No products in the cart.
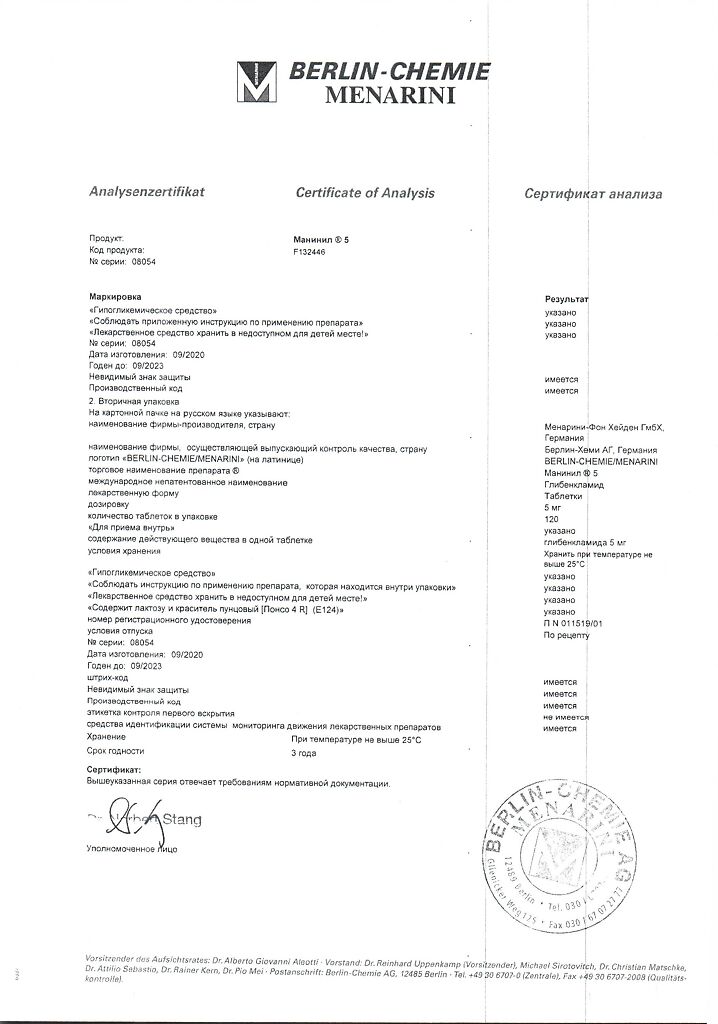
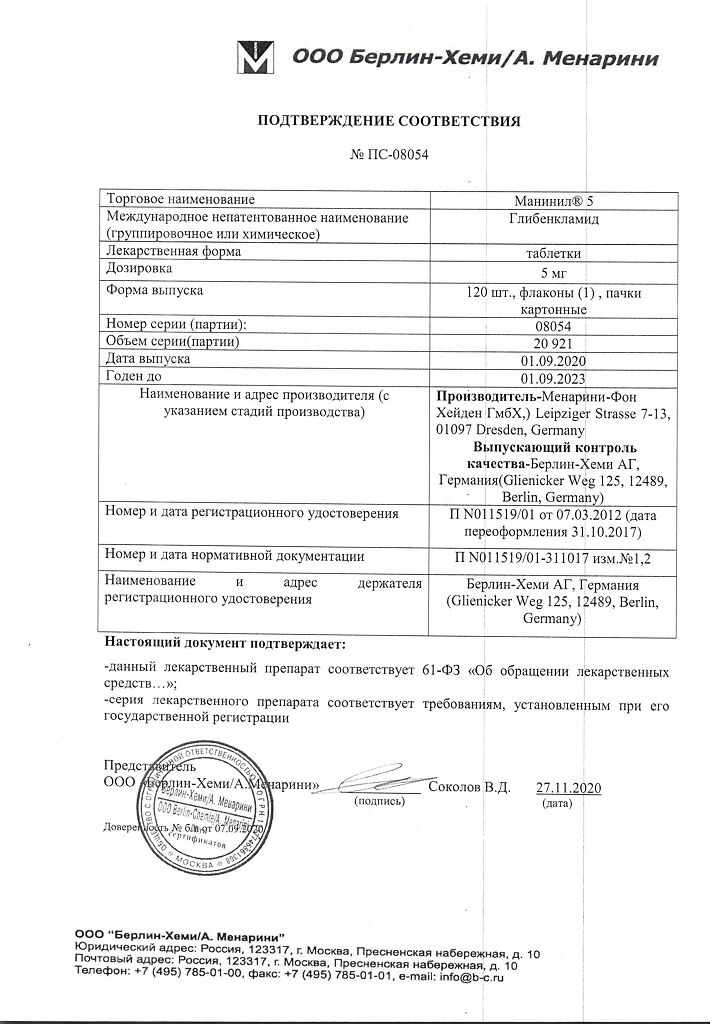
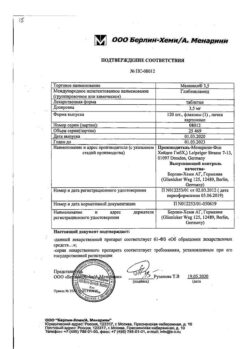
Maninil 5, tablets 5 mg 120 pcs
€4.22 €3.75
Description
Pharmacodynamics
The oral hypoglycemic drug from the group of sulfonylurea derivatives of the II generation.
Stimulates insulin secretion by binding to specific receptors of pancreatic β-cell membrane, reduces the threshold of glucose irritation of pancreatic β-cells, increases sensitivity to insulin and the degree of its binding to the target cells, increases insulin release, increases the effect of insulin on glucose absorption by muscles and liver, thus reducing the concentration of glucose in blood. Acts in the second stage of insulin secretion. Inhibits lipolysis in adipose tissue. It has a hypolipidemic effect, reduces the thrombogenic properties of the blood.
Maninil® 1.5 and Maninil® 3.5 in micronized form is a high-tech, specially milled form of glibenclamide that allows the drug to be absorbed from the gastrointestinal tract faster. Due to the earlier reaching the Cmax of glibenclamide in plasma, the hypoglycemic effect almost corresponds in time to the rise in blood glucose concentration after a meal, which makes the action of the drug more mild and physiological. The duration of hypoglycemic action is 20-24 hours.
The hypoglycemic effect of the drug Maninil® 5 develops in 2 hours and lasts 12 hours.
Pharmacokinetics
Intake
After oral administration of Maninil 1.75 and Maninil 3.5, rapid and almost complete absorption from the GI tract is observed. Complete release of the microionized active ingredient occurs within 5 minutes.
After oral administration of Maninil 5 the absorption from the GIT is 48-84%. Tmax is 1-2 h. Absolute bioavailability is 49-59%.
Distribution
The binding to plasma proteins is over 98% for Maninil 1.75 and Maninil 3.5, 95% for Maninil 5.
Metabolism and excretion
It is almost completely metabolized in the liver to form two inactive metabolites, one of which is excreted by the kidneys and the other in the bile.
The T1/2 for Maninil 1.75 and Maninil 3.5 is 1.5-3.5 h, for Maninil 5 is 3-16 h.
Indications
Indications
Type 2 diabetes mellitus – as monotherapy or in combination therapy with other oral hypoglycemic drugs, except sulfonylurea derivatives and glinides.
Active ingredient
Active ingredient
Composition
Composition
Active ingredients:
Glibenclamide 5 mg.
Auxiliary substances:
lactose monohydrate – 90 mg,
potato starch – 48.697 mg,
magnesium stearate – 1.5 mg,
Talc – 2.25 mg,
Gelatin – 2.55 mg,
Print dye (Ponceau 4R) (E124) – 0.003 mg.
How to take, the dosage
How to take, the dosage
The dose of the drug depends on age, severity of diabetes, and blood glucose concentrations on an empty stomach and 2 hours after meals.
The starting dose of Maninil® 1.75 is 1-2 tablets (1.75-3.5 mg) 1 time daily. In case of insufficient effectiveness under medical control the dose of the drug is gradually increased up to daily dose necessary for carbohydrate metabolism stabilization. Increase of dose should be made at intervals from several days to one week until reaching the required therapeutic dose, which should not exceed the maximum dose. The maximum daily dose of Maninil® 1.75 is 6 tablets (10.5 mg).
If the daily dose of glibenclamide exceeds 3 tablets of Maninil® 1.75, Maninil® 3.5 is recommended.
The transition from other hypoglycemic drugs to Maninil® 1.75 should be started under medical supervision with 1-2 tablets of Maninil® 1.75 daily (1.75-3.5 mg) and gradually increased to the desired therapeutic dose.
The starting dose of Maninil® 3.5 is 1/2 to 1 tablet (1.75 to 3 mg) once daily. In case of insufficient effectiveness under medical control the dose of the drug is gradually increased up to daily dose necessary for carbohydrate metabolism stabilization. Increase of dose should be made at intervals from several days to one week until reaching the required therapeutic dose, which should not exceed the maximum dose. The maximum daily dose of Maninil® 3.5 is 3 tablets (10.5 mg).
Transition from other hypoglycemic drugs to Maninil® 3.5 should be started under medical supervision with 1/2 to 1 tablet of Maninil® 3.5 daily (1.75 to 3.5 mg) and gradually increased to the required therapeutic dose.
The starting dose of Maninil® 5 is 1/2-1 tablet (2.5-5 mg) once daily. In case of insufficient effectiveness the dose is gradually increased under medical control up to daily dose necessary for carbohydrate metabolism stabilization. Increase of dose should be made at intervals from several days to one week until reaching the required therapeutic dose, which should not exceed the maximum dose. The maximum daily dose of Maninil® 5 is 3 tablets (15 mg).
Transition from other hypoglycemic drugs to Maninil® 5 should be started under medical supervision with 1/2 to 1 tablet of Maninil® 5 daily (2.5 to 5 mg) and gradually increased to the required therapeutic dose.
In elderly patients, frail patients, malnourished patients, patients with severe renal or hepatic impairment, the starting and maintenance dosage of Maninil® should be reduced because of the risk of hypoglycemia.
Maninil® should be taken before eating without chewing and with small amounts of fluid. Daily doses of up to 2 tablets should usually be taken once a day – in the morning, just before breakfast. Higher doses are divided into morning and evening doses.
If you miss one dose of the drug, the next tablet should be taken at the usual time, and no higher dose is allowed.
Interaction
Interaction
The hypoglycemic effect of Maninil® may be increased when concomitant administration with ACE inhibitors, anabolic agents and male sex hormones, other oral hypoglycemic agents (e.g., acarbose, biguanides) and insulin, azapropazone, NSAIDs, beta-adrenoblockers, quinolone derivatives, chloramphenicol, clofibrate and its analogues, coumarin derivatives, disopyramide, fenfluramine, antifungal drugs (miconazole, fluconazole), fluoxetine, MAO inhibitors, PASC, pentoxifylline (in high doses when administered parenterally) Perhexiline, pyrazolone derivatives, phosphamides (e.g., cyclophosphamide, ifosfamide, trophosphamide), probenecid, salicylates, sulfonamides, tetracyclines, and tritoqualine.
The urine acidifying agents (ammonium chloride, calcium chloride) enhance the effect of Maninil® by reducing its degree of dissociation and increasing its reabsorption.
The hypoglycemic effect of Maninil® may be decreased if barbiturates, isoniazid, diazoxide, GCS, glucagon, nicotinate (in high dose), phenytoin, phenothiazines, rifampicin are used simultaneously, Thiazide diuretics, acetazolamide, oral contraceptives and estrogens, thyroid hormone preparations, sympathomimetic agents, slow calcium channel blockers, lithium salts.
H2 receptor antagonists may decrease and increase the hypoglycemic effect of Maninil®.
Pentamidine may cause a strong decrease or increase in blood glucose concentration in single cases.
The effects of coumarin derivatives may be increased or decreased when used concomitantly with Maninil®.
Besides enhancing the hypoglycemic effect, beta-adrenoblockers, clonidine, guanethidine and reserpine, as well as medications with a central mechanism of action, may attenuate the sensation of precursor symptoms of hypoglycemia.
Special Instructions
Special Instructions
During treatment with Maninil® , the physician’s recommendations for diet and self-monitoring of blood glucose concentrations should be strictly followed.
Long-term abstinence from food, inadequate carbohydrate supply, vigorous physical activity, diarrhea, or vomiting pose a risk of hypoglycemia.
The concomitant use of CNS-acting medications that lower BP (including beta-adrenoblockers), and peripheral neuropathy may mask the symptoms of hypoglycemia.
In elderly patients, the risk of hypoglycemia is slightly higher; therefore, more careful selection of the drug dose and regular monitoring of blood glucose concentration on an empty stomach and after meals is necessary, especially at the beginning of treatment.
Alcohol can induce hypoglycemia, and disulfiram-like reactions (nausea, vomiting, abdominal pain, fever in the face and upper trunk, tachycardia, dizziness, headache), therefore, it is necessary to abstain from alcohol during treatment with Maninil®.
Large surgical interventions and injuries, extensive burns, infectious diseases with febrile syndrome may require withdrawal of oral hypoglycemic drugs and prescription of insulin.
Long periods of sun exposure are not recommended during treatment.
Impact on ability to drive vehicles and other mechanisms requiring increased concentration
Patients should use caution during treatment when driving vehicles and other potentially hazardous activities requiring increased attention and rapid psychomotor reactions.
Contraindications
Contraindications
Side effects
Side effects
Definition of the frequency of side effects:
Metabolic disorders: often – hypoglycemia (hunger, hyperthermia, tachycardia, drowsiness, weakness, dampness of the skin, movement coordination disorders, tremor, general anxiety, fear, headache, transient neurological disorders, including visual and speech disorders, appearance of paresis or paralysis or altered sense perception); increased body weight.
Gastrointestinal system disorders: infrequent – nausea, feeling of heaviness in the stomach, belching, vomiting, abdominal pain, diarrhea, metallic taste in the mouth.
Hepatic and biliary tract disorders: very rarely – temporary increase in liver enzymes activity, intrahepatic cholestasis, hepatitis.
The immune system: infrequent – itching, urticaria, purpura, petechiae, hypersensitization; very rare – generalized allergic reactions accompanied with skin rash, arthralgia, fever, proteinuria and jaundice; allergic vasculitis; anaphylactic shock.
Hematopoietic system: rare – thrombocytopenia; very rare: leukopenia, erythropenia, agranulocytosis; in single cases – pancytopenia, hemolytic anemia.
Others: very rare – visual disturbances and accommodation disorders, increased diuresis, transient proteinuria, hyponatremia, disulfiram-like reaction when taking alcohol (the most common signs of effect: nausea, vomiting, abdominal pain, sensation of heat in the face and upper torso, tachycardia, dizziness, headache), cross-allergy to probenecid, sulfonylurea derivatives, sulfonamides, diuretics (diuretics) containing a sulfonamide group in the molecule.
Overdose
Overdose
Symptoms: hypoglycemia (feeling of hunger, hyperthermia, tachycardia, drowsiness, weakness, wetness of the skin, poor coordination of movements, tremor, general restlessness, feeling of fear, headache, transient neurological disorders (such as visual and speech disorders, manifestations of paresis or paralysis or altered sensation perception). With progression of hypoglycemia, the patient may lose self-control and consciousness, the development of hypoglycemic coma.
Treatment: In mild hypoglycemia the patient should take a piece of sugar, food or drinks with high sugar content (jam, honey, a glass of sweet tea). If unconscious, glucose should be administered intravenously – 40-80 ml of 40% dextrose (glucose) solution, followed by an infusion of 5-10% dextrose solution. Then an additional 1 mg of glucagon may be administered by IV, IM or p/k. If the patient does not regain consciousness, this measure may be repeated; intensive care may be required thereafter.
Pregnancy use
Pregnancy use
The drug is contraindicated in pregnancy and during breastfeeding.
In case of pregnancy the drug should be discontinued.
Similarities
Similarities
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a light-protected place, at a temperature not exceeding 25 °C |
| Manufacturer | Menarini-Von Heyden GmbH, Germany |
| Medication form | pills |
| Brand | Menarini-Von Heyden GmbH |
Other forms…
Related products
Buy Maninil 5, tablets 5 mg 120 pcs with delivery to USA, UK, Europe and over 120 other countries.