No products in the cart.
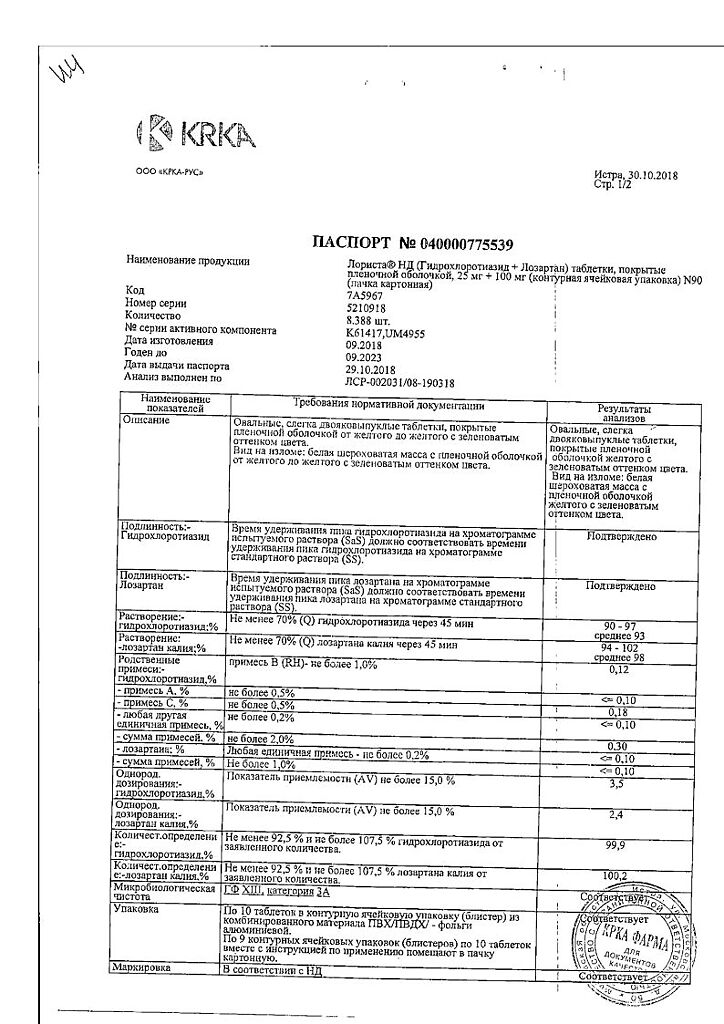
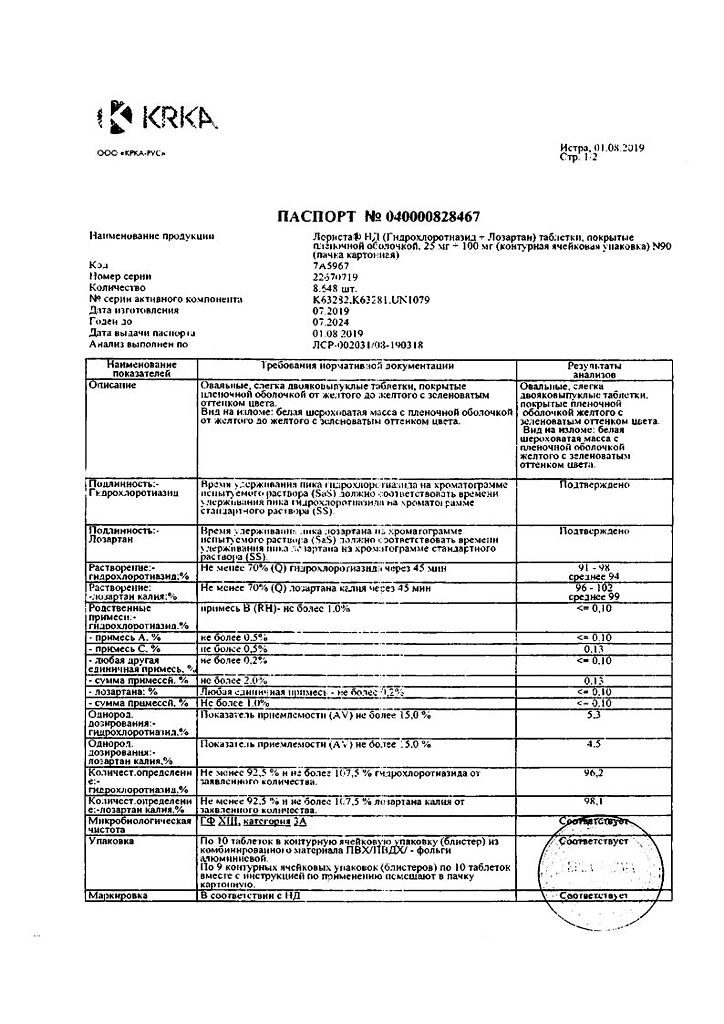
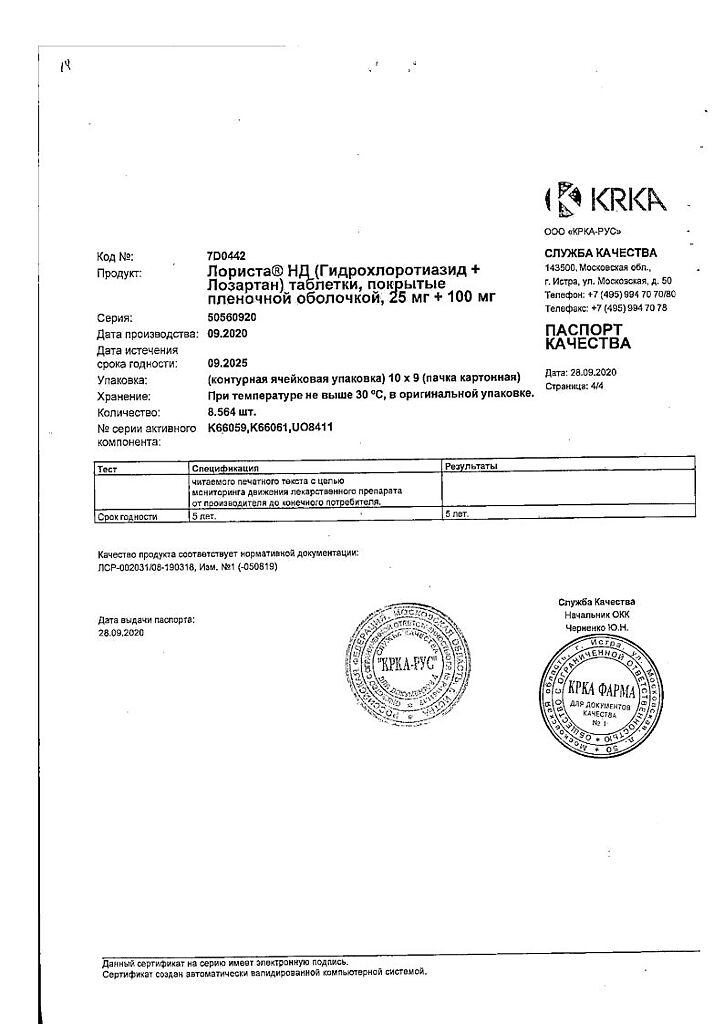
Lorista ND, 100 mg+25 mg 90 pcs
€32.25 €26.87
Description
Pharmacotherapeutic group: hypotensive combined agent (angiotensin II receptor antagonist [ARA II] + diuretic)
ATX code: C09DA01
Pharmacological properties
Mechanism of action
The drug Lorista® ND
The components of the drug Lorista® ND have an additive antihypertensive effect, reducing blood pressure (BP) to a greater extent than each of the components separately. It is believed that this effect is due to the complementary action of both components. Due to its diuretic effect, hydrochlorothiazide increases plasma renin activity (PRA), stimulates aldosterone secretion, increases angiotensin II concentration and decreases serum potassium. Administration of losartan blocks all physiologic effects of angiotensin II and, due to the suppression of aldosterone effects, may contribute to the reduction of potassium loss associated with diuretic intake.
Lozartan has moderate and transient uricosuric effects. Hydrochlorothiazide causes a slight increase in plasma uric acid concentration. The combination of losartan and hydrochlorothiazide reduces the severity of diuretic-induced hyperuricemia.
Lozartan
Angiotensin II is a potent vasoconstrictor, the main active hormone of the renin-angiotensin-aldosterone system (RAAS), and a crucial pathophysiological link in the development of arterial hypertension (AH). Angiotensin II binds to AT1 receptors located in many tissues (vascular smooth muscle tissues, adrenal glands, kidneys and heart) and performs several important biological functions, including vasoconstriction and aldosterone release. In addition, angiotensin II stimulates smooth muscle cell overgrowth. AT2 receptors are the second type of receptors to which angiotensin II binds, but its role in the regulation of cardiovascular function is unknown.
Lozartan is a selective angiotensin II AT]-receptor antagonist that is highly effective when taken orally. Losartan and its pharmacologically active carboxylated metabolite (E-3174) both in vitro and in vivo block all physiological effects of angiotensin II regardless of its source or synthesis pathway. Unlike some peptide angiotensin II antagonists, losartan has no agonist properties.
Lozartan selectively binds to AT]-receptors and does not bind to or block receptors of other hormones and ion channels that play an important role in the regulation of cardiovascular function. In addition, losartan does not inhibit angiotensin-converting enzyme (ACE, kininase II), which is responsible for bradykinin degradation. Consequently, effects not directly related to AT1 receptor blockade, such as increased bradykinin-mediated effects or the development of edema (losartan 1.7%, placebo 1.9%), are not relevant to the action of losartan.
Hydrochlorothiazide
The mechanism of antihypertensive action of thiazides is unknown. Thiazides usually have no effect on normal BP.
Hydrochlorothiazide is a diuretic and a hypotensive agent. It affects reabsorption of electrolytes in the distal tubules of the kidneys. Hydrochlorothiazide approximately equally increases sodium and chlorine ion excretion. Natriuresis may be accompanied by a small loss of potassium ions and bicarbonate. When administered orally, the diuretic effect develops within 2 hours, reaches a maximum on average after 4 hours and lasts from 6 to 12 hours.
Pharmacodynamics
Lorist® ND is a combined drug of losartan and hydrochlorothiazide. In patients with AH and left ventricular hypertrophy, losartan, including in combination with hydrochlorothiazide, reduces the risk of cardiovascular morbidity and mortality, which has been proven by evaluating the combined incidence of stroke and myocardial infarction as well as the cardiovascular mortality rate in this patient population.
Lozartan
Lozartan suppresses increases in systolic and diastolic BP with angiotensin II infusion.
While taking losartan, the elimination of the negative feedback of angiotensin II suppression of renin secretion leads to an increase in ARP. An increase in ARP leads to an increase in plasma angiotensin II concentration. During long-term (6-week) treatment of patients with AH with losartan at a dose of 100 mg/day, a 2-3-fold increase in plasma angiotensin II concentrations was observed when the Cmax of losartan was reached. In some patients, even greater increases in angiotensin II concentrations were observed, especially with a short duration of treatment (2 weeks). Despite this, during treatment, the antihypertensive effect and decrease in plasma aldosterone concentration were evident after 2 and 6 weeks of therapy, indicating effective blockade of angiotensin II receptors. After discontinuation of losartan, ARP and angiotensin II concentrations decreased within 3 days to values observed before starting losartan.
Because losartan is a specific angiotensin II AT1-receptor antagonist, it does not inhibit ACE (kininase II), the enzyme that inactivates bradykinin. A study comparing the effects of losartan at doses of 20 mg and 100 mg with those of an ACE inhibitor for effects on angiotensin I, angiotensin II, and bradykinin showed that losartan blocks the effects of angiotensin I and angiotensin II without affecting the effects of bradykinin. This is due to the specific mechanism of action of losartan. The ACE inhibitor blocked the angiotensin I response and enhanced the bradykinin-dependent effects without affecting the angiotensin II response, demonstrating the pharmacodynamic difference between losartan and ACE inhibitors.
The plasma concentrations of losartan and its active metabolite, as well as the antihypertensive effect of losartan, increase with increasing drug dose. Because losartan and its active metabolite are ARA II, they both contribute to the antihypertensive effect.
In a study with a single dose of 100 mg of losartan that included healthy volunteers (men), oral administration of the drug on a high-salt and low-salt diet had no effect on glomerular filtration rate (GFR), effective renal plasma flow, or filtration fraction. Losartan had a natriuretic effect that was more pronounced on the low-salt diet and did not appear to be associated with suppression of early sodium reabsorption in the proximal renal tubules. Losartan also caused a transient increase in renal uric acid excretion.
In patients with AH, proteinuria (at least 2 g/24 hours), without diabetes mellitus, and taking losartan for 8 weeks at a dose of 50 mg with a gradual increase to 100 mg, there was a significant reduction in proteinuria (by 42%), fractional albumin excretion, and immunoglobulin (IgG). In these patients, losartan stabilized the FFR and decreased the filtration fraction.
In postmenopausal women with AH taking losartan at a dose of 50 mg for 4 weeks, there was no effect of therapy on renal and systemic prostaglandin levels.
Lozartan has no effect on autonomic reflexes and no lasting effect on plasma norepinephrine concentrations.
In patients with AH, losartan at doses up to 150 mg/day did not cause clinically significant changes in fasting serum triglyceride, total cholesterol, and high-density lipoprotein cholesterol concentrations. At the same doses, losartan had no effect on fasting blood glucose concentration.
In general, losartan caused a decrease in serum uric acid concentrations (generally less than 0.4 mg/dL) that persisted with long-term treatment. In controlled clinical trials with AH patients, no cases of drug withdrawal due to increased serum creatinine or potassium concentrations have been reported.
The effects of losartan at doses of 2.5 mg/day, 10 mg/day, 25 mg/day, and 50 mg/day were compared with placebo in a 12-week parallel study that included patients with left ventricular failure (NYHA functional class II-IV), most of whom were taking diuretics and/or cardiac glycosides. At doses of 25 mg/day and 50 mg/day, the drug exhibited positive hemodynamic and neurohormonal effects that persisted throughout the study. Hemodynamic effects included increases in cardiac index and decreases in pulmonary capillary congestion pressure, as well as decreases in total peripheral vascular resistance, mean systemic BP, and heart rate. The incidence of arterial hypotension in these patients depended on the drug dose. Neurohormonal effects included decreased plasma concentrations of aldosterone and norepinephrine.
Hydrochlorothiazide
Thiazide diuretic whose diuretic effect is associated with disruption of reabsorption of sodium, chloride, potassium, magnesium, water ions in the distal nephron, delays excretion of calcium and uric acid ions. It has an antihypertensive effect, the effect of which develops due to the expansion of the arterioles. It has practically no effect on normal blood pressure. Diuretic effect occurs in 1-2 hours, reaches a maximum in 4 hours and lasts 6-12 hours. The maximum antihypertensive effect occurs after 3-4 days, but it may take 3-4 weeks to achieve the optimal therapeutic effect.
Pharmacokinetics
Intake
Lozartan
When ingested, losartan is well absorbed and is metabolized by “primary passage” through the liver to form the active carboxylated metabolite and inactive metabolites. The systemic bioavailability of losartan in tablet form is approximately 33%.
Mean Cmax of losartan and its active metabolite are reached in 1 hour and 3-4 hours, respectively. No clinically significant effect on the plasma concentration profile of losartan has been identified when losartan is taken with a normal meal.
Distribution
Losartan
Losartan and its active metabolite are bound to plasma proteins (mainly albumin) by at least 99%. The volume of distribution of losartan is 34 liters. Studies in rats have shown that losartan has almost no penetration through the blood-brain barrier.
Hydrochlorothiazide
Hydrochlorothiazide penetrates the placental (but not the blood-brain barrier) and is excreted with breast milk.
Metabolism
Losartan
Approximately 14% of the dose of losartan is converted to its active metabolite by intravenous or oral administration. After intravenous or intravenous administration of radioactive carbon-labeled losartan (14C losartan), the radioactivity of circulating blood plasma is primarily due to the presence of losartan and its active metabolite. Low conversion efficiency of losartan to its active metabolite was observed in approximately 1% of patients participating in the study.
In addition to the active metabolite, biologically inactive metabolites are formed, including two major metabolites formed by hydroxylation of the side butyl chain and one minor metabolite, N-2-tetrazol-glucuronide.
Elimation
Losartan
Plasma clearance of losartan and its active metabolite is approximately 600 mL/min and 50 mL/min, respectively. Renal clearance of losartan and its active metabolite is approximately 74 mL/min and 26 mL/min, respectively. When losartan is taken orally, approximately 4% of the dose is excreted unchanged by the kidneys and approximately 6% of the dose is excreted as an active metabolite by the kidneys. Losartan and its active metabolite have linear pharmacokinetics with oral losartan doses up to 200 mg.
After oral administration, plasma concentrations of losartan and its active metabolite decrease polyexponentially with a terminal elimination half-life of approximately 2 and 6-9 hours, respectively. There is no significant plasma accumulation of either losartan or its active metabolite when the drug is dosed 100 mg once daily.
Extraction of losartan and its metabolites is by the kidneys and through the intestine with bile. After oral administration of 14C losartan in men, about 35% of radioactivity is found in urine and 58% in feces. After intravenous administration of 14C losartan in men, approximately 43% of radioactivity is detectable in urine and 50% in feces.
Hydrochlorothiazide
Hydrochlorothiazide is not metabolized and is rapidly excreted by the kidneys. When monitoring plasma concentrations of the drug for at least 24 hours, the elimination half-life ranged from 5.6 to 14.8 hours. At least 61% of the dose taken orally is excreted unchanged within 24 hours.
Pharmacokinetics in Special Patient Groups
Losartan + hydrochlorothiazide
Elderly Patients
Plasma concentrations of losartan and its active metabolite and absorption rate of hydrochlorothiazide in elderly patients with AH are not significantly different from those in younger patients with AH.
Lozartan
Gender
Values of plasma concentrations of losartan in women with AH were twice as high as in men with AH. Concentrations of the active metabolite did not differ between men and women. This apparent pharmacokinetic difference, however, has no clinical significance.
Patients with impaired liver function
When losartan was ingested by patients with mild to moderate alcoholic cirrhosis, plasma concentrations of losartan and its active metabolite were 5 and 1.7 times higher, respectively, than those of young healthy male volunteers.
Patients with impaired renal function
Plasma concentrations of losartan in patients with a creatinine clearance (CK) above 10 mL/min were not different from those in patients with unchanged renal function. The area under the concentration-time curve (AUC) of losartan in patients on hemodialysis was approximately 2-fold greater compared to the AUC of losartan in patients with normal renal function. Plasma concentrations of the active metabolite were not altered in patients with impaired renal function or patients on hemodialysis. Losartan and its active metabolite are not excreted by hemodialysis.
Indications
Indications
Arterial hypertension (patients who are indicated for combination therapy).
Risk reduction in associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy, manifested by cumulative reduction in cardiovascular mortality, stroke and myocardial infarction rates.
Active ingredient
Active ingredient
Composition
Composition
1 film-coated tablet contains:
Kernel:
Active substances:
Hydrochlorothiazide 25.00 mg
Potassium losartan 100.00 mg
Auxiliary substances:
Pregelatinized starch, microcrystalline cellulose, lactose monohydrate, magnesium stearate
Shell film:
Hypromellose, macrogol-4000, quinoline yellow dye (E104), titanium dioxide (E171), talc
.
How to take, the dosage
How to take, the dosage
The drug Lorista® ND is taken orally regardless of the time of meals, once a day. Lorista® ND can be taken simultaneously with other hypotensive agents.
Arterial hypertension
The starting and maintenance dose is 1 tablet of the drug Lorista® ND once daily. Lorista® ND is indicated if there is no adequate therapeutic effect against combination of hydrochlorothiazide 12.5 mg and losartan 50 mg once daily during 2-4 weeks. Maximal daily dose is 1 tablet of the medicine Lorist® ND once daily.
Cardiovascular risk reduction and mortality in patients with arterial hypertension and left ventricular hypertrophy
The drug Lorista® ND is used in a dose of – 1 tablet once daily. Lorista® ND is indicated for patients who do not achieve the target BP values when taking a combination of hydrochlorothiazide 12.5 mg and losartan 50 mg once daily.
Special patient groups
Patients with impaired renal function or patients on hemodialysis
Lorista® ND should not be used for initial therapy in patients with moderate renal dysfunction (CKD 30-50 ml/min). Lorista®® ND is not recommended for patients on hemodialysis. Lorista® ND should not be used in patients with severe renal dysfunction (CK less than 30 ml/min) (see section “Contraindications”).
Patients with decreased BOD
The drug Lorista® ND should not be used for initial therapy in patients with reduced OBC.
Patients with impaired liver function
The drug Lorista® ND is contraindicated in patients with severe hepatic dysfunction (see Section “Contraindications”).
Elderly patients
The drug Lorista® ND should not be used for initial therapy in elderly patients.
Interaction
Interaction
Hydrochlorothiazide
Unrecommended drug combinations
Lithium drugs
The simultaneous use of hydrochlorothiazide and lithium drugs reduces renal clearance of lithium, which may result in increased plasma lithium concentrations and increased toxicity. If it is necessary to use hydrochlorothiazide concomitantly, the dose of lithium preparations should be chosen carefully, the concentration of lithium in blood plasma should be controlled regularly, and the dose of the drug should be adjusted accordingly.
Drug combinations requiring special attention
Drugs capable of causing pirouette-type polymorphic ventricular tachycardia
Particular caution should be used with hydrochlorothiazide simultaneously with such drugs as:
-neuroleptics: phenothiazines (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine, fluphenazine), benzamides (amisulpride, sultopride, sulpride, thiapride), butyrophenones (droperidol, haloperidol), pimozide, sertindol;
– antidepressants: tricyclic antidepressants, selective serotonin reuptake inhibitors (citalopram, escitalopram);
– Antibacterials: Fluoroquinolones (levofloxacin, moxifloxacin, sparfloxacin, ciprofloxacin), macrolides (erythromycin when administered intravenously, azithromycin, clarithromycin, roxithromycin, spiramycin), co-trimoxazole;
– antifungal agents: azoles (voriconazole, itraconazole, ketoconazole, fluconazole);
– antimalarials (quinine, chloroquine, mefloquine, halofantrine, lumefantrine);
– antiprotozoal agents (pentamidine in parenteral administration);
– antianginal agents (ranolazine, bepridil);
– antineoplastic agents (vandetanib, arsenic trioxide, oxaliplatin, tacrolimus);
– antiemetics (domperidone, ondansetron);
– agents affecting gastrointestinal motility (cisapride);
– antihistamines (astemisol, terfenadine, misolastin);
– other drugs (anagrelide, vasopressin, difemanil methylsulfate, ketanserin, probucol, propofol, sevoflurane, terlipressin, terodiline, cilostazol).
Due to the increased risk of ventricular arrhythmias, especially polymorphic pirouette-type ventricular tachycardia (hypokalemia is a risk factor), plasma potassium content should be determined and, if necessary, corrected before starting hydrochlorothiazide combination therapy with the above drugs. Monitoring of the patient’s clinical condition, plasma electrolyte content and ECG parameters is necessary. In patients with hypokalemia it is necessary to use agents that do not cause polymorphic ventricular tachycardia of “pirouette” type.
Drugs that can prolong QT interval duration
The concomitant use of hydrochlorothiazide with drugs that can prolong the QT interval should be based on a careful evaluation for each patient of the ratio of expected benefit to potential risk (an increased risk of pirouette-type polymorphic ventricular tachycardia is possible). While using such combinations it is necessary to record ECG regularly (for detection of prolongation of QT interval) as well as to monitor potassium content in blood.
Drugs that can cause hypokalemia: Amphotericin B (when administered intravenously), gluco- and mineralocorticosteroids (when administered systemically), tetracosactide (ACTH), glycyrrhizic acid (carbenoxolone, drugs containing licorice root), laxatives that stimulate bowel motility
Increased risk of hypokalemia when used concomitantly with hydrochlorothiazide (additive effect). Regular monitoring of plasma potassium is necessary, and its correction, if necessary. Against the background of hydrochlorothiazide therapy it is recommended to use laxatives which do not stimulate intestinal motility.
Heart glycosides
Hypokalemia and hypomagnesemia due to thiazide diuretics increase the toxicity of cardiac glycosides. When using hydrochlorothiazide and cardiac glycosides concomitantly, plasma potassium and ECG parameters should be monitored regularly and the therapy should be adjusted if necessary.
Drug combinations requiring attention
Other hypotensive drugs
Potentiation of the antihypertensive effects of hydrochlorothiazide (additive effect). It may be necessary to adjust the dose of simultaneously prescribed hypotensive drugs.
It is recommended to stop taking hydrochlorothiazide 2-3 days before starting ACE inhibitor therapy to prevent symptomatic arterial hypotension. If this is not possible, the initial dose of ACE inhibitors should be reduced.
Ethanol, barbiturates, antipsychotics (neuroleptics), antidepressants, anxiolytics, narcotic analgesics and general anesthetic agents
The antihypertensive effect of hydrochlorothiazide may be enhanced and orthostatic hypotension potentiated (additive effect).
Nedepolarizing myorelaxants (eg, tubocurarin)
The effects of nondepolarizing myorelaxants may be enhanced.
Adrenomimetics (pressor amines)
Hydrochlorothiazide may reduce the effects of adrenomimetics such as epinephrine (adrenaline) and norepinephrine (noradrenaline).
Non-steroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors and high-dose acetylsalicylic acid (> 3 g/day)
NSAIDs may decrease the diuretic and antihypertensive effects of hydrochlorothiazide. With concomitant use, there is a risk of acute renal failure due to decreased FFR. Hydrochlorothiazide may increase the toxic effects of high doses of salicylates on the central nervous system.
Hypoglycemic oral agents and insulin
Thiazide diuretics affect glucose tolerance (hyperglycemia may develop) and decrease the effectiveness of hypoglycemic agents (hypoglycemic dose adjustment may be required).
We should use hydrochlorothiazide and metformin with caution due to the risk of lactoacidosis due to hydrochlorothiazide-induced renal dysfunction.
Beta-adrenoblockers, diazoxide
The concomitant use of thiazide diuretics (including hydrochlorothiazide) with beta-adrenoblockers or diazoxide may increase the risk of hyperglycemia.
Drugs used to treat gout (probenecid, sulfinpyrazone, allopurinol)
Dose adjustment of uricosuric medications may be necessary because hydrochlorothiazide increases serum uric acid concentrations. Thiazide diuretics may increase the incidence of hypersensitivity reactions to allopurinol.
Amantadine
Thiazide diuretics (including hydrochlorothiazide) may decrease amantadine clearance, lead to higher plasma amantadine concentrations, and increase the risk of its adverse effects.
Anticholinergic drugs (choline blockers)
Anticholinergic drugs (e.g., atropine, biperidene) increase the bioavailability of thiazide diuretics by reducing GI motility and gastric emptying rate.
Cytotoxic (antitumor) drugs
Thiazide diuretics decrease renal excretion of cytotoxic drugs (e.g., cyclophosphamide and methotrexate) and potentiate their myelosuppressive effects.
Methyldopa
Cases of hemolytic anemia have been described when hydrochlorothiazide and methyldopa are used simultaneously.
Antioepileptic drugs (carbamazepine, oxcarbazepine, topiramate)
Risk of developing symptomatic hyponatremia. In concomitant use of hydrochlorothiazide and carbamazepine it is necessary to monitor the patient’s condition and control serum sodium content. When using hydrochlorothiazide and topiramate concomitantly, the content of topiramate in blood serum should also be monitored; if necessary, potassium preparations should be administered or the dose of topiramate should be adjusted.
Selective serotonin reuptake inhibitors
When used concomitantly with thiazide diuretics, hyponatremia may be potentiated. It is necessary to control the sodium content in plasma.
Cyclosporine
The concomitant use of thiazide diuretics and cyclosporine increases the risk of hyperuricemia and gout exacerbation.
Peroral anticoagulants
Tiazide diuretics may decrease the effect of oral anticoagulants.
Iodine-containing contrast agents
Dehydration from thiazide diuretics increases the risk of acute renal failure, especially when high doses of iodine-containing contrast agents are used. Before the use of iodine-containing contrast agents it is necessary to compensate the fluid loss.
Calcium preparations
With concomitant use, an increase in calcium in the blood and the development of hypercalcemia due to decreased excretion of calcium ions by the kidneys is possible. If simultaneous use of calcium containing medicines is necessary, the plasma calcium content should be monitored and the dose of calcium preparations should be corrected.
Anion exchange resins (colestyramine and colestipol)
The anionic exchange resins reduce absorption of hydrochlorothiazide. Single doses of colestyramine and colestipol reduce absorption of hydrochlorothiazide in the GI tract by 85% and 43%, respectively.
Lozartan
No clinically significant interactions of losartan with hydrochlorothiazide, digoxin, warfarin, cimetidine, and phenobarbital have been identified in clinical studies of pharmacokinetic drug interactions. Rifampicin, being an inducer of drug metabolism, reduces the plasma concentration of the active metabolite losartan.
The use of two CYP3A4 isoenzyme inhibitors, ketoconazole and erythromycin, has been studied in clinical trials. Ketoconazole had no effect on the metabolism of losartan to the active metabolite after intravenous administration of losartan. Erythromycin had no clinically significant effect when losartan was administered orally. Fluconazole, a CYP2C9 isoenzyme inhibitor, reduces the plasma concentration of the active metabolite of losartan, but the pharmacodynamic significance of concomitant use of losartan and CYP2C9 isoenzyme inhibitors has not been studied.
Patients who do not metabolize losartan to the active metabolite have been shown to have a very rare and specific defect in the CYP2C9 isoenzyme. These data suggest that the metabolism of losartan to the active metabolite is performed by the CYP2C9 isoenzyme rather than the CYP3A4 isoenzyme.
Simultaneous use of losartan, as well as other drugs that block angiotensin II or its effects, with caliberating diuretics (e.g., spironolactone, triamterene, amiloride, eplerenone), potassium-containing supplements, or potassium salts may lead to increased serum potassium levels.
As with other drugs that affect sodium excretion, losartan may decrease lithium excretion. Therefore, when concomitant use of lithium drugs and ARA II, serum lithium concentration should be monitored carefully.
Non-steroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors, may decrease the effect of diuretics and other hypotensive agents. Due to this, the antihypertensive effect of ARA II or ACE inhibitors may be weakened when concomitantly used with NSAIDs, including selective COX-2 inhibitors.
In some patients with impaired renal function (e.g., elderly patients or patients with dehydration, including those taking diuretics) receiving NSAID therapy, including selective COX-2 inhibitors, concomitant use of ARA II or ACE inhibitors may cause further impairment of renal function, including development of acute renal failure. These effects are usually reversible, therefore concomitant use of these drugs should be performed with caution in patients with impaired renal function.
Dual RAAS blockade with ARA II, ACE inhibitors or aliskiren (renin inhibitor) is associated with an increased risk of arterial hypotension, syncope, hyperkalemia and renal function disorders (including acute renal failure) compared to monotherapy. Regular monitoring of BP, renal function and plasma electrolyte content is necessary in patients concomitantly taking Lorist® ND and other drugs that affect the RAAS.
The concomitant use of ARA II with aliskiren and drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or moderate to severe renal function impairment (FFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients. Concomitant use of ARA II with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Special Instructions
Special Instructions
Bilateral renal artery stenosis or stenosis of the artery of a single kidney, hyperkalemia, conditions after kidney transplantation (no experience of use), aortic or mitral stenosis, hypertrophic obstructive cardiomyopathy (HACMI), chronic heart failure (CHF) with associated severe renal impairment, severe heart failure (NYHA functional class IV), CHF with life-threatening arrhythmias, coronary heart disease (CHD), cerebrovascular disease, primary hyperaldosteronism, history of angioneurotic edema, arterial hypotension, liver dysfunction, renal dysfunction water-electrolyte balance disorders, patients with decreased BOD (e.g., those treated with high doses of diuretics) due to the possibility of symptomatic arterial hypotension, hypokalemia, hyponatremia, hypercalcemia, concomitant use of drugs, concomitant use of drugs that may cause polymorphic ventricular tachycardia of “pirouette” type or increase the QT interval duration on ECG, concomitant use of drugs that may cause hypokalemia, cardiac glycosides, history of penicillin allergy, hyperparathyroidism, hyperuricemia, gout, history of nonmelanoma skin cancer (NSCLC) (see sect. See section “Special Indications”).
Persons under 18 years of age are contraindicated (efficacy and safety of use have not been established)
Patients with impaired renal function or patients on hemodialysis
Lorista® ND should not be used for initial therapy in patients with moderate renal dysfunction (CKD 30-50 ml/min). Lorista®® ND is not recommended for patients on hemodialysis. Lorista® ND should not be used in patients with severe renal dysfunction (CK less than 30 ml/min) (see section “Contraindications”).
Patients with decreased BOD
The drug Lorista® ND should not be used for initial therapy in patients with reduced OBC.
Patients with impaired liver function
The drug Lorista® ND is contraindicated in patients with severe hepatic dysfunction (see Section “Contraindications”).
Elderly patients
The drug Lorista® ND should not be used for initial therapy in elderly patients.
The use of Lorista® ND in patients with acute myocardial infarction is not recommended due to insufficient experience in clinical use. Also, Lorista® ND should not be used to control hypertensive crisis.
Drug Lorista® ND
Hypersensitivity reactions
In patients with a history of angioedema (edema of the face, lips, pharynx/larynx and/or tongue) the use of the drug should be monitored (see (see section “Side effects”).
Kidney and liver function disorders
The drug Lorista® ND is contraindicated for use in patients with severe hepatic dysfunction and severe renal dysfunction (CK less than 30 mL/min) (see Section “Contraindications”).
Embryotoxicity
The use of drugs affecting the RAAS in the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and newborn morbidity and mortality. The development of oligohydramnios may be associated with fetal lung hypoplasia and skeletal deformities. Possible adverse events in neonates include skull bone hypoplasia, anuria, arterial hypotension, renal failure, and death. If pregnancy is diagnosed, Lorista® ND should be discontinued immediately (see section “Use in pregnancy and during breastfeeding”).
Hydrochlorothiazide
Kidney function disorders
In patients with renal impairment, hydrochlorothiazide may cause azotemia. In patients with renal insufficiency, hydrochlorothiazide may cumulate.
In patients with decreased renal function, periodic CK monitoring is necessary. In progression of renal function impairment and/or onset of oliguria (anuria), hydrochlorothiazide should be discontinued.
Liver function disorders
Hepatic encephalopathy may develop when using thiazide diuretics in patients with liver function disorders. In patients with severe hepatic insufficiency or hepatic encephalopathy thiazides use is contraindicated. In patients with mild to moderate hepatic insufficiency and/or progressive liver disease hydrochlorothiazide should be used with caution, since even a slight change of electrolyte-water balance and accumulation of ammonium in blood serum may cause hepatic coma. In case of encephalopathy symptoms the use of diuretics should be immediately stopped.
Water-electrolyte balance and metabolic disorders
Synopsis
Synopsis
Oval, slightly biconvex film-coated tablets from yellow to yellow with a greenish tint.
Breakage appearance: white rough mass with film coating from yellow to yellow with greenish tint.
Contraindications
Contraindications
With caution
. Bilateral renal artery stenosis or stenosis of artery of single kidney, hyperkalemia, conditions after kidney transplantation (no experience of use), aortic or mitral stenosis, hypertrophic obstructive cardiomyopathy (HOCMP), heart failure with concomitant severe renal insufficiency heart failure with life-threatening arrhythmias, coronary heart disease (CHD), cerebrovascular disease, primary hyperaldosteronism, history of angioedema, acute onset myopia and closed-angle glaucoma (on hydrochlorothiazide). Symptomatic arterial hypotension may develop in patients with reduced circulating blood volume (CBC) (e.g., those treated with high doses of diuretics).
Side effects
Side effects
No adverse reactions specific to the combination of hydrochlorothiazide + losartan were observed in clinical trials with the drugs. Adverse reactions were limited to those already reported with losartan and/or hydrochlorothiazide alone. The cumulative incidence of adverse reactions reported with this combination was comparable to that with placebo. The rate of therapy withdrawal was also comparable to that of patients taking placebo.
Overall, treatment with the combination hydrochlorothiazide + losartan was well tolerated. In most cases the adverse reactions were mild, transient, and did not require therapy withdrawal.
In controlled clinical trials in the treatment of arterial hypertension, dizziness was the only adverse reaction associated with taking the drug with an incidence greater than 1% higher than that of placebo.
As has been shown in controlled clinical trials, losartan in combination with hydrochlorothiazide is generally well tolerated in patients with arterial hypertension and left ventricular hypertrophy. The most common adverse reactions were systemic and non-systemic dizziness, weakness/increased fatigue.
The following additional adverse reactions have been reported during post-registration use of this combination, clinical trials conducted and/or post-registration use of individual active ingredients of the combination.
Blood and lymphatic system disorders:thrombocytopenia, anemia, aplastic anemia, hemolytic anemia, leukopenia, agranulocytosis.
Immune system disorders: Anaphylactic reactions, angioedema, including laryngeal and vocal fold edema with development of airway obstruction, and/or edema of the face, lips, pharynx, and/or tongue in patients taking losartan were rarely observed (â¥0.01% and < 0.1% of cases), some of these patients had a history of developing angioedema when using other medications, including ACE inhibitors.
Metabolic and nutritional disorders:anorexia, hyperglycemia, hyperuricemia, blood electrolyte imbalances, including hyponatremia and hypokalemia.
Mental disorders: insomnia, anxiety.
Nervous system disorders:dysgeusia, headache, migraine, paresthesia.
Visual organ disorders: xanthopsia, transient visual focusing disorder.
cardiac disorders:sensation of palpitations, tachycardia.
vascular disorders:dose-dependent orthostatic effects, necrotizing angiitis (vasculitis), cutaneous vasculitis.
Disorders of the respiratory system, thorax and mediastinum:cough, nasal congestion, pharyngitis, sinus disorders (sinusitis), upper respiratory tract infections, adult respiratory distress syndrome (including pneumonitis and pulmonary edema).
Digestive system disorders:dyspepsia, abdominal pain, esophageal reflux, gastrointestinal colic, diarrhea, constipation, nausea, vomiting, pancreatitis, sialadenitis.
Hepatic and biliary tract disorders:hepatitis, jaundice (intrahepatic cholestatic jaundice).
Skin and subcutaneous tissue disorders:skin rash, pruritus, purpura (including Schönlein-Genoch purpura), toxic epidermal necrolysis, urticaria, erythrodermia, photosensitization, lupus-like syndrome.
Muscular and connective tissue disorders: back pain, muscle cramps, muscle spasms, myalgia, arthralgia.
Renal and urinary tract disorders:glucosuria, impaired renal function, interstitial nephritis, renal failure.
Gender and mammary gland disorders: erectile dysfunction/impotence.
General disorders and disorders at the injection site:breast pain, edema, malaise, fever, weakness.
Laboratory and instrumental findings:disorders of liver function (rarely increased plasma alanine aminotransferase activity).
Laboratory findings
In controlled clinical trials, clinically significant changes in standard laboratory parameters have rarely been observed with the hydrochlorothiazide + losartan combination. Hyperkalemia (serum potassium > 5.5 mEq/L) was observed in 0.7% of patients, but in these studies there was no need to cancel the combination hydrochlorothiazide + losartan due to the occurrence of hyperkalemia. An increase in plasma alanine aminotransferase activity was rarely observed and usually returned to normal after discontinuation of therapy.
Overdose
Overdose
There are no data on the specific treatment of overdose with the combination of hydrochlorothiazide + losartan. Treatment is symptomatic and supportive. Lorista® ND should be discontinued and the patient should be monitored. If the drug has been taken recently, provocation of vomiting is recommended, as well as elimination of dehydration, water-electrolyte disturbances, hepatic coma and BP reduction by standard methods.
Hydrochlorothiazide
Symptoms
The most common manifestation of hydrochlorothiazide overdose is increased diuresis accompanied by acute fluid loss (dehydration) and electrolyte disturbances (hypokalemia, hyponatremia, gnpochloremia). Overdose with hydrochlorothiazide may manifest as the following symptoms:
Treatment
In overdose, symptomatic and supportive therapy is given. If the drug has been taken recently, induction of vomiting or gastric lavage are indicated for excretion of hydrochlorothiazide. Absorption of hydrochlorothiazide can be reduced by oral administration of activated charcoal.
In case of BP decrease or shock, the RBC should be compensated (by administration of plasma exchange fluids) and electrolyte deficit (potassium, sodium). In case of respiratory failure, oxygen inhalation or artificial lung ventilation is indicated. Water-electrolyte balance (especially serum potassium) and renal function should be controlled until their normalization. There is no specific antidote. Hydrochlorothiazide is excreted by hemodialysis; however, the extent of its excretion has not been determined.
Lozartan
The information about overdose is limited.
Symptoms
The most likely manifestation of overdose is a marked decrease in BP and tachycardia; bradycardia may occur due to parasympathetic (vagus) stimulation.
Treatment
Symptomatic therapy, in case of symptomatic arterial hypotension development the supporting therapy is indicated.
Losartan and its active metabolite are not excreted by hemodialysis.
Pregnancy use
Pregnancy use
Pregnancy
The use of Lorista® ND is contraindicated in pregnancy.
There is limited experience with hydrochlorothiazide during pregnancy (especially in the first trimester). Preclinical data regarding safety are insufficient. Hydrochlorothiazide penetrates the placental barrier and is detected in umbilical cord blood.
Considering the mechanism of the pharmacological action of hydrochlorothiazide, its use in the second and third trimesters of pregnancy may disrupt the feto-placental perfusion and lead to complications such as jaundice, electrolyte-water balance disorders and thrombocytopenia in fetus and newborn. Cases of thrombocytopenia have been described in newborns whose mothers received thiazide diuretics.
The use of hydrochlorothiazide during pregnancy is contraindicated. Hydrochlorothiazide should not be used for the treatment of gestosis in the second half of pregnancy (edema, arterial hypertension, or preeclampsia), as it increases the risk of decreased BOD and placental hypoperfusion, but does not have a beneficial effect on the course of these pregnancy complications. Diuretics do not prevent the development of gestosis.
Drugs acting directly on the RAAS may cause serious damage and death to the developing fetus, so Lorista® ND should be stopped immediately if pregnancy is diagnosed.
Although there is no experience with Lorista® ND in pregnant women, preclinical animal studies have shown that administration of losartan causes serious fetal and neonatal damage and fetal or offspring death. The mechanism of these phenomena is thought to be due to the effect on the RAAS.
Fetal renal perfusion dependent on the development of RAAS appears in the second trimester, so the risk to the fetus is increased if Lorista® ND is used in the second or third trimester of pregnancy.
The use of drugs affecting the RAAS in the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and mortality. The development of oligohydramnios may be associated with fetal lung hypoplasia and skeletal deformities. Possible adverse events in newborns include skull bone hypoplasia, anuria, arterial hypotension, renal failure, and death.
The above adverse outcomes are usually caused by the use of drugs affecting the RAAS in the second and third trimesters of pregnancy. Most epidemiological studies of fetal abnormalities after the use of hypotensive drugs in the first trimester of pregnancy have found no differences between RAAS-acting drugs and other hypotensive agents. When prescribing hypotensive therapy to pregnant women, it is important to optimize possible outcomes for the mother and fetus.
If alternative therapy cannot be chosen to replace therapy with drugs acting on the RAAS, the patient should be informed about the possible risk of therapy to the fetus. Periodic ultrasound examinations should be performed to assess the intra-amniotic space. If oligohydramnion is detected, Lorist® ND must be discontinued unless it is vital for the mother. Depending on the week of pregnancy, appropriate fetal tests should be performed.
Patients and physicians should be aware that oligohydramnios may not be detected until irreversible fetal damage has occurred. Newborns whose mothers have taken Lorista® ND during pregnancy should be closely monitored to control arterial hypotension, oliguria and hyperkalemia.
Breastfeeding
The use of Lorista® ND is contraindicated during breast-feeding.
Hydrochlorothiazide penetrates into breast milk, therefore its use during breastfeeding is contraindicated. If the use of hydrochlorothiazide during lactation is absolutely necessary, breastfeeding should be stopped.
It is unknown whether losartan is excreted with breast milk. Because many medications are excreted with breast milk and there is a risk of possible adverse effects in a breastfed infant, a decision should be made to discontinue breastfeeding or to discontinue Lorist® ND in light of the need for its administration to the mother.
Similarities
Similarities
Additional information
| Weight | 0.080 kg |
|---|---|
| Shelf life | 5 years. Do not use the product after the expiration date. |
| Conditions of storage | At temperature not exceeding 30ºC, in original packaging. Store out of reach of children. |
| Manufacturer | KRKA-RUS, Russia |
| Medication form | pills |
| Brand | KRKA-RUS |
Related products
Buy Lorista ND, 100 mg+25 mg 90 pcs with delivery to USA, UK, Europe and over 120 other countries.