The pronounced anti-inflammatory effect of meloxicam has been established in all standard models of inflammation. The mechanism of action of meloxicam is its ability to inhibit the synthesis of prostaglandins, known mediators of inflammation.
In vivo, meloxicam inhibits prostaglandin synthesis at the site of inflammation to a greater extent than in the gastric mucosa or kidneys. These differences are due to more selective inhibition of cyclooxygenase-2 (COX-2) compared with cyclooxygenase-1 (COX-1). Inhibition of COX-2 is thought to provide the therapeutic effect of NSAIDs, whereas inhibition of the constitutively present COX-1 isoenzyme may be responsible for gastric and renal side effects. The selectivity of meloxicam for COX-2 has been confirmed in various test systems, both in vitro and ex vivo. The selective ability of meloxicam to inhibit COX-2 was demonstrated when using human whole blood as a test system in vitro.
Ex vivo it was found that meloxicam (in doses of 7.5 mg and 15 mg) more actively inhibited COX-2, having a greater inhibitory effect on the production of prostaglandin E2 stimulated by lipopolysaccharide (reaction controlled by COX-2) than on the production of thromboxane, which is involved in the blood coagulation process (reaction controlled by COX-1). These effects were dose dependent. Ex vivo it was shown that meloxicam at recommended doses did not affect platelet aggregation and bleeding time, in contrast to indomethacin, diclofenac, ibuprofen and naproxen, which significantly suppressed platelet aggregation and increased bleeding time.
Pharmacokinetics:
Suction and distribution
Plasma protein binding – 99%. Passes through histohematic barriers and penetrates into the synovial fluid. Concentration in synovial fluid is 50% of plasma concentration.
Metabolism and excretion
Metabolized in the liver to inactive metabolites.
Excreted through the intestines and kidneys (in approximately equal parts), unchanged – 5% of the daily dose (through the intestines). T1/2 – 20 hours. Plasma clearance – on average 8 ml/min (decreases in old age).
Special instructions
Special instructions
Caution should be exercised when treating patients with a history of gastrointestinal diseases. Patients experiencing gastrointestinal symptoms should be monitored regularly. If ulcerative lesions of the gastrointestinal tract or gastrointestinal bleeding occur, Meloflex Rompharm should be discontinued.
As with the use of other NSAIDs, gastrointestinal bleeding, ulcers and perforations, potentially life-threatening to the patient, can occur during treatment at any time, both in the presence of warning symptoms or a history of serious gastrointestinal complications, and in the absence of these signs. The consequences of these complications are generally more serious in older people.
Particular attention should be paid to patients reporting the development of adverse events from the skin and mucous membranes. In such cases, discontinuation of the use of Meloflex Rompharm should be considered.
In patients with reduced BCC and reduced glomerular filtration (dehydration, chronic heart failure, liver cirrhosis, nephrotic syndrome, clinically significant kidney disease, taking diuretics, dehydration after major surgery), clinically pronounced chronic renal failure may occur, which is completely reversible after discontinuation of the drug (in such patients, daily diuresis and renal function should be monitored at the beginning of treatment).
If there is a persistent and significant increase in transaminases and changes in other indicators of liver function, the drug should be discontinued and control tests performed.
In patients with an increased risk of side effects, treatment begins with a dose of 7.5 mg. In end-stage chronic renal failure in patients on dialysis, the dose should not exceed 7.5 mg/day.
Impact on the ability to drive vehicles and operate machinery
There is no data on the negative effect of the drug on the ability to drive vehicles or operate machinery. If there are disorders of the central nervous system (decreased visual acuity, increased fatigue, dizziness or other disorders), these types of activities are contraindicated.
Active ingredient
Active ingredient
Meloxicam
Composition
Composition
Active ingredient:
meloxicam 10 mg
Excipients:
meglumine – 6.25 mg,
glycofurfural – 100 mg,
Poloxamer 188 – 50 mg,
glycine – 5 mg,
sodium chloride – 3.5 mg,
sodium hydroxide solution 1M – pH 8.6-9,
water for d/i – up to 1 ml.
Pregnancy
Pregnancy
Inhibition of prostaglandin synthesis may have undesirable effects on pregnancy and fetal development. Thus, Meloflex Rompharm is contraindicated during pregnancy.
Meloxicam is excreted in breast milk, therefore Meloflex Rompharm is contraindicated during lactation. While taking the drug, you must stop breastfeeding.
Contraindications
Contraindications
a combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid and pyrazolone drugs;
peptic ulcer of the stomach and duodenum (in the acute phase);
active gastrointestinal bleeding;
chronic renal failure in patients not undergoing dialysis (creatinine clearance less than 30 ml/min);
progressive kidney disease;
severe liver failure or active liver disease;
condition after coronary artery bypass surgery;
confirmed hyperkalemia;
inflammatory bowel diseases;
children and adolescents up to 18 years of age;
hypersensitivity to the components of the drug;
hypersensitivity to other NSAIDs.
With caution: old age, coronary artery disease, chronic heart failure, cerebrovascular diseases, dyslipidemia/hyperlipidemia, diabetes mellitus, peripheral arterial disease, smoking, chronic renal failure (creatinine clearance 30-60 ml/min), history of ulcerative lesions of the gastrointestinal tract, presence of Helicobacter pylori infection, long-term use of NSAIDs, alcoholism, severe somatic diseases, simultaneous use of oral corticosteroids (including prednisolone), anticoagulants (including warfarin), antiplatelet agents (including clopidogrel), selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline).
Side Effects
Side Effects
From the digestive system: often – dyspepsia, incl. nausea, vomiting, abdominal pain, constipation, flatulence, diarrhea; infrequently – transient increase in the activity of liver transaminases, hyperbilirubinemia, belching, esophagitis, gastroduodenal ulcer, bleeding from the gastrointestinal tract (including hidden), stomatitis; rarely – gastrointestinal perforation, colitis, hepatitis, gastritis.
From the hematopoietic organs: often – anemia; infrequently – changes in the blood formula, incl. leukopenia, thromocytopenia.
From the skin: often – itching, skin rash; infrequently – urticaria; rarely – photosensitivity, bullous rashes, erythema multiforme, incl. Stevens-Johnson syndrome, toxic epidermal necrolysis.
From the respiratory system: infrequently – the occurrence of attacks of bronchial asthma in persons allergic to acetylsalicylic acid or other NSAIDs.
From the side of the central nervous system: often – dizziness, headache; infrequently – vertigo, tinnitus, drowsiness; rarely – confusion, disorientation, emotional lability.
From the cardiovascular system: often – peripheral edema; infrequently – increased blood pressure, palpitations, flushes of blood to the skin of the face.
From the urinary system: infrequently – hypercreatininemia and/or increased concentration of urea in the blood serum; rarely – acute renal failure; no connection with meloxicam has been established – interstitial nephritis, albuminuria, hematuria.
From the senses: rarely – conjunctivitis, visual impairment, incl. blurred visual perception.
Allergic reactions: rarely – angioedema, anaphylactoid/anaphylactic reactions.
Interaction
Interaction
Pharmacodynamic interaction
The simultaneous use of several NSAIDs (including salicylates) may increase the risk of developing erosive and ulcerative lesions of the gastrointestinal tract due to a synergistic effect, therefore the use of meloxicam with other NSAIDs is not recommended.
When using meloxicam with diuretics, the patient must drink sufficient fluids, and regular medical monitoring of renal function is required before and during treatment.
Combined use with indirect anticoagulants increases the risk of bleeding due to inhibition of platelet function and damage to the mucous membrane of the stomach and intestines. Therefore, combined use with NSAIDs and indirect anticoagulants is not recommended.
With the combined use of thrombolytic and antithrombotic drugs with meloxicam, an increased risk of bleeding is possible (periodic monitoring of blood coagulation parameters is necessary).
Concomitant use with ACE inhibitors and other antihypertensive drugs in elderly patients with symptoms of dehydration may provoke the development of acute renal failure. In addition, combined use with meloxicam may reduce their hypotensive effect.
Meloxicam enhances the nephrotoxic effect of cyclosporine.
Meloxicam may reduce the effectiveness of contraceptives.
Pharmacokinetic interaction
NSAIDs may increase serum lithium concentrations to toxic levels (decreased renal excretion of lithium). Therefore, the simultaneous use of meloxicam with lithium preparations is not recommended. If their combined use is necessary, the lithium content in the blood serum should be carefully monitored before, during and after the end of the course of therapy with meloxicam and lithium preparations.
When used simultaneously with methotrexate, the negative effect on the hematopoietic system increases (the risk of developing anemia and leukopenia). Periodic monitoring of the hemogram is necessary.
Cholestyramine accelerates the elimination of meloxicam, increasing the clearance of meloxicam by 50%, reducing its T1/2 by 13±3 hours. This interaction is of clinical significance.
When taken simultaneously with antacids, cimetidine and digoxin, no significant clinical interaction is observed.
NSAIDs reduce the effectiveness of contraceptive intrauterine devices.
When using meloxicam together with drugs that have a known ability to inhibit CYP2C9 and/or CYP3A4 (or are metabolized by these enzymes), the possibility of pharmacokinetic interaction should be taken into account. The possibility of interaction of meloxicam with oral hypoglycemic agents cannot be excluded.
When meloxicam is used simultaneously with selective serotonin reuptake inhibitors, the risk of gastrointestinal bleeding increases.
Overdose
Overdose
Increased dose-dependent side effects.
Symptoms: impaired consciousness, nausea, vomiting, epigastric pain, gastrointestinal bleeding, acute renal failure, acute liver failure, respiratory arrest, asystole.
Treatment: symptomatic therapy. Forced diuresis, alkalinization of urine, hemodialysis are ineffective due to the high degree of binding of meloxicam to plasma proteins. There is no specific antidote.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
4 years
Manufacturer
Manufacturer
K.O.Rompharm Company S.R.L., Romania
Additional information
| Shelf life | 4 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | C.O.Rompharm Company S.R.L., Romania |
| Medication form | solution |
| Brand | C.O.Rompharm Company S.R.L. |
Related products
Buy Meloflex Rompharm, 10 mg/ml 1.5 ml 5 pcs with delivery to USA, UK, Europe and over 120 other countries.