No products in the cart.
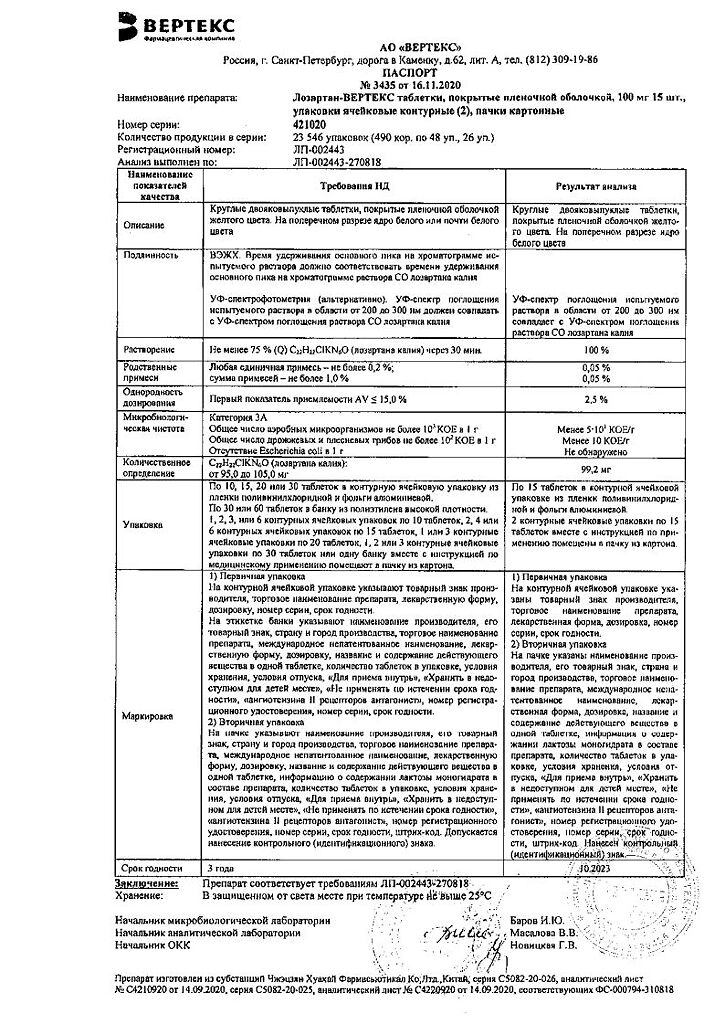
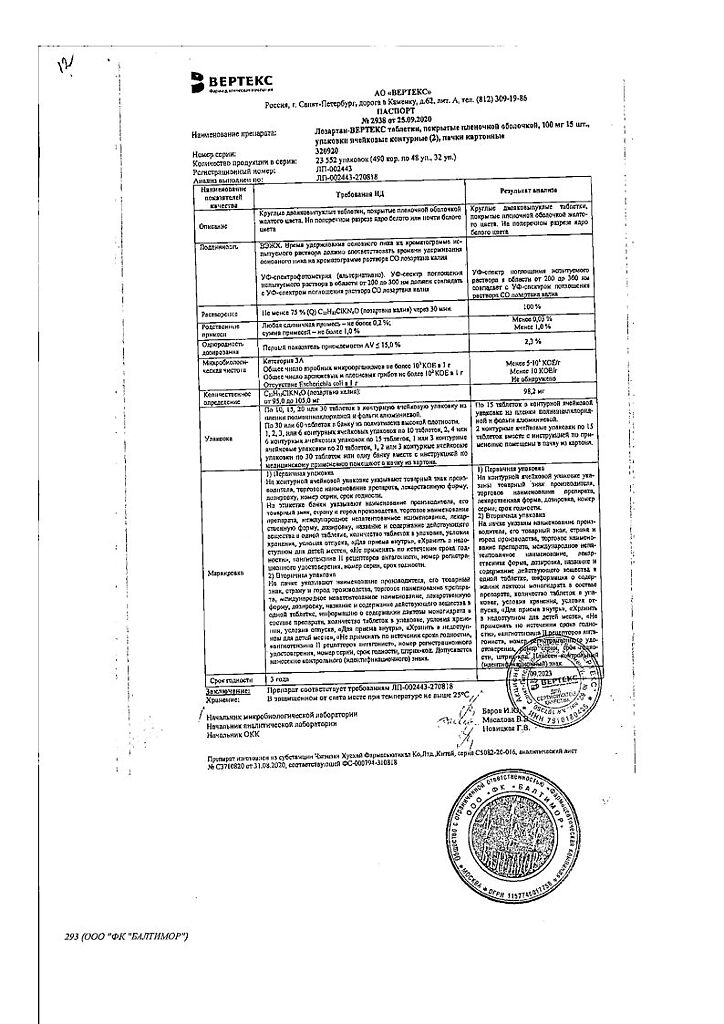
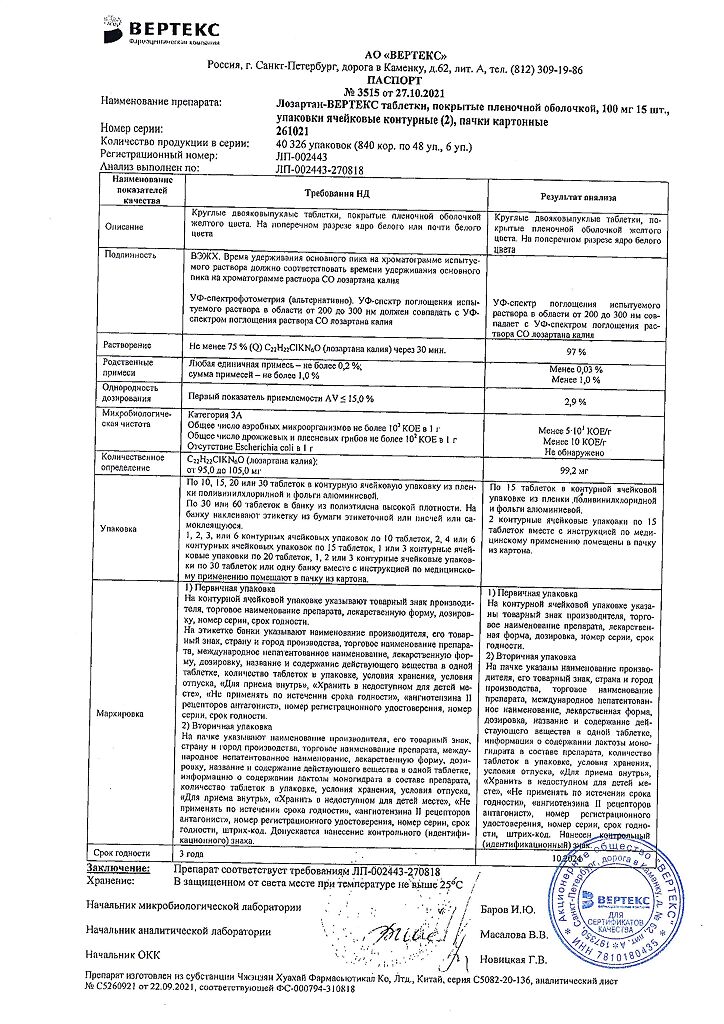
Losartan, 100 mg 30 pcs
€5.93 €5.19
Description
Pharmacotherapeutic group
An angiotensin II receptor antagonist.
ATC code
C09CA01
Pharmacological properties
Pharmacodynamics
/b>
Lozartan is a specific angiotensin II receptor antagonist (AT1 type) for oral administration. Angiotensin II selectively binds to AT1 receptors in many tissues (vascular smooth muscle tissues, adrenal glands, kidneys, and heart) and has several important biological functions including vasoconstriction and aldosterone release. Angiotensin II also stimulates smooth muscle cell overgrowth.
Lozartan and its pharmacologically active metabolite (E 3174) both in vitro and in vivo block all physiological effects of angiotensin II regardless of the source or synthesis route. Losartan selectively binds to AT1 receptors; it does not bind to or block receptors for other hormones and ion channels that play an important role in the regulation of cardiovascular function. In addition, losartan does not inhibit angiotensin-converting enzyme (ACE), which promotes bradykinin degradation, so bradykinin-mediated side effects (such as angioedema) are quite rare.
When using losartan, the lack of negative feedback effects on renin secretion results in increased plasma renin activity. Increased renin activity leads to increased plasma angiotensin II concentration.
However, antihypertensive activity and decreased plasma aldosterone concentration persist, indicating effective blockade of angiotensin II receptors. After discontinuation of losartan, plasma renin activity and angiotensin II concentrations decreased within 3 days to baseline values observed before starting the drug.
Losartan and its active metabolite have a high affinity for angiotensin II receptors (type AT1).
The plasma concentrations of losartan and its active metabolite, as well as the antihypertensive effect of losartan, increase with increasing drug dose. Maximum antihypertensive effect develops 3-6 weeks after initiation of the drug.
In patients with arterial hypertension, proteinuria (more than 2 g per day), without diabetes mellitus, use of the drug significantly reduces proteinuria, albumin and immunoglobulin G (IgG) excretion.
In postmenopausal women with arterial hypertension who received losartan at a dose of 50 mg/day for 4 weeks, no effect of therapy on renal and systemic prostaglandin levels was found.
Lozartan has no effect on autonomic reflexes and no lasting effect on plasma norepinephrine levels.
In patients with arterial hypertension, losartan at doses up to 150 mg daily does not cause clinically significant changes in triglyceride, total cholesterol and high-density lipoprotein cholesterol concentrations. At similar doses, losartan has no effect on fasting blood glucose concentrations. Lozartan has been shown to reduce serum uric acid concentrations (typically less than 0.4 mg/dL) that persists during long-term therapy. In controlled clinical trials involving patients with arterial hypertension, there have been no cases of drug withdrawal due to an increase in serum creatinine or potassium.
Pharmacokinetics
Intake
Losartan is well absorbed from the gastrointestinal tract when ingested.
The systemic bioavailability of losartan is approximately 33%; food intake does not affect the bioavailability of losartan. Mean maximum concentrations of losartan and its active metabolite are reached after 1 h and 3-4 h, respectively.
Distribution
Lozartan and its active metabolite bind to plasma proteins (mainly to albumin) by more than 99%. The volume of distribution of losartan is 34 liters. Losartan practically does not penetrate through the blood-brain barrier.
Metabolism
Lozartan undergoes a “primary passage” effect through the liver and is metabolized with the participation of cytochrome P450 isoenzyme CYP2C9. Approximately 14% of the dose of losartan administered intravenously or orally is converted to its active metabolite (EXP3174) with a carboxylic group. Biologically inactive metabolites are also formed: two major metabolites (as a result of hydroxylation of the side butyl chain) and a less significant one, N-2-tetrazol-glucuronide.
The plasma clearance of losartan and its active metabolite
is 600 ml/min and 50 ml/min, respectively. Renal clearance of losartan and its active metabolite is approximately 74 mL/min and 26 mL/min, respectively.
In oral administration of losartan, approximately 4% of the dose is excreted unchanged by the kidneys and within 6% of the dose is excreted by the kidneys as an active metabolite. Losartan and its active metabolite have linear pharmacokinetics when administered orally in doses up to 200 mg of losartan. After oral administration, plasma concentrations of losartan and its active metabolite decrease polyexponentially with final half-lives of T1/2 of approximately 2 and 6-9 h, respectively.
The excretion of losartan and its metabolites occurs in the bile and the kidneys. After ingestion of 14C-labeled losartan, approximately 35% of the radioactive label is detected in the urine and 58% in the feces.
Pharmacokinetics in Special Patient Groups
The plasma concentrations of losartan and its active metabolite in elderly male patients with arterial hypertension are not significantly different from those in younger male patients with arterial hypertension.
Plasma concentrations of losartan were 2-fold higher in women with arterial
hypertension compared to men with arterial hypertension.
Concentrations of the active metabolite did not differ in men and women. This apparent
pharmacokinetic difference has no clinical significance.
In patients with mild to moderate alcoholic cirrhosis taking losartan orally, plasma concentrations of losartan and its active metabolite were 5 and 1.7 times (respectively) higher than in young healthy male volunteers. 10 mL/min were not different from those in patients with normal renal function. In patients requiring hemodialysis, the area under the “concentration-time curve” (AUC) is approximately 2 times greater than in patients with normal renal function. Plasma concentrations of the active metabolite are unchanged in patients with impaired renal function or in patients on hemodialysis. Losartan and its active metabolite are not eliminated from the bloodstream by hemodialysis.
Indications
Indications
arterial hypertension;
Reducing the risk of associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy, as evidenced by a reduction in the combined incidence of cardiovascular mortality, stroke and myocardial infarction;
Renal protection in patients with type 2 diabetes mellitus with proteinuria – slowing the progression of renal failure, manifested by reduced incidence of hypercreatininemia, the frequency of developing end-stage chronic renal failure (CKF) requiring hemodialysis or renal transplantation, mortality rates, and reduced proteinuria;
Chronic heart failure with ineffective treatment with ACE inhibitors.
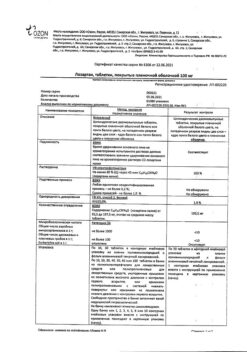
Active ingredient
Active ingredient
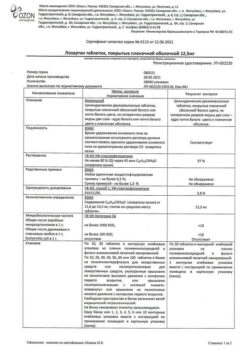
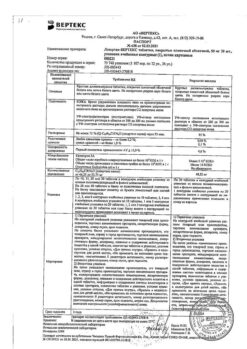
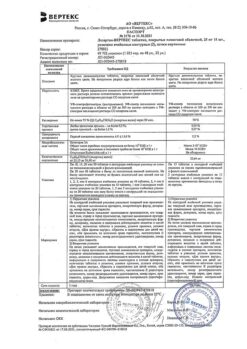
Composition
Composition
Active ingredient:
potassium losartan – 100,000 mg;
excipients:
Lactose monohydrate – 115,000 mg,
Microcrystalline cellulose – 40,000 mg,
How to take, the dosage
How to take, the dosage
Ingestion, regardless of meals.
The drug can be taken both as monotherapy and in combination with other hypotensive drugs.
Arterial hypertension
The standard starting and maintenance dose for most patients is
50 mg once daily. Maximum antihypertensive effect is achieved after 3-6 weeks of therapy.
In some patients the dose may be increased to a maximum daily dose of 100 mg once daily to achieve a greater effect.
In patients with decreased circulating blood volume (e.g., when taking high-dose diuretics), the starting dose of the drug should be reduced to 25 mg once daily (see section “Special Precautions”).
There is no need to adjust the starting dose in elderly patients and in patients with renal impairment, including dialysis patients.
Patientswith hepatic impairment (less than 9 points on the Child-Pugh scale) during hemodialysis procedure and patients older than 75 years are recommended to prescribe the drug in a lower starting dose of 25 mg once daily.
Risk reduction of associated cardiovascular morbidity and mortality in
patients with arterial hypertension and left ventricular hypertrophy
The standard initial dose of the drug is 50 mg once daily. Subsequently, it is recommended that hydrochlorothiazide be added or the dose of Lozartan be increased to 100 mg (depending on the degree of blood pressure (BP) reduction) in one or two doses.
Kidney protection in patients with type 2 diabetes mellitus and proteinuria
The standard starting dose of the drug is 50 mg once daily. Subsequently, it is recommended that the dose of Lozartan be increased to 100 mg once daily, taking into account the degree of BP reduction. Losartan may be combined with other hypotensive drugs (diuretics, slow calcium channel blockers, alpha- and beta-adrenoblockers, hypotensive drugs of central action), insulin and other hypoglycemic drugs (sulfonylurea derivatives, glitazones and glucosidase inhibitors).
Chronic heart failure
The initial dose of the drug is 12.5 mg once daily. Typically, the dose is titrated at weekly intervals (i.e., 12.5 mg once daily, 25 mg once daily, 50 mg once daily) to the usual maintenance dose of 50 mg once daily, depending on individual tolerance.
Interaction
Interaction
Can be administered with other hypotensive agents.
There are no clinically significant interactions of losartan with drugs such as hydrochlorothiazide, digoxin, warfarin, cimetidine and phenobarbital, ketoconazole and erythromycin.
Rifampicin and fluconazole decrease the level of the active metabolite. The clinical significance of these interactions has not been established.
As with other agents that block angiotensin II formation and its effects, simultaneous use of potassium-saving diuretics (e.g., spironolactone, triamterene, amiloride, eplerenone) or potassium-enhancing agents (e.g., heparin), potassium supplements and salts containing potassium may lead to increased serum potassium levels.
As with other drugs that affect sodium excretion, treatment with losartan may be accompanied by decreased sodium excretion and increased serum lithium concentrations, so serum lithium concentrations should be monitored when concomitantly treated with lithium preparations.
Non-steroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors, may decrease the effect of diuretics and other hypotensive agents. Therefore, the antihypertensive effect of angiotensin II receptor antagonists or ACE inhibitors may be weakened with concomitant use of NSAIDs, including selective COX-2 inhibitors.
In some patients with impaired renal function who were treated with NSAIDs, concomitant administration of angiotensin II antagonists may cause further deterioration of renal function. This effect is usually reversible.
Other hypotensive drugs may increase the antihypertensive effect of losartan. Concomitant use of drugs (e.g., tricyclic antidepressants, neuroleptics, baclofen, amifostine) that lower blood pressure as a primary or side effect may increase the risk of arterial hypotension.
Double RAAS blockade with angiotensin II receptor antagonists, ACE inhibitors, or aliskiren is associated with an increased risk of arterial hypotension, syncope, hyperkalemia, and renal function impairment (including acute renal failure) compared with monotherapy. Blood pressure, renal function and electrolyte balance should be carefully monitored in patients taking losartan and other drugs that affect the RAAS. Losartan should not be used concomitantly with aliskiren in patients with diabetes mellitus. Simultaneous use of losartan and aliskiren should be avoided in patients with renal impairment (glomerular filtration rate less than 60 ml/min).
There was no difference in effect when used concomitantly with fluvastatin (a weak CYP 2C9 isoenzyme inhibitor).
Consult your physician if you are prescribed losartan and you are taking other drugs.
Special Instructions
Special Instructions
Allergic reactions. Anaphylactic reactions, angioedema with involvement of the larynx and pharynx, causing airway obstruction and/or swelling of the face, lips, pharynx and/or tongue have rarely been observed in patients taking losartan. Some of these patients had a history of angioedema when taking other drugs, including ACE inhibitors. Therefore, special caution should be exercised when prescribing the drug to patients with a history of angioedema.
Arterial hypotension and impaired water-electrolyte balance or decreased RBC. Symptomatic arterial hypotension may occur in patients with decreased blood circulation (e.g., those treated with high-dose diuretics). This condition should be corrected prior to prescribing losartan or treatment should be initiated with a lower dose (see section “Dosage and administration”).
Electrolyte disturbances are common in patients with renal impairment with or without type 2 diabetes mellitus, therefore special caution should be exercised when prescribing in this population because of the risk of hyperkalemia (see section “Adverse effects”, subsection “Laboratory parameters”).
The potassium levels in blood should be monitored regularly during treatment, especially in elderly patients with impaired renal function. During treatment with losartan, patients should not take potassium supplements or salt substitutes containing potassium without first consulting their physician.
Aortic or mitral stenosis, obstructive hypertrophic cardiomyopathy. As with all drugs with vasodilatory effects, angiotensin II receptor antagonists should be prescribed with caution in patients with aortic or mitral stenosis, or obstructive hypertrophic cardiomyopathy.
Ischemic heart disease and cerebrovascular disease. As with all drugs with vasodilatory effects, angiotensin II receptor antagonists should be administered with caution in patients with ischemic heart disease or cerebrovascular disease, as excessive blood pressure lowering in this group of patients may lead to myocardial infarction or stroke.
Chronic heart failure (CHF). As with other drugs acting on the RAAS, in patients with CHF and with or without impaired renal function, there is a risk of severe arterial hypotension or acute renal failure.
There is insufficient experience with the use of losartan in patients with heart failure and concomitant severe renal impairment, in patients with severe heart failure (NYHA functional class IV), and in patients with heart failure and symptomatic life-threatening arrhythmias. Therefore, losartan should be administered with caution in these groups.
Primary hyperaldosteronism. Patients with primary hyperaldosteronism generally do not respond positively to therapy with hypotensive agents that act by inhibiting the RAAS, so the use of losartan is not recommended in this group of patients.
Hepatic impairment. The data from pharmacokinetic studies indicate that plasma concentrations of losartan are significantly increased in patients with cirrhosis, so patients with a history of liver disease should use the drug in a lower dose (see section “Dosage and administration”).
Renal dysfunction. Due to inhibition of the RAAS, renal function changes, including the development of renal failure, have been observed in some predisposed patients. These changes may go away after discontinuation of treatment.
Some drugs that affect the RAAS may increase blood urea and serum creatinine concentrations in patients with bilateral renal artery stenosis or artery stenosis of the single kidney. Changes in renal function may be reversible after therapy. Serum creatinine concentration should be monitored regularly at regular intervals during treatment.
Patients of advanced age. Clinical studies have not demonstrated any differences in safety and efficacy of losartan in elderly patients.
Impact on driving and operating ability
We should be careful during treatment about driving and engaging in other potentially hazardous activities requiring increased concentration and rapid psychomotor reactions (dizziness is possible, especially in patients who have taken diuretic drugs and have switched to therapy with the drug).
Contraindications
Contraindications
Hypersensitivity to any of the ingredients of the drug;
pregnancy and breastfeeding;
Under 18 years of age;
refractory hyperkalemia;
lactose intolerance, lactase deficiency, and glucose-galactose malabsorption syndrome;
dehydration;
severe hepatic impairment (no experience of use);
concomitant use with aliskiren in patients with diabetes and/or impaired renal function (glomerular filtration rate less than 60 ml/min).
With caution
Hepatic insufficiency (less than 9 points by Child-Pugh), arterial hypotension,
reduced circulating blood volume (CBC), impaired water-electrolyte
balance, hyperkalemia, bilateral renal artery stenosis or stenosis of the artery of the only kidney, renal failure, conditions after renal transplantation, aortic and mitral stenosis, obstructive hypertrophic cardiomyopathy, angioedema in anamnesis, severe heart failure
.br> (NYHA functional class IV), coronary heart disease, heart failure with life-threatening arrhythmias, cerebrovascular disease, primary aldosteronism, heart failure with concomitant severe renal failure.
Side effects
Side effects
In most cases, losartan is well tolerated and side effects are mild and transient and do not require withdrawal.
The side effects observed when taking the drug are classified into categories according to their frequency of occurrence: Very frequently ⥠1/10 (10%); frequently > 1/100
(1%) ⤠1/10 (10%); sometimes ⥠1/1000 (0.1%), ⤠1/100 (1%); rarely â¥1/10000 (0.01%),
⤠1/1000 (0.1%); very rarely ⤠1/10000 (0.01%), including individual events.
Back effects occurring with an incidence greater than 1%
General disorders: asthenia, weakness, increased fatigue, chest pain, peripheral edema.
Cardiovascular system disorders: palpitations, tachycardia.
Digestive system disorders: abdominal pain, diarrhea, dyspepsia, nausea.
Musculoskeletal system disorders: back pain, leg pain, muscle cramps.
Central nervous system (CNS): dizziness, headache, insomnia.
Respiratory system disorders: cough, bronchitis, nasal mucous membrane swelling, pharyngitis, sinusitis, upper respiratory tract infections.
Back effects occurring with a frequency of less than 1%
Cardiovascular system: Angina, symptomatic arterial hypotension (especially in patients with intravascular dehydration, such as patients with severe heart failure or when taking high-dose diuretics), dose-dependent orthostatic hypotension, bradycardia, arrhythmias, myocardial infarction, vasculitis.
Gastrointestinal system disorders: anorexia, dry mouth, toothache, flatulence, gastritis, constipation, hepatitis, liver function disorders, vomiting.
The skin: dry skin, ecchymosis, erythema, photosensitization, increased sweating, alopecia.
Allergic reactions: urticaria, pruritus, skin rash, angioedema (including swelling of the larynx, vocal folds, causing airway obstruction, and/or swelling of the face, lips, pharynx and/or tongue).
Hematopoietic system disorders: anemia, thrombocytopenia, eosinophilia, Schoenlein-Henoch purpura.
Nervous system and sensory system disorders: anxiety, sleep disturbance, somnolence, memory disturbance, peripheral neuropathy, paresthesia, hypoesthesia, tremor, ataxia, depression, fainting, tinnitus, taste disturbance, visual disturbance, conjunctivitis, migraine.
Motor system disorders: arthralgia, arthritis, pain in the shoulder and knee, fibromyalgia.
Urinary system disorders: imperative urge to urinate, urinary tract infections, renal dysfunction.
Reproductive system disorders: decreased libido, impotence.
Others: aggravation of the course of gout, nasal bleeding.
In terms of laboratory parameters:
often – hyperkalemia (potassium over 5.5 mmol/l);
infrequently – increased concentration of urea, residual nitrogen, serum creatinine;
very rarely – moderate increase of transaminases activity (aspartate aminotransferase, alanine aminotransferase), hyperbilirubinemia.
Please note! If any of the side effects listed in the instructions worsen or if you notice any other side effects not listed in the instructions, tell your doctor.
Overdose
Overdose
There is limited information about overdose of the drug.
The most likely symptoms
A marked decrease in BP and tachycardia; bradycardia may occur due to parasympathetic (vagus) stimulation.
Treatment
Forced diuresis, symptomatic therapy.
Neither losartan nor its active metabolite is excreted by hemodialysis.
Similarities
Similarities
Additional information
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C. |
|---|---|
| Manufacturer | Vertex, Russia |
| Medication form | pills |
| Brand | Vertex |
Other forms…
Related products
Buy Losartan, 100 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.