No products in the cart.
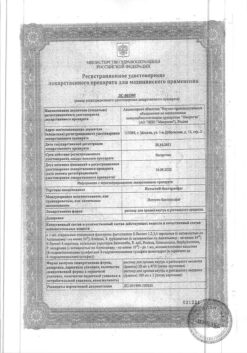
Measles MMR II vaccine, 1 dose
€1.00
Out of stock
(E-mail when Stock is available)
Description
A vaccine for the prevention of rubella, measles and mumps. M-M-P II has high immunogenic properties.
Single administration of the vaccine causes 95% of susceptible patients to develop measles hemagglutination inhibitory antibodies, 96% to develop mumps neutralizing antibodies, and 99% to develop rubella virus hemagglutination inhibitory antibodies.
The rubella virus strain RA 27/3 of M-M-P II detects higher titers of hemagglutination inhibitory, complement-binding and neutralizing antibodies immediately after vaccination than other rubella vaccine strains.
It has been shown to induce a broader spectrum of circulating antibodies, including anti-titer and anti-iotic precipitating antibodies. The rubella virus strain RA 27/3 immunologically mimics natural infection to a greater extent than other rubella vaccine viruses. The increased level and broader spectrum of antibodies induced by the RA 27/3 vaccine strain of rubella virus correlate with greater resistance to subclinical reinfection by natural virus and more reliably provide prolonged immunity.
Vaccination with the M-M-P II vaccine ensures that antibody levels in the patient’s blood will persist for more than 11 years.
The immunization of women of childbearing age who have no immunity to rubella protects them from getting rubella during pregnancy, which in turn prevents the infection of the fetus and the development of lesions due to congenital rubella.
Indications
Indications
Composition
Composition
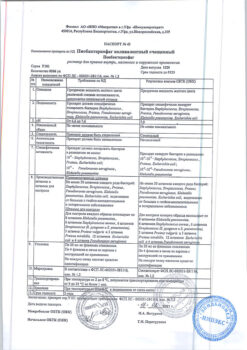
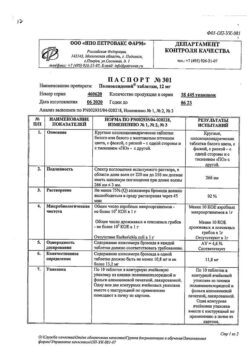
Lyophilized powder for injection
1 dose
live attenuated viruses, including.Ñ.:
standard measles viruses (US)
1000 TID50*
standard mumps viruses (US)
5000 TID50*
standard rubella viruses (US)
/td>
1000 TID50*
Associates:
neomycin (25 µg per dose),
sorbitol,
sucrose,
human albumin,
calf embryo serum,
hydrolyzed gelatin,
sodium chloride,
sodium phosphate.
The product does not contain preservatives.
The viruses in the vaccine are identical to those used to produce Attenuvax (live measles vaccine, MSD), Mumpsvax (live mumps vaccine, MSD), Meruvax II (live rubella vaccine, MSD).
Attenuvax (live measles vaccine, MSD), a more attenuated line of measles virus derived from the attenuated (Enders) Edmonston strain and grown in chicken embryo cell culture.
Mumpsvax (live mumps vaccine, MSD), a Jeryl Lynn (level B) strain of mumps virus grown in chicken embryo cell culture;
Meruvax II (live rubella vaccine, MSD), Wistar RA 27/3 strain of live attenuated rubella virus grown in human diploid pulmonary fibroblast cell culture (WI-38).
* – TID50 is the dose that infects 50% of the cell cultures.
Interaction
Interaction
The expected immune response may be impaired if M-M-R II and immunoglobulins are administered simultaneously.
M-M-R II was administered simultaneously with chickenpox and Haemophilus influenzae B vaccinations administered with different syringes to different body sites. No impairment of the immune response to the injected antigens was found, and the nature, frequency and severity of adverse reactions were similar to those of the monotherapy injections.
The mass administration of DPT and/or live polio vaccines simultaneously with measles, mumps and rubella vaccines is not recommended due to limited data on the results of combining these antigens.
However, data from published studies regarding concomitant administration of commercially available polyvalent vaccines (e.g., DPT, OPV, M-M-R, Haemophilus influenzae B vaccine and hepatitis B vaccine) indicate no interaction between them.
Directions for use
Directions for use
The vaccine is administered by injection by injection, preferably into the outer surface of the upper third of the upper arm at a dose of 0.5 ml. The vaccine dose is the same for patients of all ages.
In children less than 15 months of age, there may be no response to the measles component of the vaccine due to residual circulating measles antibodies from the mother, and the younger the child, the lower the probability of seroconversion. In geographically isolated or other inaccessible populations in which immunization programs are difficult to implement and in populations with a high risk of natural exposure to measles virus in children under 15 months of age, earlier administration of the vaccine is possible. If vaccination was given before 12 months of age, revaccination should be given at 15 months of age.
Special Instructions
Special Instructions
The vaccine is not administered intravenously.
In view of the possibility of anaphylactic and anaphylactoid reactions, the necessary treatment, including adrenaline for injection (1:1000), should be prepared before administering the vaccine.
There is evidence that in children immunized before the age of 1 year, repeat vaccination at a later date does not always result in prolonged antibody persistence, so the benefits of early immunization must be weighed against the possibility of inadequate response to repeat vaccination.
Vaccination of persons in contact with a measles patient may provide some protection if the vaccine is administered within the first 72 h after contact. If, however, the vaccine was administered several days before exposure, a high preventive effect would be achieved. There are no conclusive data on the preventive effect of vaccination of persons in contact with patients with mumps and rubella.
There have been reports of patients with severe immune disorders developing cases of encephalitis, pneumonia, and death after accidental administration of the measles vaccine as a result of disseminated infection caused by the vaccine virus.
Particular caution should be exercised when vaccinating patients who have a history of seizures (including relatives), brain tissue damage, or any other condition where fever should be avoided.
Patients with thrombocytopenia may develop more severe thrombocytopenia after vaccination. In addition, thrombocytopenia may develop in persons with thrombocytopenia after the first M-M-P II vaccination (or the vaccine it contains) when subsequent doses are administered. In the latter case, specific immunity should be evaluated to determine whether a second vaccination is necessary. In these cases, the potential risk/benefit ratio should be carefully evaluated before vaccination.
Children and adolescents infected with human immunodeficiency virus but without obvious clinical signs of immunosuppression may be vaccinated. In these cases, vaccination may be less effective than in uninfected individuals.
M-M-R II should be given 1 month before or 1 month after other vaccines.
In most patients, small amounts of live, attenuated rubella virus were excreted from the nose and pharynx within 7 to 28 days after vaccination. The possibility of transmission of the virus in this way from a vaccinated person to other people has not been proven. In close personal contact, this possibility should theoretically be considered, but the risk is negligible.
There are no reports of transmission of live attenuated measles or mumps virus from vaccinated persons to susceptible individuals.
There are reports that live measles, mumps, and rubella vaccines administered separately may result in a temporary reduction of cutaneous sensitivity to tuberculin. Therefore, if necessary, tuberculin tests should be performed before or at the same time as the M-M-P II vaccine.
In children receiving tuberculosis therapy, no worsening of the disease course has been reported after administration of live measles vaccine. There are no reports of studies of the effect of live measles vaccine on the course of untreated tuberculosis in children.
Arthralgia and/or arthritis (usually transient and rarely chronic) and polyneuritis are characteristic of natural rubella and can vary in frequency and severity depending on age and sex, being most severe in adult women and least severe in prepubertal children. In naturally occurring rubella, chronic arthritis can occur due to persistence of the virus and/or viral antigen released from body tissues. Vaccinated individuals rarely develop chronic joint symptoms.
A study of the widespread clinical use of more than 200 million doses of M-M-P and M-M-P II worldwide over 25 years (1971-1996) suggests that reports of serious adverse events, such as encephalitis and encephalopathy, remain rare. Cases of subacute sclerosing panencephalitis (SSPE) have been described in children who had not had measles but had received the measles vaccine. In some of these children, the illness may have been caused by unrecognized measles during the first year of life or by measles vaccination. Given the estimated prevalence of measles vaccination, the possible risk of developing PSPE with measles vaccination is about 1 case per 1 million doses of vaccine. This is significantly less than the measles incidence of 6-22 cases of HSPE per million measles cases. Measles vaccination is thought to generally prevent PSPE, reducing the incidence of measles, where the risk of this complication is high.
There have been rare reports of the occurrence of panniculitis after administration of the measles vaccine.
The vaccination should be given 2 weeks before or 3 months after administration of human immunoglobulin or blood or plasma transfusions.
Like any other vaccine, M-M-P II does not provide protection against the disease in 100% of those vaccinated.
Please note that each dose of dissolved M-M-P II vaccine contains about 25 µg of neomycin.
Pediatric use
The safety and efficacy of the measles vaccine in children under 6 months of age has not been established. The safety and efficacy of mumps and rubella vaccines in children under 1 year of age have not been established.
Contraindications
Contraindications
Side effects
Side effects
The same adverse reactions have been observed with M-M-P II vaccine as with monovalent or combination vaccines.
Local reactions: often a rapid burning and/or soreness at the injection site; rarely erythema, thickening and skin sensitivity.
Dermatological reactions: rarely – rash (usually minor, but sometimes generalized; appears between 5 and 12 days).
In the digestive system: rarely – parotitis, nausea, vomiting, diarrhea.
Hematopoietic system: rare – thrombocytopenia, thrombocytopenic purpura.
Lymphatic system disorders: rarely regional lymphadenopathy.
Allergic reactions: rare – skin reactions such as blisters or hyperemia at the injection site, anaphylactic and anaphylactoid reactions, angioedema (including peripheral edema and facial edema), bronchospasm, urticaria.
Muscular system disorders: rare – arthralgia and/or arthritis (usually transient, in some cases chronic), myalgia.
In vaccinating children, joint reactions are not typical and usually transient. The incidence of arthritis in women is usually higher than in children, 12%-20% and 0-3%, respectively, and reactions are usually more severe and prolonged.
Joint syndrome in women tends to be more severe and prolonged; symptoms may persist for several months, and in rare cases, even years. Adolescent girls have a higher incidence of joint reactions than children, but a lower incidence than adult women. Even in older women (35-45 years old), these reactions are usually well tolerated and do not affect normal activities of life.
CNS and peripheral nervous system disorders: Rarely, febrile seizures in children, seizures not associated with fever, headache, dizziness, irritability, paresthesias, polyneuritis, polyneuropathy, Guillain-Barré syndrome, ataxia, subacute sclerosing encephalitis, various variants of optic neuritis including retrobulbar rhinitis, papillitis; eye nerve palsy, deafness associated with neuritis.
An isolated case of encephalitis/encephalopathy with an incidence of 1 in 3 million doses has been described. In no case have these reactions been shown to be actually related to vaccination. The risk of developing such severe neurological disorders after administration of live measles vaccine remains significantly lower than the risk of encephalitis and encephalopathies in measles disease (1 in 2000 cases described).
Sensory organs: rarely – otitis media, conjunctivitis.
Respiratory system: rarely – pneumonia, cough, rhinitis.
Perior genital system disorders: rarely – orchitis.
Others: rare – fever (38.8°C or more; usually appears between days 5 and 12), sore throat, malaise, mitigated measles, syncope.
There have been very rare reports of death from various and in some cases unknown causes after administration of measles, mumps, and rubella vaccine, but no correlation with vaccination has been established. In an observational study of widespread clinical use involving 1.5 million children and adults vaccinated with M-M-P II during 1982-1993, there were no reports of fatal outcomes or long-term complications.
Overdose
Overdose
Additional information
| Shelf life | The shelf life of the vaccine is 3 years, the solvent 5 years. Do not use after the expiration date. It is recommended to use the vaccine as soon as possible after dissolution; storage in a dark place at 2-8°C for not more than 8 hours is allowed. The vaccine must be kept at 10°C or lower to maintain its properties during transportation. Freezing during transportation does not affect the quality of the product. |
|---|---|
| Conditions of storage | The M-M-P II vaccine should be stored at 2° to 8°C in a dark place before dissolution. The vaccine must be protected from light, since viral inactivation is possible. The solvent can be stored in the refrigerator together with the lyophilized vaccine or separately at room temperature |
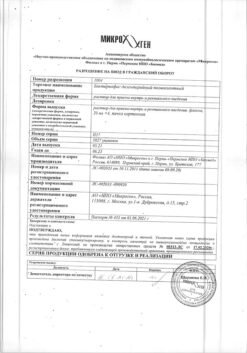
| Manufacturer | Merck Sharp & Doum B.V., The Netherlands |
| Brand | Merck Sharp & Doum B.V. |
Related products
Buy Measles MMR II vaccine, 1 dose with delivery to USA, UK, Europe and over 120 other countries.