No products in the cart.
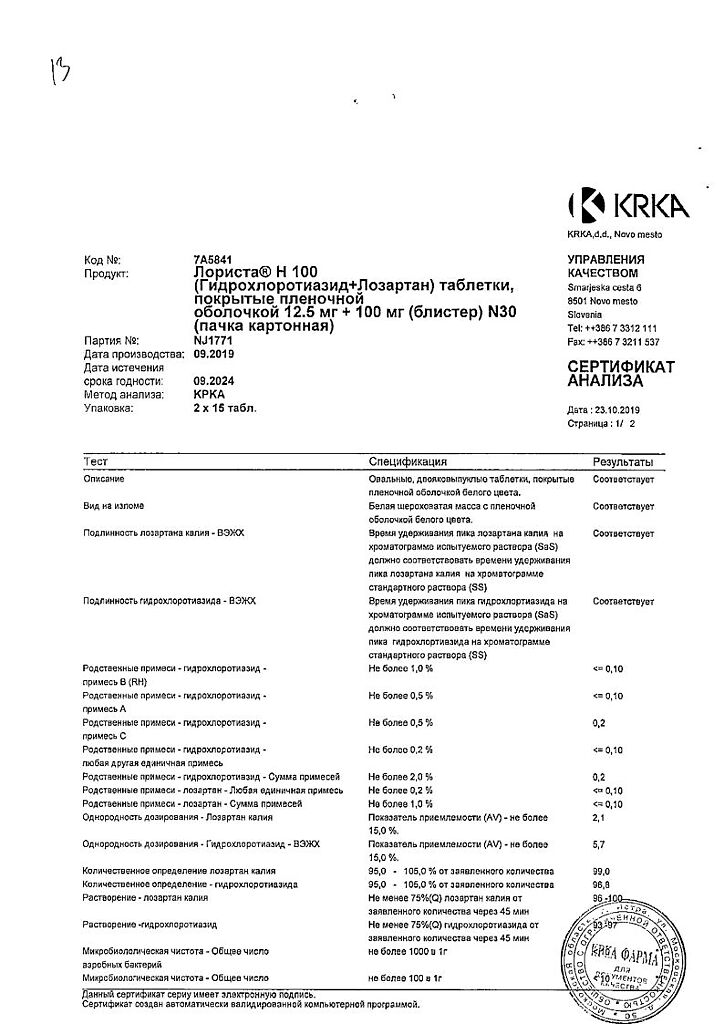
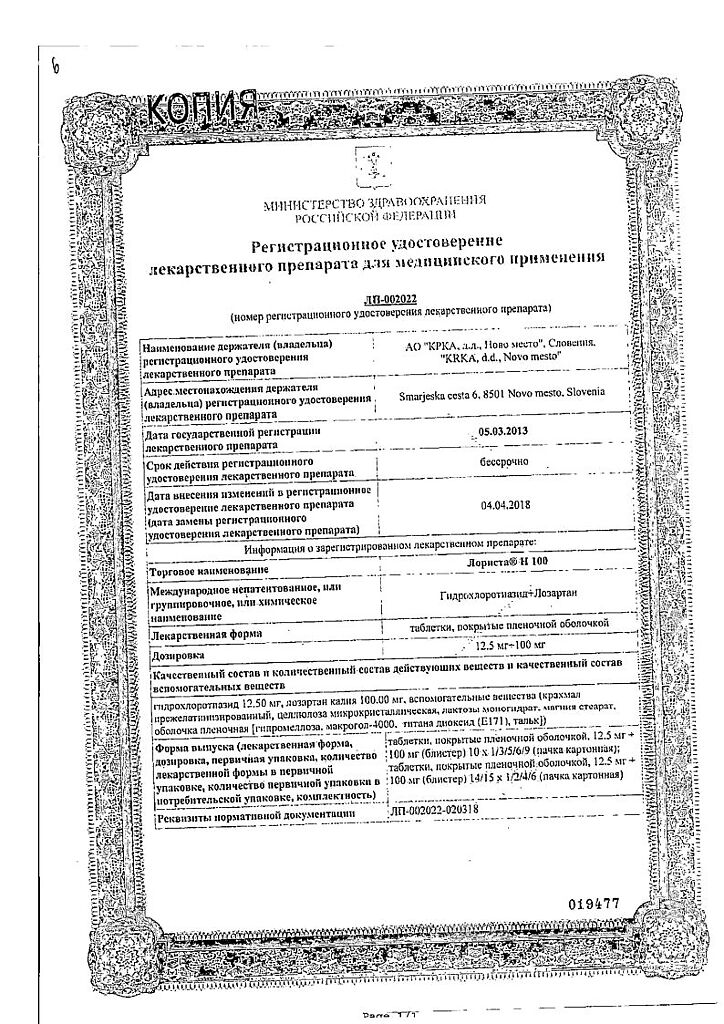
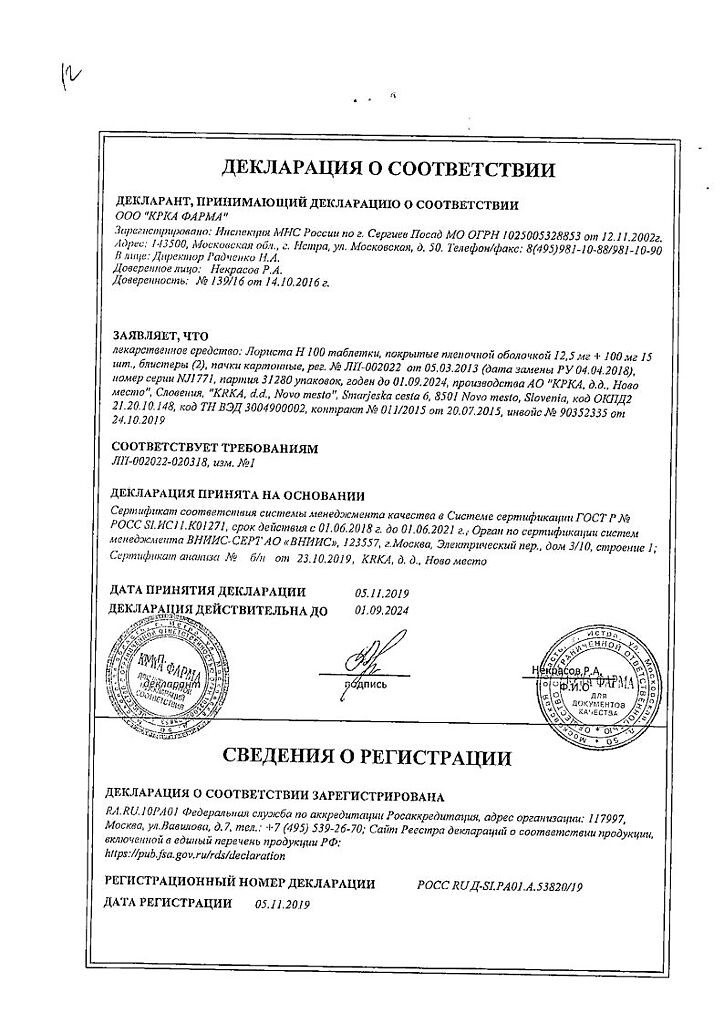
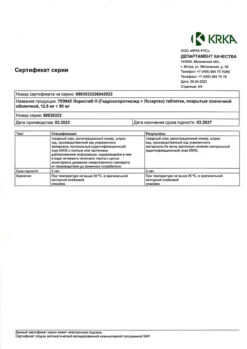
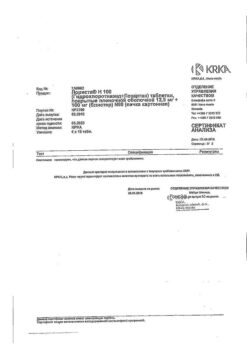
Lorista N, 100 mg+12, 5 mg 30 pcs
€14.07 €11.72
Out of stock
(E-mail when Stock is available)
Description
hypotensive combination drug (diuretic + angiotensin II receptor antagonist)
Indications
Indications
Arterial hypertension (patients for whom combination therapy is indicated).
Reduced risk of associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy, manifested by a cumulative reduction in the incidence of cardiovascular mortality, stroke and myocardial infarction.
Pharmacological effect
Pharmacological effect
antihypertensive combined drug (diuretic + angiotensin II receptor antagonist)
Special instructions
Special instructions
Bilateral renal artery stenosis or stenosis of the artery of a single kidney, hyperkalemia, conditions after kidney transplantation (no experience with use), aortic or mitral stenosis, hypertrophic obstructive cardiomyopathy (HOCM), CHF with concomitant severe renal impairment, severe CHF (IV functional class according to the NYHA classification), CHF with life-threatening arrhythmias, coronary heart disease (CHD), cerebrovascular diseases, primary hyperaldosteronism, history of angioedema, arterial hypotension, liver dysfunction, renal dysfunction, fluid and electrolyte imbalance, patients with reduced blood volume (for example, receiving treatment with large doses of diuretics) due to the possibility of symptomatic arterial hypotension, hypokalemia, hyponatremia, hypercalcemia, simultaneous use of drugs that can cause polymorphic ventricular tachycardia of the “pirouette” type or increase the duration of the QT interval on the ECG, simultaneous use of drugs that can cause hypokalemia, cardiac glycosides, a history of allergic reactions to penicillin, hyperparathyroidism, hyperuricemia, gout, a history of non-melanoma skin cancer (NMSC) (see. section “Special instructions”).
Contraindicated in persons under the age of 18 years (efficacy and safety have not been established).
Use in patients with impaired renal function and in patients on hemodialysis
There is no need to select the initial dose of the drug in patients with moderate renal impairment (creatinine clearance 30-50 ml/min). The use of the combination of hydrochlorothiazide + losartan is not recommended in patients on hemodialysis. The combination of hydrochlorothiazide + losartan should not be used in patients with severe renal failure (creatinine clearance less than 30 ml/min) (see section “Contraindications”).
Use in patients with reduced blood volume
The drug Lorista® N 100 should not be used at the initial stage of therapy in patients with reduced blood volume.
Use in patients with liver dysfunction
The use of Lorista® N 100 is contraindicated in patients with severe liver dysfunction (see section “Contraindications”).
Use in elderly patients
Lorista® N 100 should not be used at the initial stage of therapy in elderly patients.
The use of Lorista® N 100 in patients with acute myocardial infarction is not recommended due to insufficient experience in clinical use.
Also, the drug Lorista® N 100 should not be used to relieve a hypertensive crisis.
Combination hydrochlorothiazide + losartan
Children and teenagers
There is no experience with the combination of hydrochlorothiazide + losartan in children and adolescents.
If newborns whose mothers took Lorista® N 100 during pregnancy develop oliguria or arterial hypotension, symptomatic therapy aimed at maintaining blood pressure and renal perfusion is necessary. Blood transfusions or dialysis may be required to prevent hypotension and/or maintain renal function.
Elderly patients
Clinical studies have not revealed any particularities regarding the safety and effectiveness of the hydrochlorothiazide + losartan combination in elderly patients (over 65 years of age).
Hydrochlorothiazide
Renal dysfunction
In patients with impaired renal function, hydrochlorothiazide may cause azotemia. In case of renal failure, accumulation of hydrochlorothiazide is possible.
In patients with reduced renal function, periodic monitoring of CK is necessary. If renal dysfunction progresses and/or oliguria (anuria) occurs, hydrochlorothiazide should be discontinued.
Liver dysfunction
When using thiazide diuretics in patients with impaired liver function, hepatic encephalopathy may develop. In patients with severe liver failure or hepatic encephalopathy, the use of thiazides is contraindicated. In patients with mild to moderate hepatic impairment and/or progressive liver disease, hydrochlorothiazide should be used with caution, since even slight changes in fluid and electrolyte balance and accumulation of ammonium in the blood serum can cause hepatic coma. If symptoms of encephalopathy occur, diuretics should be discontinued immediately.
Water-electrolyte balance and metabolic disorders
Thiazide diuretics (including hydrochlorothiazide) can cause a decrease in blood volume (hypovolemia) and disturbances in water and electrolyte balance (including hypokalemia, hyponatremia, hypochloremic alkalosis).
Clinical symptoms of water and electrolyte imbalance are dryness of the oral mucosa, thirst, weakness, lethargy, fatigue, drowsiness, anxiety, muscle pain or cramps, muscle weakness, marked decrease in blood pressure, oliguria, tachycardia, arrhythmia and gastrointestinal disorders (such as nausea and vomiting). In patients receiving hydrochlorothiazide therapy (especially with long-term course treatment), clinical symptoms of water-electrolyte imbalance should be identified and the content of electrolytes in the blood plasma should be regularly monitored.
Sodium
All diuretics can cause hyponatremia, sometimes leading to severe complications. Hyponatremia and hypovolemia can lead to dehydration and orthostatic hypotension. A concomitant decrease in plasma chlorine content can lead to secondary compensatory metabolic alkalosis, but the frequency and severity of this effect are insignificant. It is recommended to determine the sodium content in the blood plasma before starting treatment and regularly monitor this indicator while taking hydrochlorothiazide.
Potassium
When using thiazide and thiazide-like diuretics, there is a risk of a sharp decrease in the potassium content in the blood plasma and the development of hypokalemia (potassium content in the blood plasma less than 3.4 mmol/l). Hypokalemia increases the risk of developing heart rhythm disturbances (including severe arrhythmias) and enhances the toxic effect of cardiac glycosides. In addition, hypokalemia (as well as bradycardia) is a condition that contributes to the development of polymorphic ventricular tachycardia of the “pirouette” type, which can be fatal.
Hypokalemia poses the greatest danger to the following groups of patients: elderly people, patients simultaneously receiving therapy with antiarrhythmic and non-antiarrhythmic drugs that can cause polymorphic ventricular tachycardia of the “pirouette” type or increase the duration of the QT interval on the ECG, patients with impaired liver function, coronary artery disease, and heart failure. In addition, patients with an increased QT interval are at increased risk. It does not matter whether this increase is caused by congenital causes or the effect of drugs.
In all the cases described above, it is necessary to avoid the risk of developing hypokalemia and regularly monitor the potassium content in the blood plasma. The first determination of potassium content in blood plasma should be carried out within the first week from the start of treatment. If hypokalemia occurs, appropriate treatment should be prescribed. Hypokalemia can be corrected by using potassium-containing medications or eating foods rich in potassium (dried fruits, fruits, vegetables).
Calcium
Thiazide diuretics may reduce the excretion of calcium ions by the kidneys, leading to a slight and temporary increase in plasma calcium levels. In some patients, with long-term use of thiazide diuretics, pathological changes in the parathyroid glands with hypercalcemia and hyperphosphatemia were observed, but without the typical complications of hyperparathyroidism (nephrolithiasis, decreased bone mineral density, peptic ulcer). Severe hypercalcemia may be a manifestation of previously undiagnosed hyperparathyroidism.
Because of their effect on calcium metabolism, thiazides may interfere with laboratory parameters of parathyroid function. Thiazide diuretics (including hydrochlorothiazide) should be discontinued before testing parathyroid function.
Magnesium
Thiazides have been found to increase the excretion of magnesium ions by the kidneys, which can lead to hypomagnesemia. The clinical significance of hypomagnesemia remains unclear.
Glucose
Treatment with thiazide diuretics may impair glucose tolerance. When using hydrochlorothiazide in patients with manifest or latent diabetes mellitus, it is necessary to regularly monitor the concentration of glucose in the blood. Dosage adjustment of hypoglycemic medications may be required.
Uric acid
In patients with gout, the frequency of attacks may increase or the course of gout may worsen. Careful monitoring of patients with gout and impaired uric acid metabolism (hyperuricemia) is necessary.
Lipids
When using hydrochlorothiazide, the concentration of cholesterol and triglycerides in the blood plasma may increase.
Acute myopia/secondary angle-closure glaucoma
Hydrochlorothiazide can cause an idiosyncratic reaction leading to the development of acute myopia and an acute attack of secondary angle-closure glaucoma. Symptoms include: sudden loss of vision or eye pain, usually occurring within hours to weeks of starting hydrochlorothiazide therapy. If left untreated, acute angle-closure glaucoma can lead to irreversible vision loss. If symptoms appear, you should stop taking hydrochlorothiazide as soon as possible. If intraocular pressure remains uncontrolled, emergency medical treatment or surgery may be required. Risk factors for the development of acute angle-closure glaucoma are: a history of an allergic reaction to sulfonamides or penicillin.
Immune system disorders
There are reports that thiazide diuretics (including hydrochlorothiazide) may cause exacerbation or progression of systemic lupus erythematosus, as well as lupus-like reactions.
In patients receiving thiazide diuretics, hypersensitivity reactions may occur even in the absence of a history of allergic reactions or bronchial asthma.
Photosensitivity
There is information about cases of the development of photosensitivity reactions when taking thiazide diuretics. If photosensitivity occurs while taking hydrochlorothiazide, treatment should be discontinued. If continued use of the diuretic is necessary, the skin should be protected from exposure to sunlight or artificial ultraviolet (UV) rays.
NMRK
Two pharmacoepidemiological studies using data from the Danish National Cancer Registry demonstrated an association between hydrochlorothiazide use and an increased risk of NMSC basal cell carcinoma and squamous cell carcinoma. The risk of developing NMSC increased with increasing total (cumulative) dose of hydrochlorothiazide. A possible mechanism for the development of NMSC is the photosensitizing effect of hydrochlorothiazide.
Patients taking hydrochlorothiazide as monotherapy or in combination with other drugs should be aware of the risk of developing NMSC. It is recommended that such patients undergo regular skin examination to identify any new suspicious lesions as well as changes in existing skin lesions.
Any suspicious skin changes should be reported to your doctor immediately. Suspicious areas of skin should be examined by a specialist. To clarify the diagnosis, histological examination of skin biopsies may be required.
To minimize the risk of developing NMSC, patients should be advised to follow preventive measures, such as limiting exposure to sunlight and UV rays, and using appropriate protective equipment.
In patients with a history of NMSC, it is recommended to reconsider the use of hydrochlorothiazide.
Athletes
Hydrochlorothiazide may give a positive result during doping control in athletes.
Other
In patients with severe atherosclerosis of the cerebral and coronary arteries, hydrochlorothiazide should be used with extreme caution.
Thiazide diuretics can reduce the amount of iodine bound to plasma proteins without causing signs of thyroid dysfunction.
Losartan
Angioedema
Patients with a history of angioedema (swelling of the face, lips, pharynx/larynx and/or tongue) should be under strict medical supervision when using losartan (see section “Side effects”).
Arterial hypotension and decreased blood volume
In patients with reduced blood volume and/or sodium content in the blood plasma during the use of diuretics, a diet with limited salt intake, diarrhea or vomiting, symptomatic arterial hypotension may develop, especially after taking the first dose of losartan. Correction of such conditions must be carried out before prescribing Lorista® H 100 (see sections “Indications for use” and “Contraindications”).
Water-electrolyte imbalance
Fluid and electrolyte imbalance is common in patients with renal failure with or without diabetes mellitus, so careful monitoring of these patients is necessary. Careful monitoring of potassium levels in blood plasma or CK is necessary, especially in patients with heart failure and CK 30-50 ml/min.
During treatment with the drug, it is not recommended to take potassium-sparing diuretics, potassium supplements or table salt substitutes containing potassium (see section “Interaction with other drugs”).
Liver dysfunction
Data from pharmacokinetic studies indicate that the concentration of losartan in the blood plasma in patients with cirrhosis of the liver is significantly increased, therefore, patients with a history of mild or moderate impaired liver function should prescribe Lorista® H 100 with caution. There is no experience with the use of losartan in patients with severe liver dysfunction (more than 9 points on the Child-Pugh scale), so the drug should not be used in this group of patients (see sections “Pharmacological properties. Pharmacokinetics”, “Contraindications” and “Dosage and Administration”).
Double blockade of the RAAS
There is evidence that the simultaneous use of ACE inhibitors, ARB II or aliskiren increases the risk of arterial hypotension, hyperkalemia and renal dysfunction (including acute renal failure). The simultaneous use of losartan with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients. Concomitant use of losartan with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Renal dysfunction
Due to inhibition of the RAAS, changes in renal function, including the development of renal failure, have been observed in some susceptible patients. These changes in renal function may return to normal after treatment is stopped.
Some drugs that affect the RAAS may increase serum urea and creatinine concentrations in patients with bilateral renal artery stenosis or renal artery stenosis of a solitary kidney. Similar effects have been reported with the use of losartan. Such renal dysfunction may be reversible after discontinuation of therapy. Losartan should be used with caution in patients with bilateral renal artery stenosis or renal artery stenosis of a solitary kidney.
Kidney transplant
There is no experience with patients who have recently undergone kidney transplantation.
Primary hyperaldosteronism
Since patients with primary hyperaldosteronism, as a rule, do not have a positive response to therapy with antihypertensive drugs that act by inhibiting the RAAS, the use of Lorista® H 100 is not recommended in this group of patients.
IHD and cerebrovascular diseases
Like all drugs that have a vasodilating effect, ARA II should be prescribed with caution in patients with coronary artery disease or cerebrovascular diseases, since a pronounced decrease in blood pressure in this group of patients can lead to the development of myocardial infarction or stroke.
CHF
As with other drugs that act on the RAAS, patients with CHF with or without renal impairment are at risk of developing severe hypotension and renal failure (often acute).
Aortic stenosis or mitral stenosis, HOCM
Like all drugs that have a vasodilating effect, ARA II should be used with caution in patients with aortic or mitral valve stenosis or HOCM.
Ethnic characteristics
As with ACE inhibitors, losartan and other ARBs are likely to be less effective in lowering blood pressure in blacks than in other races, possibly due to the higher prevalence of low-renin hypertension in this population.
Analysis of data from the entire population of patients included in the LIFE study to study the effect of losartan on reducing the incidence of the study’s main composite criterion in patients with hypertension and left ventricular hypertrophy (n = 9193) showed that the ability of losartan, compared with atenolol, to reduce the risk of stroke and myocardial infarction, as well as reduce the rate of cardiovascular mortality in patients with hypertension and left ventricular hypertrophy (by 13.0 %, p = 0.021) does not apply to patients of the Black race, although both treatment regimens effectively reduced blood pressure in these patients. In this study, losartan, compared with atenolol, reduced cardiovascular morbidity and mortality in patients with hypertension and left ventricular hypertrophy of all races except blacks (n = 8660, p = 0.003). However, in this study, black patients receiving atenolol had a lower risk of the study’s primary composite endpoint (i.e., lower composite incidence of cardiovascular death, stroke, and myocardial infarction) compared with race-matched patients receiving losartan (p = 0.03).
Pregnancy
ARA II should not be used during pregnancy. If there is no need for continuous therapy with ARA II, patients planning pregnancy should replace ARA II with alternative antihypertensive drugs with an established safety profile during pregnancy. If pregnancy is diagnosed, the use of Lorista® N 100 should be stopped immediately and, if necessary, alternative therapy should be started (see sections “Contraindications”, “Use during pregnancy and breastfeeding”).
Special information on excipients
The composition of the drug Lorista® N 100 includes lactose as an excipient, therefore the drug is contraindicated in patients with lactase deficiency, lactose intolerance, glucose-galactose malabsorption syndrome (see section “Contraindications”).
No studies have been conducted to assess the effect on the ability to drive vehicles and operate machines.
When driving vehicles or operating machinery, caution should be exercised due to the possibility of developing dizziness or weakness (see section “Side Effects”).
Active ingredient
Active ingredient
Hydrochlorothiazide, Losartan
Composition
Composition
1 film-coated tablet contains:
Core:
Active ingredients:
Hydrochlorothiazide 12.50 mg
Losartan potassium 100.00 mg
Excipients:
Pregelatinized starch, microcrystalline cellulose, lactose monohydrate, magnesium stearate
Film shell:
Hypromellose, macrogol-4000, titanium dioxide (E171), talc
Pregnancy
Pregnancy
Pregnancy
Hydrochlorothiazide + losartan
The use of Lorista® N 100 is contraindicated during pregnancy. Drugs that affect the renin-angiotensin-aldosterone system (RAAS) can cause serious damage and death to the fetus, therefore, if pregnancy is diagnosed, the combination of hydrochlorothiazide + losartan should be discontinued immediately.
If oligohydramnios is detected, the hydrochlorothiazide + losartan combination should be stopped unless it is vital for the mother. Depending on the stage of pregnancy, appropriate fetal tests are necessary. Patients and physicians should be aware that oligohydramnios may not be detected until irreversible fetal damage occurs. Careful monitoring of newborns whose mothers took the hydrochlorothiazide + losartan combination during pregnancy is necessary to monitor arterial hypotension, oliguria and hyperkalemia.
Hydrochlorothiazide
There is limited experience with the use of hydrochlorothiazide during pregnancy (especially in the first trimester). Preclinical data regarding safety are insufficient.
Hydrochlorothiazide penetrates the placental barrier and is detected in umbilical cord blood. Taking into account the mechanism of pharmacological action of hydrochlorothiazide, its use in the second and third trimesters of pregnancy can disrupt fetoplacental perfusion and lead to the development of complications such as jaundice, water-electrolyte imbalance and thrombocytopenia in the fetus and newborn. Cases of the development of thrombocytopenia in newborns whose mothers received thiazide diuretics have been described.
The use of hydrochlorothiazide during pregnancy is contraindicated. Hydrochlorothiazide should not be used to treat gestosis in the second half of pregnancy (edema, hypertension or preeclampsia), as it increases the risk of a decrease in blood volume and placental hypoperfusion, but does not have a beneficial effect on the course of these pregnancy complications. Diuretics do not prevent the development of gestosis.
Losartan
Although there is no experience with the use of losartan in pregnant women, preclinical studies in animals have shown that administration of losartan leads to the development of serious fetal and neonatal damage and death of the fetus or offspring. It is believed that the mechanism of these phenomena is due to the effect on the RAAS.
Renal perfusion in the fetus, depending on the development of the RAAS, appears in the second trimester, so the risk to the fetus increases if the combination of hydrochlorothiazide + losartan is used in the second and third trimester of pregnancy.
The use of drugs that affect the RAAS in the second and third trimester of pregnancy reduces fetal renal function and increases the morbidity and mortality of the fetus and newborns. The development of oligohydramnios may be associated with fetal pulmonary hypoplasia and skeletal deformation. Possible adverse events in neonates include calvarial hypoplasia, anuria, hypotension, renal failure and death.
The above undesirable outcomes are usually caused by the use of drugs that affect the RAAS in the second and third trimesters of pregnancy. Most epidemiological studies examining the development of fetal abnormalities after the use of antihypertensive drugs in the first trimester of pregnancy have not revealed differences between drugs acting on the RAAS and other antihypertensive drugs. When prescribing antihypertensive therapy to pregnant women, it is important to optimize possible outcomes for the mother and fetus.
If it is impossible to select an alternative therapy instead of therapy with drugs that affect the RAAS, it is necessary to inform the patient about the possible risk of therapy to the fetus. Periodic ultrasound examinations are necessary to assess the intra-amniotic space.
Breastfeeding period
Hydrochlorothiazide + losartan
The use of Lorista® N 100 is contraindicated during breastfeeding. Since many drugs are excreted in breast milk and there is a risk of possible adverse effects in a breastfed baby, a decision should be made to stop breastfeeding or discontinue the drug, taking into account the need for the mother.
Hydrochlorothiazide
Hydrochlorothiazide passes into breast milk, and therefore its use during breastfeeding is contraindicated. If the use of hydrochlorothiazide during lactation is absolutely necessary, then breastfeeding should be discontinued.
Losartan
It is not known whether losartan is excreted in breast milk.
Contraindications
Contraindications
Hypersensitivity to any of the components of the drug, hypersensitivity to other sulfonamide derivatives, anuria, severe renal dysfunction (creatinine clearance less than 30 ml/min), treatment-resistant hypokalemia or hypercalcemia, severe liver dysfunction, cholestasis and biliary obstruction, resistant hyponatremia, symptomatic hyperuricemia/gout, dehydration, severe arterial hypotension, difficult-to-control diabetes mellitus, Addison’s disease, concomitant use with aliskiren or drugs containing aliskiren in patients with diabetes mellitus and/or with moderate or severe renal impairment (glomerular filtration rate [GFR] less than 60 ml/min/1.73 m2 body surface area), concomitant use with angiotensin-converting enzyme (ACE) inhibitors in patients with diabetic nephropathy, pregnancy, breastfeeding period, age under 18 years (efficacy and safety have not been established), lactase deficiency, hereditary lactose intolerance, glucose-galactose malabsorption syndrome.
Interaction
Interaction
Hydrochlorothiazide
Not recommended drug combinations
Lithium preparations
With the simultaneous use of hydrochlorothiazide and lithium preparations, the renal clearance of lithium is reduced, which can lead to an increase in the concentration of lithium in the blood plasma and an increase in its toxicity. If concomitant use of hydrochlorothiazide is necessary, the dose of lithium preparations should be carefully selected, the concentration of lithium in the blood plasma should be regularly monitored and the dose of the drug should be adjusted accordingly.
Combinations of drugs requiring special attention
Drugs that can cause polymorphic ventricular tachycardia of the “pirouette” type
Hydrochlorothiazide should be used with extreme caution concomitantly with drugs such as:
· class IA antiarrhythmic drugs (quinidine, hydroquinidine, disopyramide, procainamide);
· class III antiarrhythmic drugs (dofetilide, ibutilide, bretylium tosylate), sotalol, dronedarone, amiodarone;
other (non-antiarrhythmic) medicines such as:
– neuroleptics: phenothiazines (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine, fluphenazine), benzamides (amisulpride, sultopride, sulpiride, tiapride), butyrophenones (droperidol, haloperidol), pimozide, sertindole;
– antidepressants: tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs) (citalopram, escitalopram);
– antibacterial agents: fluoroquinolones (levofloxacin, moxifloxacin, sparfloxacin, ciprofloxacin), macrolides (erythromycin for intravenous administration, azithromycin, clarithromycin, roxithromycin, spiramycin), co-trimoxazole;
– antifungals: azoles (voriconazole, itraconazole, ketoconazole, fluconazole);
– antimalarials (quinine, chloroquine, mefloquine, halofantrine, lumefantrine);
– antiprotozoal drugs (pentamidine for parenteral administration);
– antianginal drugs (ranolazine, bepridil);
– antitumor agents (vandetanib, arsenic trioxide, oxaliplatin, tacrolimus);
– antiemetics (domperidone, ondansetron);
– drugs affecting gastrointestinal motility (cisapride);
– antihistamines (astemizole, terfenadine, mizolastine);
– other medicines (anagrelide, vasopressin, difemanil methyl sulfate, ketanserin, probucol, propofol, sevoflurane, terlipressin, terodiline, cilostazol).
Due to the increased risk of ventricular arrhythmias, especially polymorphic ventricular tachycardia of the “pirouette” type (risk factor – hypokalemia), the potassium content in the blood plasma should be determined and, if necessary, adjusted before starting combination therapy with hydrochlorothiazide with the above drugs. It is necessary to monitor the patient’s clinical condition, blood plasma electrolyte levels and ECG parameters. In patients with hypokalemia, it is necessary to use drugs that do not cause polymorphic ventricular tachycardia of the “pirouette” type.
Medicines that can prolong the QT interval
The simultaneous use of hydrochlorothiazide with drugs that can prolong the QT interval should be based on a careful assessment for each patient of the expected benefit versus the potential risk (possible increased risk of developing torsade de pointes (TdP). When using such combinations, it is necessary to regularly record an ECG (to detect prolongation of the QT interval), as well as monitor potassium levels in the blood plasma.
Drugs that can cause hypokalemia: amphotericin B (when administered intravenously), gluco- and mineralocorticosteroids (when administered systemically), tetracosactide (adrenocorticotropic hormone [ACTH]), glycyrrhizic acid (carbenoxolone, preparations containing licorice root), laxatives that stimulate intestinal motility
Increased risk of hypokalemia when used simultaneously with hydrochlorothiazide (additive effect). Regular monitoring of the potassium content in the blood plasma is necessary, and, if necessary, its correction. During therapy with hydrochlorothiazide, it is recommended to use laxatives that do not stimulate intestinal motility.
Cardiac glycosides
Hypokalemia and hypomagnesemia caused by the action of thiazide diuretics increase the toxicity of cardiac glycosides. When using hydrochlorothiazide and cardiac glycosides simultaneously, you should regularly monitor the potassium content in the blood plasma, ECG readings, and, if necessary, adjust therapy.
Drug combinations requiring attention
Other antihypertensive drugs
Potentiation of the antihypertensive effect of hydrochlorothiazide (additive effect). It may be necessary to adjust the dose of concomitantly prescribed antihypertensive drugs. It is recommended to stop taking hydrochlorothiazide 2-3 days before starting ACE inhibitor therapy to prevent the development of symptomatic arterial hypotension. If this is not possible, then the initial dose of ACE inhibitors should be reduced.
Ethanol, barbiturates, antipsychotics (neuroleptics), antidepressants, anxiolytics, narcotic analgesics and general anesthesia
It is possible to enhance the antihypertensive effect of hydrochlorothiazide and potentiate orthostatic hypotension (additive effect).
Non-depolarizing muscle relaxants (eg, tubocurarine)
The effect of non-depolarizing muscle relaxants may be enhanced.
Adrenergic agonists (pressor amines)
Hydrochlorothiazide may reduce the effect of adrenergic agonists such as epinephrine (adrenaline) and norepinephrine (norepinephrine).
Nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors and high doses of acetylsalicylic acid (≥ 3 g/day)
NSAIDs may reduce the diuretic and antihypertensive effects of hydrochlorothiazide. With simultaneous use, there is a risk of developing acute renal failure due to a decrease in GFR. Hydrochlorothiazide may enhance the toxic effects of high doses of salicylates on the central nervous system.
Oral hypoglycemic agents and insulin
Thiazide diuretics affect glucose tolerance (hyperglycemia may develop) and reduce the effectiveness of hypoglycemic agents (dose adjustment of hypoglycemic agents may be required).
Hydrochlorothiazide and metformin should be used concomitantly with caution due to the risk of lactic acidosis due to renal impairment caused by hydrochlorothiazide.
Beta blockers, diazoxide
Concomitant use of thiazide diuretics (including hydrochlorothiazide) with beta-blockers or diazoxide may increase the risk of hyperglycemia.
Medicines used to treat gout (probenecid, sulfinpyrazone, allopurinol)
Dosage adjustment of uricosuric drugs may be required as hydrochlorothiazide increases serum uric acid concentrations. Thiazide diuretics may increase the incidence of hypersensitivity reactions to allopurinol.
Amantadine
Thiazide diuretics (including hydrochlorothiazide) may reduce the clearance of amantadine, lead to increased plasma concentrations of amantadine and increase the risk of adverse effects.
Anticholinergic drugs (cholinergic blockers)
Anticholinergic drugs (eg, atropine, biperiden) increase the bioavailability of thiazide diuretics by reducing gastrointestinal motility and the rate of gastric emptying.
Cytotoxic (antitumor) drugs
Thiazide diuretics reduce the renal excretion of cytotoxic drugs (for example, cyclophosphamide and methotrexate) and potentiate their myelosuppressive effects.
Methyldopa
Cases of hemolytic anemia have been described with the simultaneous use of hydrochlorothiazide and methyldopa
Antiepileptic drugs (carbamazepine, oxcarbazepine, topiramate)
Risk of developing symptomatic hyponatremia. When using hydrochlorothiazide and carbamazepine simultaneously, it is necessary to monitor the patient’s condition and monitor the sodium level in the blood serum. When using hydrochlorothiazide and topiramate simultaneously, the level of topiramate in the blood serum should also be monitored, and if necessary, prescribe potassium supplements or adjust the dose of topiramate.
SSRIs
When used simultaneously with thiazide diuretics, hyponatremia may be potentiated. Monitoring of sodium levels in blood plasma is necessary.
Cyclosporine
With simultaneous use of thiazide diuretics and cyclosporine, the risk of developing hyperuricemia and exacerbation of gout increases.
Oral anticoagulants
Thiazide diuretics may reduce the effect of oral anticoagulants.
Iodinated contrast agents
Dehydration while taking thiazide diuretics increases the risk of developing acute renal failure, especially when using high doses of iodinated contrast agents. Before using iodinated contrast agents, it is necessary to compensate for fluid loss.
Calcium preparations
With simultaneous use, it is possible to increase the calcium content in the blood plasma and develop hypercalcemia due to a decrease in the excretion of calcium ions by the kidneys. If simultaneous administration of calcium-containing drugs is necessary, the calcium level in the blood plasma should be monitored and the dose of calcium supplements should be adjusted.
Anion exchange resins (cholestyramine and colestipol)
Anion exchange resins reduce the absorption of hydrochlorothiazide. Single doses of cholestyramine and colestipol reduce the absorption of hydrochlorothiazide in the gastrointestinal tract by 85% and 43%, respectively.
Losartan
Clinical studies did not reveal clinically significant interactions between losartan and hydrochlorothiazide, digoxin, warfarin, cimetidine, phenobarbital, ketoconazole and erythromycin.
Rifampicin and fluconazole reduce the concentration of the active metabolite (this interaction has not been clinically studied).
Concomitant use with potassium-sparing diuretics (spironolactone, eplerenone, triamterene, amiloride), potassium preparations or potassium-containing salt substitutes, as well as the use of other drugs that increase the content of potassium in the blood plasma, increases the risk of developing hyperkalemia.
NSAIDs, including selective COX-2 inhibitors, may reduce the effect of diuretics and other antihypertensive agents, including losartan. The antihypertensive effect of losartan, like other antihypertensive drugs, may be reduced when using indomethacin. Concomitant use of ARB II or diuretics with NSAIDs may cause an increased risk of deterioration of renal function, including acute renal failure, and an increase in plasma potassium, especially in patients with underlying renal impairment. Combination treatment should be prescribed with caution, especially in elderly patients. Patients should be adequately hydrated and renal function monitored after initiation of combination treatment and periodically during treatment. In some patients with impaired renal function receiving treatment with NSAIDs, including selective COX-2 inhibitors, concomitant use of ARB II may worsen renal impairment. These effects are usually reversible.
Double blockade of the RAAS
Concomitant use of ARB II with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients. Concomitant use of ARB II with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
According to clinical studies, it has been proven that dual blockade of the RAAS through the simultaneous use of ACE inhibitors, ARB II or aliskiren is associated with a higher incidence of adverse events, such as arterial hypotension, hyperkalemia and decreased renal function (including acute renal failure) compared with monotherapy with a drug acting on the RAAS.
Possible reduction in the excretion of lithium ions. Therefore, when using ARA II with lithium salts simultaneously, serum lithium concentrations should be carefully monitored.
Other drugs that cause a decrease in blood pressure, such as tricyclic antidepressants, antipsychotics, baclofen, amifostine: simultaneous use of losartan with these drugs may increase the risk of developing arterial hypotension.
Overdose
Overdose
Hydrochlorothiazide + losartan
There is no data on the specific treatment of overdose with the combination of hydrochlorothiazide + losartan. Treatment is symptomatic and supportive. Taking Lorista® N 100 should be discontinued and the patient should be monitored. If the drug has been taken recently, it is recommended to induce vomiting, as well as eliminate dehydration, fluid and electrolyte disturbances, hepatic coma and lower blood pressure using standard methods.
Hydrochlorothiazide
Symptoms
The most common manifestations of an overdose of hydrochlorothiazide are an increase in diuresis, accompanied by acute loss of fluid (dehydration) and electrolyte disturbances (hypokalemia, hyponatremia, hypochloremia). An overdose of hydrochlorothiazide may be manifested by the following symptoms:
· from the cardiovascular system: tachycardia, decreased blood pressure, shock;
· from the nervous system: weakness, confusion, dizziness and spasms of the calf muscles, paresthesia, disturbances of consciousness, fatigue;
· from the gastrointestinal tract: nausea, vomiting, thirst;
· from the kidneys and urinary tract: polyuria, oliguria or anuria (due to hemoconcentration);
· laboratory indicators: hypokalemia, hyponatremia, hypochloremia, alkalosis, increased concentration of residual urea nitrogen in the blood plasma (especially in patients with renal failure).
Treatment
In case of overdose, symptomatic and supportive therapy is provided. If hydrochlorothiazide has recently been taken, induction of vomiting or gastric lavage is indicated to remove it. The absorption of hydrochlorothiazide can be reduced by oral administration of activated charcoal. In case of a decrease in blood pressure or shock, the bcc should be replenished with the introduction of plasma replacement fluids and a deficiency of electrolytes (potassium, sodium). In case of respiratory failure, oxygen inhalation or artificial ventilation is indicated. Water and electrolyte balance (especially serum potassium levels) and renal function should be monitored until they return to normal.
There is no specific antidote. Hydrochlorothiazide is eliminated by hemodialysis, but the extent of its elimination has not been established.
Losartan
Information on overdose is limited.
Symptoms
The most likely manifestation of an overdose is a pronounced decrease in blood pressure and tachycardia; bradycardia can occur due to parasympathetic (vagal) stimulation.
Treatment
Symptomatic therapy. In case of development of symptomatic arterial hypotension, maintenance therapy is indicated.
Losartan and its active metabolite are not eliminated by hemodialysis.
Clinical pharmacology
Clinical pharmacology
Pharmacodynamics
The drug Lorista® N 100 is a combination drug that contains losartan and hydrochlorothiazide, which have an additive antihypertensive effect, reducing blood pressure (BP) to a greater extent than each of the components separately.
Due to the diuretic effect, hydrochlorothiazide increases the activity of plasma renin, stimulates the secretion of aldosterone, increases the concentration of angiotensin II and reduces the potassium content in the blood plasma. Taking losartan blocks all physiological effects of angiotensin II and, by suppressing the effects of aldosterone, may help reduce diuretic-associated potassium loss.
Losartan has a moderate and transient uricosuric effect.
Hydrochlorothiazide causes a slight increase in the concentration of uric acid in the blood plasma, the combination of losartan and hydrochlorothiazide helps reduce the severity of hyperuricemia caused by the diuretic.
Hydrochlorothiazide
The mechanism of action of thiazide diuretics (thiazides) has not been fully studied. Thiazides block the reabsorption of sodium and chloride ions at the beginning of the renal tubules. Thus, they increase the excretion of sodium and chlorine and therefore the excretion of water from the body.
As a result of the diuretic effect of hydrochlorothiazide, the circulating blood volume (CBV) decreases, as a result of which the activity of renin and the content of aldosterone in the blood plasma increases. This leads to an increase in the excretion of potassium ions by the kidneys and a decrease in the potassium content in the blood plasma (hypokalemia). Hydrochlorothiazide also increases the excretion of magnesium ions and reduces the excretion of calcium ions by the kidneys. Thiazide diuretics reduce the excretion of uric acid by the kidneys and increase its concentration in the blood plasma. Thiazide diuretics also reduce carbonic anhydrase activity by increasing the excretion of bicarbonate ions. But this effect is usually weak and does not affect the pH of the urine.
At maximum therapeutic doses, the diuretic/natriuretic effect of all thiazide diuretics is approximately the same. Natriuresis and diuresis occur within 2 hours and reach their maximum after approximately 4 hours. The duration of the diuretic effect of hydrochlorothiazide ranges from 6 to 12 hours.
Hydrochlorothiazide has an antihypertensive effect. Thiazide diuretics have no effect on normal blood pressure.
Losartan
Losartan is a selective angiotensin II receptor antagonist (ARA II) (AT1 type) for oral administration. Under invivo and invitro conditions, losartan and its pharmacologically active metabolite E-3174 block all physiologically significant effects of angiotensin II on AT1 receptors, regardless of the route of its synthesis: it leads to an increase in plasma renin activity and reduces the concentration of aldosterone in the blood plasma. Losartan indirectly causes activation of AT2 receptors by increasing the concentration of angiotensin II in the blood plasma.
Does not inhibit the activity of kininase II, an enzyme that is involved in the metabolism of bradykinin. Reduces total peripheral vascular resistance (TPVR), pressure in the “lesser” circulation, reduces afterload on the myocardium, and has a diuretic effect. Prevents the development of myocardial hypertrophy, increases exercise tolerance in patients with chronic heart failure (CHF). Taking losartan once a day leads to a statistically significant decrease in systolic and diastolic blood pressure. Losartan evenly controls blood pressure throughout the day, while the antihypertensive effect corresponds to the natural circadian rhythm. The reduction in blood pressure at the end of the dosing interval was approximately 70-80% of the effect of losartan observed 5-6 hours after dosing. There is no withdrawal syndrome. Losartan does not have a clinically significant effect on heart rate (HR).
Losartan is equally effective in men and women, as well as in patients under 65 years of age and elderly patients with arterial hypertension (AH).
Pharmacokinetics
Hydrochlorothiazide + losartan
The pharmacokinetics of losartan and hydrochlorothiazide when used simultaneously does not differ from that when used in monotherapy.
Special patient groups
Elderly patients
Concentrations of losartan and its active metabolite in blood plasma and the rate of absorption of hydrochlorothiazide in elderly patients with hypertension do not differ significantly from these indicators in young patients with hypertension.
Hydrochlorothiazide
Action and distribution
Hydrochlorothiazide is not fully, but is absorbed quite quickly from the gastrointestinal tract (GIT). After oral administration at a dose of 100 mg, the maximum concentration (Cmax) of hydrochlorothiazide in the blood plasma is reached after 1.5-2.5 hours. At maximum diuretic activity (approximately 4 hours after oral administration), the concentration of hydrochlorothiazide in the blood plasma is 2 mcg/ml. The connection with blood plasma proteins is 40%.
Hydrochlorothiazide crosses the placental barrier and is excreted into breast milk, but does not cross the blood-brain barrier.
Metabolism
Hydrochlorothiazide is not metabolized in the human body.
Withdrawal
Primary route of excretion by the kidneys (filtration and secretion) unchanged. Approximately 61% of an oral dose is eliminated within 24 hours. In patients with normal renal function, the half-life (T½) ranges from 5.6 to 14.8 hours (average 6.4 hours).
Special patient groups
Impaired kidney function
In patients with moderate renal failure, T½ of hydrochlorothiazide averages 11.5 hours, and in patients with creatinine clearance (CC) less than 30 ml/min – 20.7 hours.
Losartan
Suction
Losartan is well absorbed from the gastrointestinal tract when taken orally. It undergoes significant metabolism during the “primary” passage through the liver, forming a pharmacologically active carboxylated metabolite (E-3174) and inactive metabolites. Bioavailability is approximately 33%. The average Cmax of losartan and its active metabolite is reached after 1 hour and after 3-4 hours, respectively.
Distribution
Losartan and its active metabolite bind to blood plasma proteins (mainly albumin) by more than 99%. The volume of distribution of losartan is 34 liters.
It penetrates the blood-brain barrier very poorly.
Metabolism
Losartan is metabolized to an active metabolite (E-3174) (14%) and inactive metabolites, including two major metabolites formed by hydroxylation of the butyl group of the chain, and a less significant metabolite, N-2-tetrazole glucuronide.
Withdrawal
Plasma clearance of losartan and its active metabolite is approximately 10 ml/sec (600 ml/min) and 0.83 ml/sec (50 ml/min), respectively. The renal clearance of losartan and its active metabolite is approximately 1.23 ml/sec (74 ml/min) and 0.43 ml/sec (26 ml/min). T½ of losartan and active metabolite is 2 hours and 6-9 hours, respectively. It is excreted primarily with bile through the intestines (58%), and by the kidneys – 35%. Does not cumulate.
When taken orally in doses up to 200 mg, losartan and its active metabolite have linear pharmacokinetics.
Special patient groups
Gender
The concentration of losartan in blood plasma was 2 times higher in women with hypertension compared to men with hypertension. This pharmacokinetic difference is not clinically significant. The concentration of the active metabolite does not differ between men and women.
Disorders of liver and kidney function
When losartan was taken orally by patients with mild to moderate alcoholic cirrhosis, the concentrations of losartan and its active metabolite in the blood plasma were 5 and 1.7 times higher, respectively, than in young male volunteers.
Plasma concentrations of losartan in patients with creatinine clearance above 10 ml/min did not differ from those in patients with preserved renal function. The area under the concentration-time curve (AUC) of losartan in patients on hemodialysis was approximately 2 times greater than the AUC of losartan in patients with normal renal function. Plasma concentrations of the active metabolite do not change in patients with impaired renal function or in patients on hemodialysis. Losartan and its active metabolite cannot be removed by hemodialysis.
Storage conditions
Storage conditions
At a temperature not exceeding 25°C, in original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
5 years.
Do not use the drug after the expiration date.
Manufacturer
Manufacturer
KRKA dd Novo Mesto, Slovenia
Additional information
| Shelf life | 5 years. Do not use the product after the expiration date. |
|---|---|
| Conditions of storage | At the temperature not more than 25°C, in the original package. Keep out of reach of children. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Lorista N, 100 mg+12, 5 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.