No products in the cart.
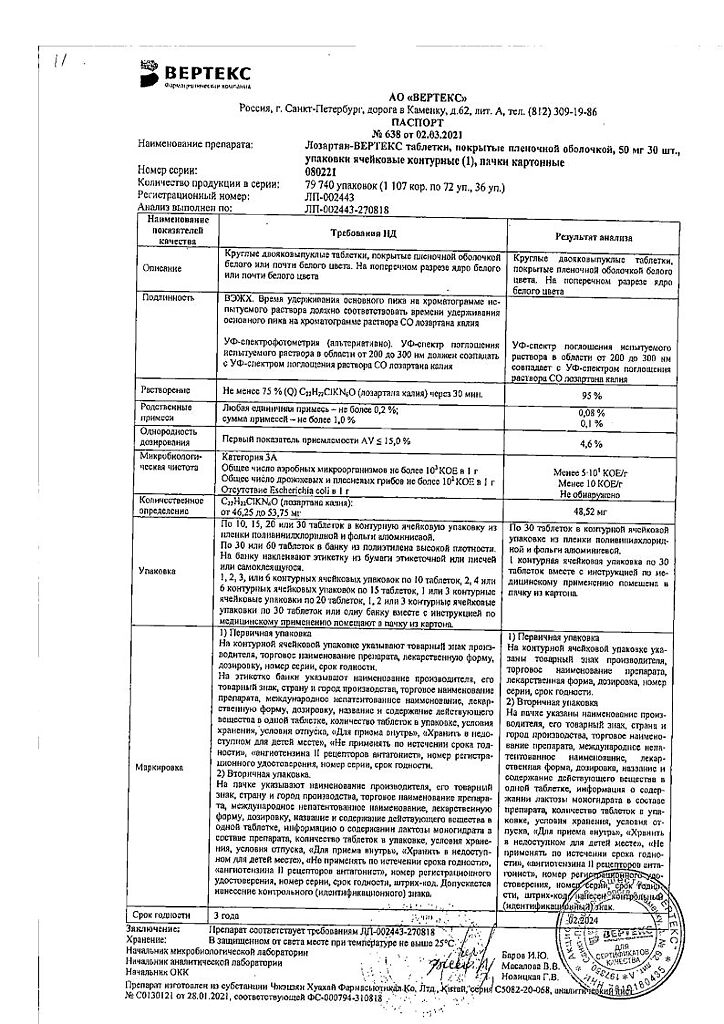
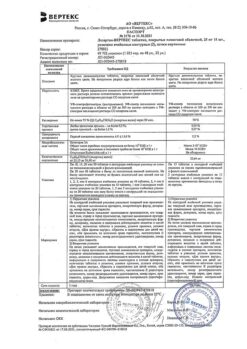
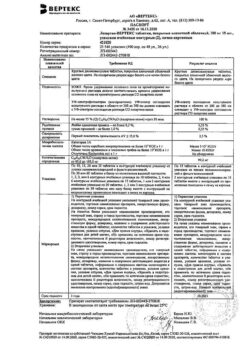
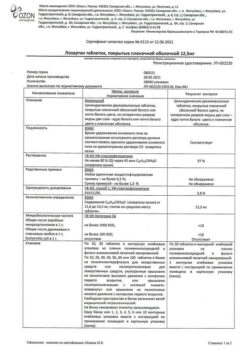
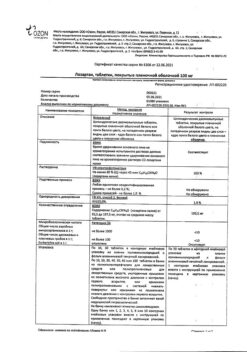
Losartan-Vertex, 50 30 pcs.
€5.37 €4.77
Description
Pharmacotherapeutic group
Drugs affecting the renin-angiotensin system. Angiotensin II antagonists. Lozartan.
The ATC code
C09CA01
Pharmacological properties
/p>
Pharmacodynamics
Mechanism of action
Angiotensin II is a potent vasoconstrictor, the principal active hormone of the renin-angiotensin-aldosterone system (RAAS), and a crucial pathophysiological link in the development of arterial hypertension (AH). Angiotensin II binds to AT1 receptors located in many tissues (vascular smooth muscle tissues, adrenal, kidney and heart) and performs several important biological functions, including vasoconstriction and aldosterone release. In addition, angiotensin II stimulates smooth muscle cell overgrowth. AT2 receptors are the second type of receptors that angiotensin II binds to, but its role in the regulation of cardiovascular function is unknown.
Lozartan is a selective AT1-receptor antagonist of angiotensin II that is highly effective when taken orally. Losartan and its pharmacologically active carboxylated metabolite (E-3174) both in vitro and in vivo block all physiological effects of angiotensin II regardless of its source or synthesis pathway. Unlike some peptide angiotensin II antagonists, losartan does not have agonist properties.
Losartan selectively binds to AT1 receptors and does not bind to or block receptors for other hormones and ion channels that play an important role in regulating cardiovascular function. In addition, losartan does not inhibit angiotensin-converting enzyme (ACE, kininase II), which is responsible for bradykinin degradation. Consequently, effects not directly related to AT1 receptor blockade, such as increased bradykinin-mediated effects or the development of edema (losartan 1.7%, placebo 1.9%), are not relevant to the effects of losartan.
Lozartan suppresses systolic and diastolic blood pressure (BP) elevations with angiotensin II infusion. At the time of reaching the maximum plasma concentration of losartan (Cmax) after a 100 mg dose of losartan, the above effect of angiotensin II is suppressed by approximately 85%, and by 26-39% after 24 hours of single and multiple doses.
While taking losartan, the elimination of the negative feedback of angiotensin II suppression of renin secretion leads to an increase in plasma renin activity (ARP). Increase of ARP leads to increase of angiotensin II concentration in blood plasma. During long-term (6-week) treatment of patients with AH with losartan at a dose of 100 mg/day, a 2-3-fold increase in plasma angiotensin II concentrations at the time of reaching Cmax of losartan was observed. In some patients, even greater increases in angiotensin II concentrations were observed, especially with a short duration of treatment (2 weeks). Despite this, during treatment, the antihypertensive effect and decrease in plasma aldosterone concentration were evident after 2 and 6 weeks of therapy, indicating effective blockade of angiotensin II receptors. After discontinuation of losartan, ARP and angiotensin II concentrations decreased within 3 days to values observed before starting losartan. Because losartan is a specific AT1-receptor antagonist of angiotensin II, it does not inhibit ACE (kininase II), an enzyme that inactivates bradykinin. A study comparing the effects of losartan at doses of 20 mg and 100 mg with those of an ACE inhibitor for effects on angiotensin I, angiotensin II, and bradykinin showed that losartan blocks the effects of angiotensin I and angiotensin II without affecting the effects of bradykinin. This is due to the specific mechanism of action of losartan. The ACE inhibitor blocked the response to angiotensin I and increased the severity of the bradykinin-dependent effects without affecting the severity of the response to angiotensin II, demonstrating the pharmacodynamic difference between losartan and ACE inhibitors. Plasma concentrations of losartan and its active metabolite, as well as the antihypertensive effect of losartan, increase with increasing drug dose. Because losartan and its active metabolite are angiotensin II receptor antagonists (ARA II), they both contribute to the antihypertensive effect.
In a study with a single dose of 100 mg of losartan that included healthy volunteers (men), oral administration of the drug on a high-salt and low-salt diet had no effect on glomerular filtration rate (GFR), effective renal plasma flow, or filtration fraction. Losartan had a natriuretic effect that was more pronounced on the low-salt diet and did not appear to be associated with suppression of early sodium reabsorption in the proximal renal tubules. Losartan also caused a transient increase in renal uric acid excretion.
In patients with AH, proteinuria (at least 2 g/24 h), without diabetes mellitus, and taking losartan for 8 weeks at a dose of 50 mg with a gradual increase to
100 mg, there was a significant reduction in proteinuria (by 42%), fractional albumin excretion and immunoglobulin (IgG). In these patients, losartan stabilized GFR and decreased filtration fraction.
In postmenopausal women with AH taking losartan in a dose of 50 mg for 4 weeks, no effect of therapy on renal and systemic prostaglandin levels was detected.
Lozartan has no effect on autonomic reflexes and no lasting effect on plasma norepinephrine concentrations.
In patients with AH, losartan at doses up to 150 mg daily did not cause clinically significant changes in fasting triglyceride, total cholesterol, and high-density lipoprotein cholesterol concentrations. At similar doses, losartan had no effect on fasting blood glucose concentration.
The HEAAL clinical trial to evaluate the effect of high and low dose ARA II (losartan) on treatment outcome in patients with chronic heart failure (CHF) included patients (n = 3834) with CHF (NYHA functional class II-IV) and ACE inhibitor intolerance. Patients were followed more than 4 years (median follow-up was 4.7 years) to compare the effects of losartan at a dose of 50 mg/day and at a dose of 150 mg/day on reducing all-cause mortality or hospitalization for heart failure. This study showed that losartan at a dose of 150 mg/day significantly reduced the risk of all-cause mortality or hospitalization for heart failure compared with a dose of 50 mg/day (hazard ratio [OR] 0.899, p = 0.027).
In general, losartan caused a reduction in serum uric acid concentration (generally less than 0.4 mg/dL) that persisted with long-term treatment. In controlled clinical trials with patients with AH, there have been no reported cases of withdrawal of losartan due to increased serum creatinine or potassium concentrations.
In a 12-week parallel study that included patients with left ventricular failure (NYHA functional class II-IV), most of whom were taking diuretics and/or cardiac glycosides, the effects of losartan at doses of 2.5, 10, 25, and 50 mg/day were compared with placebo. At doses of 25 and 50 mg/day, losartan exhibited positive hemodynamic and neurohormonal effects that persisted throughout the study. Hemodynamic effects included an increase in cardiac index and a decrease in pulmonary capillary congestion pressure, as well as a decrease in total peripheral vascular resistance, mean systemic BP, and heart rate. The incidence of arterial hypotension in these patients depended on the dose of losartan. Neurohormonal effects included decreased aldosterone and norepinephrine blood concentrations.
Pharmacokinetics
absorption
In oral administration, losartan is well absorbed and metabolized at
“primary passage” through the liver to form the active carboxylated metabolite and inactive metabolites. Systemic bioavailability of losartan in tablet form is approximately 33%. Mean maximum concentrations (Cmax) of losartan and its active metabolite are reached after 1 h and 3-4 h, respectively. No clinically significant effect on the plasma concentration profile of losartan has been identified when losartan is taken with a normal meal.
Distribution
Lozartan and its active metabolite bind to plasma proteins (mainly to albumin) by more than 99%. The volume of distribution of losartan is 34 liters. Studies in rats have shown that losartan has almost no penetration through the blood-brain barrier.
Metabolism
About 14% of losartan is converted to its active metabolite when administered intravenously and when taken orally. After intravenous or intravenous administration of radioactive carbon-labeled losartan (14C losartan), the radioactivity of circulating blood plasma is primarily due to the presence of losartan and its active metabolite. Low conversion efficiency of losartan to its active metabolite was observed in approximately 1% of patients in the study.
In addition to the active metabolite, biologically inactive metabolites are formed, including two major metabolites formed by hydroxylation of the side butyl chain and one minor metabolite, N-2-tetrazol-glucuronide.
Elimation
Plasma clearance of losartan and its active metabolite is approximately 600 ml/min and 50 ml/min, respectively. Renal clearance of losartan and its active metabolite is approximately 74 mL/min and 26 mL/min, respectively.
When losartan is ingested, approximately 4% of the dose is excreted unchanged by the kidneys and approximately 6% of the dose is excreted by the kidneys as the active metabolite. Losartan and its active metabolite have linear pharmacokinetics with oral administration of losartan up to 200 mg.
After oral administration, plasma concentrations of losartan and its active metabolite decrease polyexponentially with a terminal elimination half-life of approximately 2 and 6-9 hours, respectively. There is no significant plasma accumulation of either losartan or its active metabolite when the drug is dosed 100 mg once daily.
Losartan and its metabolites are eliminated by the kidneys and through the intestine with bile. After oral administration of 14C losartan in men, about 35% radioactivity is detected in urine and 58% in feces. After intravenous administration of 14C losartan in men, approximately 43% of radioactivity is detectable in urine and 50% in feces.
Pharmacokinetics in special patient groups
Elderly patients
Plasma concentrations of losartan and its active metabolite in elderly male patients with arterial hypertension are not significantly different from those in younger male patients with AH.
Gender
The plasma concentrations of losartan in women with AH were twice as high as in men with AH. Concentrations of the active metabolite did not differ between men and women. This apparent pharmacokinetic difference, however, has no clinical significance.
Patients with impaired liver function
Patients with mild and moderate alcoholic cirrhosis taking losartan orally had plasma concentrations of losartan and its active metabolite 5 and 1.7 times higher than those of young healthy male volunteers, respectively.
Patients with impaired renal function
Plasma concentrations of losartan in patients with a creatinine clearance (CK) above 10 mL/min were not different from those in patients with unchanged renal function. The area under the concentration-time curve (AUC) of losartan in patients on hemodialysis was approximately 2-fold greater compared to the AUC of losartan in patients with normal renal function. Plasma concentrations of the active metabolite were not altered in patients with impaired renal function or patients on hemodialysis. Losartan and its active metabolite are not excreted by hemodialysis.
Indications
Indications
arterial hypertension;
reducing the risk of associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy, manifested by a cumulative reduction in the incidence of cardiovascular mortality, stroke and myocardial infarction;
kidney protection in patients with type 2 diabetes mellitus with proteinuria – slowing the progression of renal failure, manifested by a decrease in the incidence of hypercreatininemia, the incidence of end-stage chronic renal failure requiring hemodialysis or kidney transplantation, mortality rates, as well as a decrease in proteinuria;
chronic heart failure with ineffective treatment with ACE inhibitors or intolerance to ACE inhibitors. It is not recommended to transfer patients with heart failure and stable indicators while taking ACE inhibitors to losartan therapy.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Drugs affecting the renin-angiotensin system. Angiotensin II antagonists. Losartan.
ATC code
C09CA01
Pharmacological properties
Pharmacodynamics
Mechanism of action
Angiotensin II is a powerful vasoconstrictor, the main active hormone of the renin-angiotensin-aldosterone system (RAAS), and also a decisive pathophysiological link in the development of arterial hypertension (AH). Angiotensin II binds to AT1 receptors found in many tissues (vascular smooth muscle, adrenal glands, kidneys, and heart) and has several important biological functions, including vasoconstriction and aldosterone release. In addition, angiotensin II stimulates the proliferation of smooth muscle cells. AT2 receptors are the second type of receptor to which angiotensin II binds, but its role in regulating cardiovascular function is unknown.
Losartan is a selective antagonist of angiotensin II AT1 receptors, highly effective when taken orally. Losartan and its pharmacologically active carboxylated metabolite (E-3174) both in vitro and in vivo block all physiological effects of angiotensin II, regardless of its source or route of synthesis. Unlike some peptide angiotensin II antagonists, losartan does not have agonist properties.
Losartan selectively binds to AT1 receptors and does not bind to or block receptors of other hormones and ion channels that play an important role in regulating the function of the cardiovascular system. In addition, losartan does not inhibit angiotensin-converting enzyme (ACE, kininase II), which is responsible for the destruction of bradykinin. Therefore, effects not directly related to AT1 receptor blockade, such as increased bradykinin-mediated effects or the development of edema (losartan 1.7%, placebo 1.9%), are not related to the action of losartan.
Losartan suppresses the increase in systolic and diastolic blood pressure (BP) during infusion of angiotensin II. At the moment of reaching the maximum concentration of losartan in the blood plasma (Cmax) after taking losartan at a dose of 100 mg, the above effect of angiotensin II is suppressed by approximately 85%, and 24 hours after single and multiple doses – by 26-39%.
During the period of taking losartan, elimination of the negative feedback, which consists in the suppression of renin secretion by angiotensin II, leads to an increase in plasma renin activity (PRA). An increase in APP leads to an increase in the concentration of angiotensin II in the blood plasma. With long-term (6-week) treatment of patients with hypertension with losartan at a dose of 100 mg/day, a 2-3-fold increase in the concentration of angiotensin II in the blood plasma was observed at the time the losartan Cmax was reached. In some patients, an even greater increase in angiotensin II concentrations was observed, especially with a short duration of treatment (2 weeks). Despite this, during treatment, an antihypertensive effect and a decrease in plasma aldosterone concentrations appeared after 2 and 6 weeks of therapy, indicating effective blockade of angiotensin II receptors. After discontinuation of losartan, ARP and angiotensin II concentrations decreased within 3 days to the values observed before the start of losartan administration. Since losartan is a specific antagonist of angiotensin II AT1 receptors, it does not inhibit ACE (kininase II), an enzyme that inactivates bradykinin. A study comparing the effects of losartan at doses of 20 mg and 100 mg with the effects of an ACE inhibitor on angiotensin I, angiotensin II and bradykinin showed that losartan blocked the effects of angiotensin I and angiotensin II without affecting the effects of bradykinin. This is due to the specific mechanism of action of losartan. The ACE inhibitor blocked responses to angiotensin I and increased the effects due to bradykinin without affecting the response to angiotensin II, demonstrating a pharmacodynamic difference between losartan and ACE inhibitors. Plasma concentrations of losartan and its active metabolite, as well as the antihypertensive effect of losartan, increase with increasing dose of the drug. Since losartan and its active metabolite are angiotensin II receptor antagonists (ARA II), they both contribute to the antihypertensive effect.
In a study with a single dose of 100 mg losartan, which included healthy volunteers (men), oral administration of the drug under conditions of a high- and low-salt diet did not affect the glomerular filtration rate (GFR), effective renal plasma flow and filtration fraction. Losartan had a natriuretic effect that was more pronounced with a low-salt diet and did not appear to be associated with suppression of early sodium reabsorption in the proximal renal tubules. Losartan also caused a transient increase in renal excretion of uric acid.
In patients with hypertension, proteinuria (at least 2 g/24 hours), without diabetes mellitus and taking losartan for 8 weeks at a dose of 50 mg with a gradual increase to
100 mg, a significant decrease in proteinuria (by 42%), fractional excretion of albumin and immunoglobulins (IgG) was observed. In these patients, losartan stabilized GFR and reduced the filtration fraction.
In postmenopausal women with hypertension who took losartan at a dose of 50 mg for 4 weeks, there was no effect of therapy on the renal and systemic levels of prostaglandins.
Losartan does not affect autonomic reflexes and does not have a long-term effect on the concentration of norepinephrine in the blood plasma.
In patients with hypertension, losartan in doses up to 150 mg per day did not cause clinically significant changes in the concentration of fasting triglycerides, total cholesterol and high-density lipoprotein cholesterol. At the same doses, losartan had no effect on fasting blood glucose concentrations.
The HEAAL clinical trial to evaluate the effect of high and low doses of ARB II (losartan) on the outcome of treatment in patients with chronic heart failure (CHF) included patients (n = 3834) with CHF (II-IV functional class according to the NYHA classification) and intolerance to ACE inhibitors. Patients were followed for more than 4 years (median follow-up 4.7 years) to compare the effects of losartan 50 mg/day and 150 mg/day on reducing all-cause mortality or hospitalization for heart failure. This study showed that losartan 150 mg/day significantly reduced the risk of all-cause mortality or hospitalization for heart failure compared with 50 mg/day (hazard ratio [HR] 0.899, P = 0.027).
In general, losartan caused a decrease in serum uric acid concentrations (usually less than 0.4 mg/dL), which persisted with long-term treatment. In controlled clinical studies involving patients with hypertension, no cases of losartan withdrawal due to an increase in creatinine concentration or serum potassium levels were recorded.
In a 12-week parallel study, which included patients with left ventricular failure (NYHA functional class II-IV), most of whom were taking diuretics and/or cardiac glycosides, the effects of losartan at doses of 2.5, 10, 25 and 50 mg/day were compared with placebo. At doses of 25 and 50 mg/day, losartan exhibited positive hemodynamic and neurohormonal effects that persisted throughout the study. Hemodynamic effects included an increase in cardiac index and a decrease in pulmonary capillary wedge pressure, as well as a decrease in total peripheral vascular resistance, mean systemic blood pressure, and heart rate. The incidence of arterial hypotension in these patients depended on the dose of losartan. Neurohormonal effects included a decrease in the concentration of aldosterone and norepinephrine in the blood.
Pharmacokinetics
Suction
When taken orally, losartan is well absorbed and is metabolized by
“primary passage” through the liver with the formation of an active carboxylated metabolite and inactive metabolites. The systemic bioavailability of losartan in tablet form is approximately 33%. The average maximum concentrations (Cmax) of losartan and its active metabolite are reached after 1 hour and after 3-4 hours, respectively. When taking losartan with a normal meal, there was no clinically significant effect on the plasma concentration profile of losartan.
Distribution
Losartan and its active metabolite are more than 99% bound to plasma proteins (mainly albumin). The volume of distribution of losartan is 34 liters. Studies on rats have shown that losartan practically does not penetrate the blood-brain barrier.
Metabolism
Approximately 14% of losartan when administered intravenously and when taken orally is converted into its active metabolite. Following oral or intravenous administration of radioactive carbon-labeled losartan (14C losartan), the radioactivity of circulating blood plasma is primarily due to the presence of losartan and its active metabolite. Low efficiency of conversion of losartan to its active metabolite was observed in approximately 1% of patients participating in the study.
In addition to the active metabolite, biologically inactive metabolites are formed, including two major metabolites formed as a result of hydroxylation of the butyl side chain, and one minor one – N-2-tetrazole glucuronide.
Withdrawal
Plasma clearance of losartan and its active metabolite is about 600 ml/min and 50 ml/min, respectively. The renal clearance of losartan and its active metabolite is approximately 74 ml/min and 26 ml/min, respectively.
When losartan is taken orally, about 4% of the dose is excreted unchanged by the kidneys and about 6% of the dose is excreted by the kidneys in the form of an active metabolite. Losartan and its active metabolite have linear pharmacokinetics when losartan is taken orally in doses up to 200 mg.
After oral administration, plasma concentrations of losartan and its active metabolite decrease polyexponentially with a terminal half-life of approximately 2 and 6-9 hours, respectively. With a dosage regimen of 100 mg once a day, there is no significant accumulation of either losartan or its active metabolite in the blood plasma.
Losartan and its metabolites are excreted by the kidneys and through the intestines with bile. After oral administration of 14C losartan in men, about 35% of radioactivity is found in urine and 58% in feces. After intravenous administration of 14C losartan in men, approximately 43% of radioactivity is found in urine and 50% in feces.
Pharmacokinetics in special groups of patients
Elderly patients
Concentrations of losartan and its active metabolite in blood plasma in elderly male patients with arterial hypertension do not differ significantly from these indicators in young male patients with hypertension.
Gender
The values of losartan concentrations in blood plasma in women with hypertension were 2 times higher than the corresponding values in men with hypertension. Concentrations of the active metabolite did not differ between men and women. This apparent pharmacokinetic difference is, however, not clinically significant.
Patients with liver dysfunction
When losartan was taken orally by patients with mild to moderate alcoholic cirrhosis, the concentrations of losartan and its active metabolite in the blood plasma were 5 and 1.7 times higher, respectively, than in young healthy male volunteers.
Patients with impaired renal function
Plasma concentrations of losartan in patients with creatinine clearance (CC) above 10 ml/min did not differ from those in patients with unchanged renal function. The area under the concentration-time curve (AUC) of losartan in patients on hemodialysis was approximately 2 times greater than the AUC of losartan in patients with normal renal function. Plasma concentrations of the active metabolite did not change in patients with impaired renal function or patients on hemodialysis. Losartan and its active metabolite are not removed by hemodialysis.
Special instructions
Special instructions
Hypersensitivity reactions
In patients with a history of angioedema (swelling of the face, lips, pharynx/larynx and/or tongue), monitoring of the use of the drug is necessary (see section “Side effects”).
Embryotoxicity
The use of drugs that affect the RAAS in the second and third trimester of pregnancy reduces fetal renal function and increases morbidity and mortality of the fetus and newborns. The development of oligohydramnios may be associated with fetal lung hypoplasia and skeletal deformities. Possible adverse events in neonates include calvarial hypoplasia, anuria, hypotension, renal failure and death. If pregnancy is diagnosed, the drug should be discontinued immediately (see section
“Use during pregnancy and breastfeeding”)
Arterial hypotension and water-electrolyte imbalance or decreased circulating blood volume
In patients with reduced blood volume (for example, those receiving treatment with large doses of diuretics), symptomatic arterial hypotension may occur. Correction of such conditions must be carried out before prescribing losartan or starting treatment with a lower dose of losartan (see section “Method of administration and dosage”).
Impaired water and electrolyte balance is typical for patients with impaired renal function with or without diabetes mellitus, so careful monitoring of these patients is necessary. In clinical trials in patients with type 2 diabetes mellitus with proteinuria, the incidence of hyperkalemia was greater in the losartan group than in the placebo group. Several patients discontinued therapy due to hyperkalemia (see sections “Side effects”, “Laboratory and instrumental data”).
During treatment with losartan, it is not recommended to take potassium-sparing diuretics, potassium supplements, or potassium-containing salt substitutes.
Aortic or mitral stenosis, hypertrophic obstructive cardiomyopathy
Like all drugs that have a vasodilating effect, ARA II should be prescribed with caution to patients with aortic or mitral stenosis or hypertrophic obstructive cardiomyopathy.
Ischemic heart disease and cerebrovascular diseases
Like all drugs that have a vasodilating effect, ARA II should be prescribed with caution to patients with coronary heart disease or cerebrovascular diseases, since an excessive decrease in blood pressure in this group of patients can lead to the development of myocardial infarction or stroke.
Chronic heart failure
As with the use of other drugs that act on the RAAS, in patients with CHF and with or without impaired renal function, there is a risk of developing severe arterial hypotension or acute renal impairment.
Since there is insufficient experience with the use of losartan in patients with heart failure and concomitant severe renal impairment, in patients with severe heart failure (NYHA functional class IV), as well as in patients with heart failure and symptomatic life-threatening arrhythmias, losartan should be prescribed with caution.
Primary hyperaldosteronism
Because patients with primary hyperaldosteronism generally do not respond well to antihypertensive agents that act by inhibiting the RASS, the use of losartan is not recommended in this group of patients.
Liver dysfunction
Data from pharmacokinetic studies indicate that the plasma concentration of losartan in patients with cirrhosis is significantly increased, therefore patients with a history of impaired liver function should be prescribed losartan at a lower dose. There is no experience with the use of losartan in patients with severe liver dysfunction, so the drug should not be used in this group of patients (see sections “Pharmacological properties”, “Pharmacokinetics”,
“Contraindications”, “Method of administration and dosage”).
Impaired kidney function
Due to inhibition of the RAAS, changes in renal function, including the development of renal failure, have been observed in some predisposed patients. These changes in renal function may return to normal after treatment is stopped.
Some drugs that affect the RAAS may increase blood urea and serum creatinine concentrations in patients with bilateral renal artery stenosis or arterial stenosis of a solitary kidney. Similar effects have been reported with losartan. Such changes in renal function may be reversible after discontinuation of therapy. Losartan should be used with caution in patients with bilateral renal artery stenosis or renal artery stenosis of a solitary kidney.
Special groups of patients. Race.
Analysis of data from the entire population of patients included in the LIFE study to study the effect of losartan on reducing the incidence of the study’s main composite criterion in patients with hypertension and left ventricular hypertrophy (n = 9193), showed that the ability of losartan, compared with atenolol, to reduce the risk of stroke and myocardial infarction, as well as reduce the rate of cardiovascular mortality in patients with hypertension and left ventricular hypertrophy (by 13.0%, p = 0.021) does not apply to patients of the Negroid race, although both treatment regimens effectively reduced blood pressure in these patients. In this study, losartan, compared with atenolol, reduced cardiovascular morbidity and mortality in patients with hypertension and left ventricular hypertrophy of all races except blacks (n = 8660, p = 0.003). However, in this study, black patients receiving atenolol had a lower risk of the study’s primary composite endpoint (i.e., lower composite incidence of cardiovascular death, stroke, and myocardial infarction) compared with race-matched patients receiving losartan (p = 0.03).
Children and teenagers
The effectiveness and safety of losartan in children and adolescents under 18 years of age have not been established.
If oliguria or arterial hypotension develops in newborns whose mothers took losartan during pregnancy, symptomatic therapy aimed at maintaining blood pressure and renal perfusion is necessary. Blood transfusions or dialysis may be required to prevent hypotension and/or maintain renal function.
Elderly patients
Clinical studies have not revealed any particularities regarding the safety and effectiveness of losartan in elderly patients (over 65 years of age).
Influence on the ability to drive vehicles and machinery
No studies have been conducted to evaluate the effect on the ability to drive or operate machines, but caution should be exercised when using antihypertensive therapy and driving or operating machines, as dizziness and drowsiness may develop, especially at the beginning of therapy or when the dose is increased.
Active ingredient
Active ingredient
Losartan
Composition
Composition
Dosage 50 mg
active ingredient: losartan potassium – 50.0 mg;
excipients: lactose monohydrate – 57.5 mg; microcrystalline cellulose – 20.0 mg; croscarmellose sodium – 5.6 mg; povidone K-17 (low molecular weight polyvinylpyrrolidone) – 4.5 mg; colloidal silicon dioxide – 1.0 mg; magnesium stearate – 1.4 mg;
film coating: [hypromellose – 2.4 mg, talc – 0.8 mg, titanium dioxide – 0.44 mg, macrogol 4000 (polyethylene glycol 4000) – 0.36 mg] or [dry mixture for film coating containing hypromellose (60%), talc (20%), titanium dioxide (11%), macrogol 4000 (polyethylene glycol 4000) (9%)] − 4.0 mg.
Pregnancy
Pregnancy
Medicines that act directly on the RAAS can cause serious damage and death to the developing fetus, therefore, when pregnancy is diagnosed, the drug should be immediately discontinued and, if necessary, alternative antihypertensive therapy should be prescribed.
Pregnancy
Losartan therapy should not be started during pregnancy. If continued therapy with losartan is considered necessary in patients planning pregnancy, losartan should be replaced with alternative antihypertensive agents that have an established safety profile for use during pregnancy.
Although there is no experience with the use of losartan in pregnant women, preclinical studies in animals have shown that administration of losartan leads to the development of serious fetal and neonatal damage and death of the fetus or offspring. It is believed that the mechanism of these phenomena is due to the effect on the RAAS.
Fetal renal perfusion, which is dependent on the development of the RAAS, appears in the second trimester, so the risk to the fetus increases if losartan is used in the second or third trimester of pregnancy.
The use of drugs that affect the RAAS in the second and third trimester of pregnancy reduces fetal renal function and increases morbidity and mortality of the fetus and newborns. The development of oligohydramnios may be associated with fetal lung hypoplasia and skeletal deformities. Possible adverse events in newborns include calvarial hypoplasia, anuria, hypotension, renal failure and death.
The above undesirable outcomes are usually caused by the use of drugs that affect the RAAS in the second and third trimester of pregnancy. Most epidemiological studies examining the development of fetal abnormalities following the use of antihypertensive drugs in the first trimester of pregnancy have found no differences between drugs acting on the RAAS and other antihypertensive drugs. When prescribing antihypertensive therapy to pregnant women, it is important to optimize possible outcomes for the mother and fetus.
If it is impossible to select an alternative therapy instead of therapy with drugs that affect the RAAS, it is necessary to inform the patient about the possible risk of therapy to the fetus. Periodic ultrasound examinations are necessary to assess the intra-amniotic space. If oligohydramnios is detected, losartan should be discontinued unless it is essential for the mother. Depending on the week of pregnancy, appropriate fetal tests are necessary. Patients and clinicians should be aware that oligohydramnios may not be detected until irreversible fetal damage occurs. Neonates whose mothers took losartan during pregnancy should be closely monitored to monitor for hypotension, oliguria, and hyperkalemia.
Breastfeeding period
It is not known whether losartan is excreted in breast milk. Since many drugs are excreted in breast milk and there is a risk of possible adverse effects in a breastfed baby, a decision should be made to stop breastfeeding or discontinue the drug, taking into account the need for the mother.
Contraindications
Contraindications
hypersensitivity to losartan and other components of the drug;
simultaneous use with angiotensin-converting enzyme (ACE) inhibitors in patients with diabetic nephropathy;
simultaneous use with aliskiren and drugs containing aliskiren in patients with diabetes mellitus and/or moderate or severe renal impairment (glomerular filtration rate (GFR) less than 60 ml/min/1.73 m2 body surface area) (see “Interaction with other drugs”);
hereditary lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome;
severe liver dysfunction (no experience with use);
pregnancy and breastfeeding;
children under 18 years of age (efficacy and safety of use have not been established).
With caution
bilateral renal artery stenosis or stenosis of the artery of a single kidney; hyperkalemia;
conditions after kidney transplantation (no experience of use);
aortic or mitral stenosis;
hypertrophic obstructive cardiomyopathy;
heart failure with concomitant severe renal impairment;
severe heart failure (functional class IV according to the NYHA classification);
heart failure with life-threatening arrhythmias;
coronary heart disease;
cerebrovascular diseases;
primary hyperaldosteronism;
history of angioedema;
Patients with reduced circulating blood volume (for example, those receiving treatment with large doses of diuretics) may experience symptomatic arterial hypotension.
Side Effects
Side Effects
Classification of the frequency of side effects according to the recommendations of the World Health Organization (WHO):
very often ≥ 1/10;
often from ≥ 1/100 to < 1/10; infrequently from ≥ 1/1000 to < 1/100; rarely from ≥ 1/10000 to <1/1000;
very rare <1/10000, including individual messages;
frequency unknown – based on available data, it is not possible to determine the frequency of occurrence.
In general, losartan is well tolerated by patients with hypertension. Adverse events (AEs) are mild and transient in nature and do not require discontinuation of the drug. The total incidence of AEs when taking losartan is comparable to this indicator when taking placebo. In controlled clinical trials, the rate of discontinuation of therapy due to clinically significant AEs was 2.3% in the group of patients taking losartan and 3.7% in the group of patients taking placebo.
In controlled clinical trials of losartan in patients with hypertension, the following AEs were observed.
Nervous system disorders:
often – dizziness;
uncommon – drowsiness, headache, sleep disturbances.
Disorders of the hearing organ and labyrinth:
often – systemic dizziness (vertigo).
Heart disorders:
uncommon – palpitations, angina pectoris.
Vascular disorders:
uncommon – (orthostatic) hypotension (including dose-mediated orthostatic effects) (especially in patients with reduced volume, for example, in patients with severe heart failure or patients treated with high doses of diuretics).
Gastrointestinal disorders:
Uncommon – abdominal pain, constipation.
Skin and subcutaneous tissue disorders:
uncommon – skin rash.
General disorders and reactions at the injection site:
uncommon – weakness, increased fatigue, swelling.
Laboratory and instrumental data:
often – hyperkalemia;
rarely – increased alanine aminotransferase (ALT) activity (usually returned to normal after discontinuation of therapy).
Controlled clinical studies have shown that losartan is generally well tolerated in patients with hypertension and left ventricular hypertrophy. The following AEs were observed in these studies:
Nervous system disorders:
often – dizziness.
Hearing and labyrinthine disorders:
often – systemic dizziness (vertigo).
General disorders and reactions at the injection site:
uncommon – weakness, increased fatigue.
In the LIFE study, in patients without a history of diabetes mellitus, the incidence of new onset diabetes mellitus was lower with losartan compared with atenolol (p < 0.001). Since this study did not include a placebo group, it is unknown whether this is a beneficial effect of losartan or an adverse effect of atenolol. Controlled clinical studies have shown that losartan is generally well tolerated in patients with type 2 diabetes mellitus and proteinuria. The following AEs were observed in these studies:
Nervous system disorders:
often – dizziness.
Vascular disorders:
often – (orthostatic) hypotension (including dose-mediated orthostatic effects) (especially in patients with reduced blood volume, for example, in patients with severe heart failure or patients treated with high doses of diuretics).
General disorders and reactions at the injection site:
uncommon – weakness, increased fatigue.
Laboratory and instrumental data:
often – hyperkalemia (in a clinical study involving patients with type 2 diabetes mellitus and nephropathy, hyperkalemia (more than 5.5 mmol/l) was observed in 9.9% of patients taking losartan and in 3.4% of patients taking placebo), hypoglycemia.
Controlled clinical studies have shown that losartan is generally well tolerated by patients with CHF. AEs observed during clinical trials were typical for this group of patients.
Blood and lymphatic system disorders:
often – anemia.
Nervous system disorders:
often – dizziness; infrequently – headache; rarely – paresthesia.
Heart disorders:
rarely – fainting, atrial fibrillation, cerebrovascular accident.
Vascular disorders:
often – (orthostatic) hypotension (including dose-mediated orthostatic effects) (especially in patients with reduced blood volume, for example, in patients with severe heart failure or patients treated with high doses of diuretics).
Disorders of the respiratory system, chest and mediastinal organs: uncommon – shortness of breath, cough.
Gastrointestinal disorders:
uncommon – diarrhea, nausea, vomiting.
Skin and subcutaneous tissue disorders:
uncommon – urticaria, skin itching, skin rash.
Disorders of the kidneys and urinary tract:
often – renal dysfunction, renal failure.
General disorders and reactions at the injection site:
uncommon – weakness, increased fatigue.
Laboratory and instrumental data:
often – an increase in the concentration of creatinine, urea and potassium in the blood; uncommon – hyperkalemia (more common in patients taking losartan at a dose of 150 mg per day than in patients taking losartan at a dose of 50 mg per day).
The following AEs were observed in clinical practice during the post-registration period.
Blood and lymphatic system disorders:
frequency unknown – anemia, thrombocytopenia.
Immune system disorders:
rarely – hypersensitivity reactions, anaphylactic reactions, angioedema (including angioedema of the larynx, pharynx, face, lips, pharynx and/or tongue (causing airway obstruction); some of these patients had a history of angioedema when taking other drugs (including ACE inhibitors), vasculitis (including purpura Schönlein-Henoch).
Mental disorders:
frequency unknown – depression.
Nervous system disorders:
frequency unknown – migraine, dysgeusia.
Disorders of the hearing organ and labyrinth:
frequency unknown – tinnitus.
Disorders of the respiratory system, chest and mediastinal organs:
frequency unknown – cough.
Gastrointestinal disorders:
frequency unknown – diarrhea, pancreatitis.
Disorders of the liver and biliary tract:
rarely – hepatitis;
frequency unknown – liver dysfunction.
Skin and subcutaneous tissue disorders:
frequency unknown – urticaria, itching, rash, photosensitivity. Muscular, skeletal and connective tissue disorders: frequency unknown – myalgia, arthralgia, rhabdomyolysis.
Disorders of the reproductive system and mammary gland:
frequency unknown – erectile dysfunction/impotence.
General disorders and reactions at the injection site:
frequency unknown – general malaise.
Laboratory and instrumental data:
frequency unknown – hyponatremia.
Interaction
Interaction
In clinical studies studying pharmacokinetic drug interactions, no clinically significant interactions of losartan with hydrochlorothiazide, digoxin, warfarin, cimetidine and phenobarbital were identified.
Rifampicin, being an inducer of drug metabolism, reduces the concentration of the active metabolite of losartan in the blood.
In clinical studies, the use of two inhibitors of the P450 3A4 isoenzyme was studied: ketoconazole and erythromycin. Ketoconazole did not affect the metabolism of losartan to the active metabolite after intravenous administration of losartan, and erythromycin did not have a clinically significant effect when losartan was taken orally. Fluconazole, an inhibitor of the P450 2C9 isoenzyme, reduces the concentration of the active metabolite of losartan, but the pharmacodynamic significance of the simultaneous use of losartan and inhibitors of the P450 2C9 isoenzyme has not been studied. It has been shown that patients who do not metabolize losartan into the active metabolite have a very rare and specific defect in the P450 2C9 isoenzyme. These data suggest that the metabolism of losartan to the active metabolite is carried out by the P450 2C9 isoenzyme, and not by the P450 3A4 isoenzyme.
Concomitant use of losartan, as well as other drugs that block angiotensin II or its effects, with potassium-sparing diuretics (for example, spironolactone, eplerenone, triamterene, amiloride), potassium supplements or potassium salts may lead to an increase in serum potassium.
As with the use of other drugs that affect sodium excretion, losartan may reduce lithium excretion, therefore, when using lithium preparations and ARA II simultaneously, it is necessary to carefully monitor the concentration of lithium in the blood serum.
Nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors, may reduce the effect of diuretics and other antihypertensive agents. As a result, the antihypertensive effect of ARA II or ACE inhibitors may be weakened when used simultaneously with NSAIDs, including selective COX-2 inhibitors.
In some patients with impaired renal function (for example, elderly patients or patients with dehydration, including those taking diuretics) receiving NSAID therapy, including selective COX-2 inhibitors, concomitant use of ARB II or ACE inhibitors may cause a further deterioration of renal function, including the development of acute renal failure. These effects are usually reversible, so simultaneous use of these drugs should be done with caution in patients with impaired renal function.
Dual blockade of the RAAS using ARB II, ACE inhibitors or aliskiren (renin inhibitor) is associated with an increased risk of arterial hypotension, syncope, hyperkalemia and renal dysfunction (including acute renal failure) compared with monotherapy. Regular monitoring of blood pressure, renal function and electrolyte levels in the blood is necessary in patients taking losartan and other drugs that affect the RAAS at the same time. Losartan should not be used concomitantly with aliskiren or products containing aliskiren in patients with diabetes mellitus and/or moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients. Concomitant use of losartan with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Overdose
Overdose
Information about overdose is limited.
The most likely manifestation of an overdose
Severe decrease in blood pressure and tachycardia; bradycardia may occur due to parasympathetic (vagal) stimulation. In case of development of symptomatic arterial hypotension, maintenance therapy is indicated.
Treatment
Symptomatic therapy.
Losartan and its active metabolite are not eliminated by hemodialysis.
Storage conditions
Storage conditions
Store in a place protected from light at a temperature not exceeding 25 ºС. Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Vertex, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store in a light-protected place at a temperature not exceeding 25 ºC. Keep out of reach of children. |
| Manufacturer | Vertex, Russia |
| Medication form | pills |
| Brand | Vertex |
Other forms…
Related products
Buy Losartan-Vertex, 50 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.