No products in the cart.
Leia, 3 mg+0.02 mg 84 pcs
€41.18 €35.69
EAN: 3582910090793
SKU: 270253
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
Contraception
– contraception;
– contraception and treatment of moderate acne (acne vulgaris);
– contraception and treatment of severe premenstrual syndrome (PMS).
Active ingredient
Active ingredient
Composition
Composition
Permaceutical tablets, film-coated pink, round, biconvex. 1 tablet
drospirenone 3 mg
ethinyl estradiol 0.02 mg
Excipients:
lactose monohydrate – 68.18 mg,
Polacryline potassium – 4 mg,
povidone K30 – 4 mg,
magnesium stearate – 0.8 mg.
Shell composition:
opadray II pink 85F34048 – 2 mg (macrogol 3350 – 0.404 mg, titanium dioxide – 0.496 mg, polyvinyl alcohol – 0.8 mg, talc – 0.296 mg, iron oxide red dye – 0.0036 mg, iron oxide yellow dye – 0.0004 mg).
Placebo tablets are white, round, biconvex.
Excipients:
Lactose monohydrate – 73.4 mg,
Polacryline potassium – 1.6 mg,
povidone K-30 – 4 mg,
silicon dioxide colloid – 0.2 mg,
magnesium stearate – 0.8 mg.
Shell composition:
opadray II white 85F18422 – 2 mg (macrogol-3350 – 0.8 mg, titanium dioxide – 0.5 mg, polyvinyl alcohol – 0.404 mg, talc – 0.296 mg).
How to take, the dosage
How to take, the dosage
The drug Leia is intended to be taken orally daily for 28 days without interruptions, approximately at the same time, with a little water, in the order indicated on the blister pack. Taking pills from a new package begins the day after taking the last tablet from the previous package.
How to take Lea
The administration of Leia begins on the first day of the menstrual cycle (i.e. the first day of menstrual bleeding). It is allowed to start taking it on days 2-5 of menstrual cycle, but in this case it is recommended to use an additional barrier method of contraception during the first 7 days of taking the pills from a new package.
The “withdrawal” bleeding usually begins on the 2nd or 3rd day after starting the inactive pills and may not end before taking the pills from the new pack.
If you switch from other combined oral contraceptives (OCs, vaginal ring, or transdermal patch).
Preferably, Leia should be started the day after taking the last active pill from the previous package, but never later than the day after the usual 7-day interval (for products containing 21 active pills) or after taking the last inactive pill (for products containing 28 pills per package). Leia should be started on the day the vaginal ring or contraceptive patch is removed, but no later than the day a new ring or patch is to be inserted.
When switching from contraceptives containing only gestagens (“mini-pills,” injectable forms, implant or intrauterine contraceptive).
A woman may switch from a “mini-pili” to Leia on any day (without a break), from an implant or intrauterine therapeutic system releasing gestagen – on the day of its removal, from an injectable contraceptive – on the day when the next injection is to be made. In all cases, it is necessary to use an additional barrier method of contraception during the first 7 days of taking the pills.
After an abortion in the first trimester of pregnancy
A woman may begin taking Leia from the first day after the abortion. If this condition is met, the woman does not need additional contraceptive measures.
After childbirth or 2nd trimester abortion
It is recommended that Leia be started 21-28 days after childbirth, in the absence of breastfeeding, or 2nd trimester abortion. If it is begun later, it is necessary to use an additional barrier method of contraception during the first 7 days of taking the pills. However, if the woman has already been sexually active, pregnancy must be ruled out before starting Leia.
Missing pills
Missing inactive pills can be ignored. However, they should be discarded to avoid inadvertently prolonging the period of inactive pills. The following recommendations apply only to skipping active pills:
If it is less than 24 hours late in taking the medication, contraceptive protection is not reduced. The woman should take the missed pill as soon as possible and take the next ones at the usual time.
If pills are missed for more than 24 hours, contraceptive protection may be reduced. The more pills missed, and the closer the missed pills are to the inactive pill phase, the greater the chance of pregnancy.
The following basic rules can guide you:
– taking the drug should never be interrupted, for more than 7 days (the recommended interval for inactive pills is 4 days);
– 7 days of continuous pills are required to achieve adequate suppression of the hypothalamic-pituitary-ovarian system.
Hence, if the delay in taking active pills is more than 24 h, the following can be recommended:
From day 1 to day 7:
The woman should take the last missed pill as soon as she remembers it, even if it means taking two pills at once. She continues to take the next pills at the usual time. In addition, an additional barrier method of contraception (e.g., a condom) should be used for the next 7 days. If sexual intercourse took place in the 7 days before skipping the pill, the possibility of pregnancy should be considered.
From day 8 to day 14:
The woman should take the last pill she missed as soon as she remembers it, even if that means taking two pills at once. The next pills should be taken at the usual time. Provided that the woman has taken the pills correctly in the 7 days preceding the first missed pill, there is no need to use additional contraceptive measures. Otherwise, and if two or more pills are missed, additional barrier methods of contraception (e.g., a condom) should be used for 7 days.
From day 15 to day 24:
The risk of decreased reliability is inevitable because of the approaching inactive pill phase. A woman should strictly adhere to one of the following two options. That said, if all pills were taken correctly in the 7 days preceding the first missed pill, there is no need to use additional contraceptive methods. Otherwise, she needs to use the first of the following regimens and additionally use a barrier method of contraception (such as a condom) for 7 days.
1 option:
The woman should take the last missed pill as soon as she remembers (even if that means taking two pills at once). The next pills are taken at the usual time until the active pills in the package run out. The four inactive pills should be discarded and the pills from the next pack should be started immediately. Bleeding “cancellation” is unlikely until the active pills in the second pack are finished, but “smeary” discharge and “breakthrough” bleeding may occur while taking the pills.
Option 2:
The woman can also stop taking the pills from her current pack. She should then take a break of no more than 4 days, including the days she missed the pills, and then start taking the pills from the new package. If the woman skipped the active pills and no bleeding “cancellation” occurred while taking the inactive pills, pregnancy must be ruled out.
Recommendations in gastrointestinal disorders
In severe gastrointestinal disorders, absorption of the drug may not be complete, so additional contraceptive measures should be taken.
If vomiting occurs within 4 hours of taking the active pill, the recommendations for skipping the pill should be followed. If a woman does not want to change her usual regimen and postpone the start of her menstruation to another day of the week, an additional active pill should be taken from a different package.
Changing the day menstrual bleeding starts
In order to delay the onset of menstrual bleeding, women should continue taking pills from the next package, skipping the inactive pills from the current package. In this way, the cycle can be prolonged, if desired, for any length of time, until the active pills of the second package run out. While taking pills from the second package, a woman may experience “smeary” discharge or “breakthrough” uterine bleeding. Regular use of Leia is resumed after the end of the inactive pill phase.
In order to move the start day of menstrual bleeding to another day of the week, a woman should shorten the next phase of inactive pills by the desired number of days. The shorter the interval, the greater the risk that she will not have “cancellation” bleeding and will have “spotting” and “breakthrough” bleeding during the second pack (just like when she would like to delay the start of her menstrual-like bleeding) in the future.
How to delay bleeding “cancellation”
To delay the onset of menstruation, a woman must switch to taking pills from a new pack of Leia, skipping the placebo pills. This extension of the cycle can continue until the active pills of the second pack run out. During this extension, a woman may experience a “breakthrough” bleeding or bloody discharge. Thereafter, regular use of Leia should be resumed after the usual 7-day interval without taking the pills.
In order to postpone the onset of menstruation to another day more suitable to a woman’s usual schedule, it is possible to shorten the second phase of taking the placebo pills for as many days as necessary. The shorter this phase, the greater the risk of not developing “cancellation” bleeding, and of having “breakthrough” bleeding or bleeding while taking the second-pack of pills (and of delaying menstruation).
Special patient groups
.Children and adolescents
The Leia drug is indicated only after the onset of menarche. The available data do not suggest a dose adjustment in this group of patients.
Elderly patients
Not applicable. Leia is not indicated after the onset of menopause.
Patients with liver disorders
Leja is contraindicated in women with severe liver disease until liver function returns to normal. (See Contraindications and Pharmacological Action).
Patients with renal impairment
Leah is contraindicated in women with severe renal impairment or acute renal failure. (see sections “Contraindications” and “Pharmacological effects”).
Interaction
Interaction
The interaction of oral contraceptives with other medications may result in “breakthrough” bleeding and/or decreased contraceptive reliability. Women taking these drugs should temporarily use barrier methods of contraception in addition to taking Leia or choose another method of contraception.
The use of drugs that induce microsomal liver enzymes may lead to increased clearance of sex hormones. These drugs include: phenytoin, barbiturates, primidone, carbamazepine, rifampicin; there are also suggestions for oxcarbazepine, topiramate, felbamate, griseofulvin, and drugs containing St. John’s wort.
HIV proteases (e.g., ritonavir) and non-nucleoside reverse transcriptase inhibitors (e.g., nevirapine) and combinations thereof can also potentially affect hepatic metabolism.
Some antibiotics (e.g., penicillins and tetracyclines) can decrease intestinal hepatic estrogen recirculation, thereby lowering ethinylestradiol concentrations, according to individual studies.
When taking drugs that affect microsomal enzymes and for 28 days after their withdrawal, an additional barrier method of contraception should be used.
When taking antibiotics (such as ampicillins and tetracyclines) and for 7 days after their withdrawal, an additional barrier method of contraception should be used. If the active (pink) pills run out during these 7 days of barrier method contraception use, you should skip taking the placebo (white) pills from the current pack and start taking pills from the next pack of Leia. The major metabolites of drospirenone are formed in plasma without the participation of cytochrome P450 system isoenzymes. Therefore, it is unlikely that cytochrome P450 isoenzyme inhibitors affect the metabolism of drospirenone. OCs can affect the metabolism of other drugs, resulting in an increase (e.g., cyclosporine) or decrease (e.g., lamotrigine) in their plasma and tissue concentrations.
Based on in vitro interaction studies as well as in vivo studies in female volunteers taking omeprazole, simvastatin and midazolam as markers, it can be concluded that the effect of drospirenone at a dose of 3 mg on the metabolism of other drugs is unlikely.
There is a theoretical possibility of increased plasma potassium concentrations in women receiving Leia concomitantly with other drugs that can increase plasma potassium concentrations. These drugs include ACE inhibitors, angiotensin II receptor antagonists, some nonsteroidal anti-inflammatory drugs, potassium-saving diuretics, and aldosterone antagonists. However, in studies evaluating the interaction of drospirenone with ACE inhibitors or indomethacin, no significant difference was found between plasma potassium concentrations compared with placebo. However, in women taking drugs that may increase plasma potassium concentrations, it is recommended that plasma potassium concentrations be determined during the first cycle of Leia.
To determine possible interactions with drugs taken concomitantly with Leia, read the instructions for use for these drugs.
Special Instructions
Special Instructions
If any of the conditions/risk factors listed below are currently present, the potential risks and expected benefits of OC use should be carefully weighed on a case-by-case basis and discussed with the patient before starting the medication. If any of these conditions or risk factors worsen, intensify, or first appear, the woman should consult her physician, who may decide whether to discontinue the medication.
Cardiovascular disease
. Epidemiologic studies suggest an association between OC use and an increased incidence of venous and arterial thrombosis and thromboembolism (such as deep vein thrombosis, pulmonary embolism, myocardial infarction, and cerebrovascular events) when taking OC. These diseases are rare.
The risk of venous thromboembolism (VTE) is highest in the first year of taking these drugs. An increased risk is present after initial use of OCs or renewed use of the same or different OCs (after a break of 4 weeks or more between doses), primarily during the first 3 months.
The overall risk of VTE in patients taking low-dose OCs (< 50 mcg ethinylestradiol) is 2-3 times higher than in nonpregnant patients not taking OCs, yet the risk remains lower compared to the risk of VTE in pregnancy and childbirth. VTE can be life-threatening or fatal (1-2% of cases). Venous thromboembolism, manifesting as deep vein thrombosis or pulmonary embolism, can occur with any OC.
In extremely rare cases, thrombosis of other blood vessels, such as hepatic, mesenteric, renal, cerebral veins and arteries, or retinal vessels, occurs with the use of OCs. Symptoms of deep vein thrombosis (DVT) include the following: unilateral swelling of the lower extremity or along a vein in the lower extremity, pain or discomfort when standing or walking only, localized fever, redness, or discoloration of the skin of the lower extremity.
The symptoms of pulmonary embolism (TELA) are: difficulty or rapid breathing; sudden cough, including some with hemoptysis; sharp pain in the chest, which may increase with deep breaths; anxiety; feeling very dizzy; and rapid or irregular heartbeat. Some of these symptoms (e.g., shortness of breath, coughing) are nonspecific and may be misinterpreted as signs of other more or less severe conditions (e.g., respiratory infection).
Arterial thromboembolism can lead to stroke, vascular occlusion, or myocardial infarction.
The symptoms of a stroke are as follows: sudden weakness or loss of sensation in the face, arm or leg,especially on one side of the body, sudden confusion, problems with speech and understanding; sudden one- or two-sided loss of vision; sudden gait disturbance, dizziness, loss of balance or coordination of movements; sudden, severe or prolonged headache for no apparent reason; loss of consciousness or fainting with or without an epileptic seizure. Other signs of vascular occlusion: sudden pain, swelling and mild bruising of the extremities, “acute abdominal” symptoms.
Symptoms of myocardial infarction include: pain, discomfort, pressure, heaviness, compression, or tumescence in the chest or behind the chest; discomfort radiating to the back, jaw, left upper extremity, epigastric region; cold sweat, nausea, vomiting or dizziness, severe weakness, anxiety or shortness of breath; palpitations that are rapid or irregular. Arterial thromboembolism can be life-threatening or fatal.
The risk of thrombosis (venous and/or arterial) and thromboembolism is increased:
– with age;
– in smokers (the risk increases with more cigarettes or greater age, especially in women over 35);
when:
– obesity (BMI greater than 30 kg/m2);
– dyslipoproteinemia;
– arterial hypertension;
– migraine;
– heart valve disease;
– atrial fibrillation;
– family history (e.g., venous or arterial thromboembolism ever in a close relative or parent at a relatively young age). If there is an inherited or acquired predisposition, the woman should be examined by an appropriate specialist to decide whether she should take OCs;
Long-term immobilization, major surgery, any surgery on the lower extremities, the pelvis, neurosurgery, or extensive trauma. In these cases, the use of OCs should be stopped (in the case of planned surgery, at least four weeks before it) and not resumed for two weeks after the end of immobilization. It is worth bearing in mind that temporary immobilization (e.g., a flight of more than 4 hours) is also a risk factor for venous thromboembolism.
The risk of thrombosis and thromboembolism is mutually reinforcing when several high-risk factors are combined.
The possible role of varicose veins and superficial thrombophlebitis in the development of venous thromboembolism remains controversial. The increased risk of thromboembolism in the postpartum period should be considered.
Peripheral circulatory disorders may also be seen in diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn’s disease or ulcerative colitis) and sickle cell anemia.
An increase in the frequency and severity of migraine during the use of OCs (which may precede cerebrovascular disorders) is grounds for immediate withdrawal of these drugs. Biochemical indicators indicating an inherited or acquired predisposition to venous or arterial thrombosis include: resistance to activated protein C, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant).
When evaluating the risk-benefit ratio, it should be considered that adequate treatment of the condition in question may reduce the associated risk of thrombosis. It should also be considered that the risk of thrombosis and thromboembolism in pregnancy is higher than with low-dose oral contraceptives (< 0.05 mg ethinylestradiol).
There is some evidence that preparations containing drospirenone have a higher risk of thromboembolic complications compared with those containing levonorgestrel, norgestimate, or norethindrone.
Tumors
The most significant risk factor for cervical cancer, is persistent papillomavirus infection. There have been reports of some increased risk of cervical cancer with long-term use of OCs. The association with OC use has not been proven. There remains controversy about the extent to which these findings are related to screening for cervical abnormalities or to patterns of sexual behavior (less frequent use of barrier methods of contraception).
A meta-analysis of 54 epidemiological studies showed that there is a slightly increased relative risk of breast cancer diagnosed in women currently taking OC (relative risk 1.24). The increased risk gradually disappears over a period of 10 years after stopping these drugs. Because breast cancer is rare in women younger than 40 years of age, the increase in breast cancer diagnoses in women currently or recently taking OC is small relative to the overall risk of the disease. The increased risk observed may be due to earlier diagnosis of breast cancer in women using OCs, to the biological effects of the oral contraceptives, or to a combination of both. Women who have used OCs are at an earlier stage of breast cancer than women who have never used them. Rarely has there been evidence of benign, and very rarely, malignant liver tumors developed during the use of OCs, sometimes leading to life threatening intra-abdominal bleeding. This should be considered when making a differential diagnosis if severe abdominal pain, liver enlargement, or signs of intra-abdominal bleeding occur. Tumors can be life-threatening or fatal.
Other conditions
Clinical studies have shown no effect of drospirenone on plasma potassium concentrations in patients with mild to moderate renal impairment. There is a theoretical risk of hyperkalemia in patients with impaired renal function with an initial potassium concentration at the upper limit of normal when simultaneously taking drugs that lead to potassium retention in the body. However, in women who are at increased risk of developing hyperkalemia, it is recommended that plasma potassium concentrations be determined during the first cycle of Leia.
Women with hypertriglyceridemia (or a family history of this condition) may have an increased risk of pancreatitis while taking OC.
While small increases in BP have been described in many women taking OCs, clinically significant increases have been rare. However, if a persistent, clinically significant increase in BP develops while taking OCs, the medications should be stopped and treatment for arterial hypertension should be initiated. The use of OCs may be continued if normal BP is achieved with hypotensive therapy.
The following conditions have been reported to develop or worsen both during pregnancy and while taking OCs, but their association with taking OCs has not been proven: Jaundice and/or pruritus associated with cholestasis; gallstone formation; porphyria; systemic lupus erythematosus; hemolytic uremic syndrome; Sydenham’s chorea; pregnancy herpes; hearing loss associated with otosclerosis. Cases of Crohn’s disease and ulcerative colitis have also been described with OCs.
In women with hereditary forms of angioedema, exogenous estrogens may cause or worsen symptoms of angioedema.
Acute or chronic liver dysfunction may require withdrawal of OCs until liver function returns to normal. A recurrence of cholestatic jaundice first developed during a previous pregnancy or previous use of sex hormones requires discontinuation of OCs. Although OCs may affect insulin resistance and glucose tolerance, hypoglycemic dose adjustments are not usually necessary in diabetic patients using low-dose OCs (< 0.05 mg ethinylestradiol). However, diabetic women should be closely monitored by an endocrinologist while taking OCs. Occasionally, chloasma may develop, especially in women with a history of pregnancy chloasma. Women with a history of chloasma should avoid prolonged sun exposure and exposure to ultraviolet radiation while taking OCs.
Cases of depression and epilepsy have been described while taking OCs.
Laboratory tests
The use of OC can affect the results of some laboratory tests, including indicators of liver, kidney, thyroid and adrenal function, plasma levels of transport proteins, carbohydrate metabolism, coagulation parameters and fibrinolysis. The changes usually do not go beyond the normal values. Drospirenone increases plasma renin and aldosterone activity, which is associated with its anti-mineralocorticoid effect.
Medical examinations
. Before starting or resuming use of Leia, a woman’s medical history, family history, thorough medical (including measurement of BP, heart rate, and BMI) and gynecologic examinations (including breast examination and cervical mucus cytology), and pregnancy should be ruled out. The frequency and nature of follow-up examinations should be determined individually for each woman, but at least once every 6 months.
Warn women that OCs do not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Decreased efficacy
The efficacy of Leia may be reduced in the following cases: skipping active pills (pink), vomiting, diarrhea, or as a result of drug interactions.
Inadequate control of the menstrual cycle
An irregular bleeding (“smeary” bleeding or “breakthrough” bleeding) may occur while taking Leia, especially during the first months of use. Therefore, any irregular bleeding should be evaluated only after an adjustment period of approximately three cycles.
If irregular bleeding recurs or develops after previous regular cycles, a thorough evaluation should be performed to rule out malignancy or pregnancy. Some women may not develop “withdrawal” bleeding during a break in the active pill (pink). If Leia was taken as directed, it is unlikely that the woman is pregnant. If Leia was taken irregularly or if there are no two consecutive “withdrawal” bleeds, pregnancy must be ruled out to continue taking the drug.
Influence on the ability to drive and operate vehicles
There is no known effect of Leia on the ability to operate vehicles and machinery.
Contraindications
Contraindications
The use of Leia is contraindicated in the presence of any of the conditions listed below; if any of these conditions occur for the first time during treatment with OCs, the use should be stopped immediately.
– Thrombosis (venous and arterial) and thromboembolism, current or history of thrombosis (including deep vein thrombosis). deep vein thrombosis, pulmonary embolism, myocardial infarction), cerebrovascular disorders (including history). transient ischemic attacks, angina pectoris) currently or in the history;
– Hereditary or acquired predisposition to develop venous or arterial thrombosis, such as activated protein C resistance, antithrombin III deficiency, protein C deficiency, protein S deficiency, hyperhomocysteinemia, and antiphospholipid antibodies (cardiolipin antibodies, lupus anticoagulant);
– migraine with focal neurologic symptoms currently or in the history;
– multiple or significant risk factors for venous or arterial thrombosis, includingÑ. complicated valvular heart disease, atrial fibrillation; cerebrovascular or coronary artery disease; uncontrolled arterial hypertension; severe dyslipoproteinemia; diabetes with vascular complications; major surgery with prolonged immobilization; Smoking over 35 years of age; obesity with BMI greater than 30 kg/m2; extensive trauma;
– Liver failure, severe liver disease (until normalization of liver function parameters);
– Liver tumors (benign or malignant), includingÑ.
– severe renal insufficiency, acute renal failure;
– adrenal insufficiency;
– pancreatitis, including a history ofhistory, if associated with severe triglyceridemia;
– identified hormone-dependent malignancies (including of genital or mammary glands) or suspected;
– vaginal bleeding of unspecified etiology;
– pregnancy or suspected pregnancy;
– period of breastfeeding;
– lactose intolerance, lactase deficiency, glucose-galactose malabsorption (lactose monohydrate is included);
– hypersensitivity to any of the components of Lea.
Cautions
If a patient has any of the conditions/risk factors listed below, the potential risks and expected benefits of OCs, including Leia, should be carefully weighed.
Risk factors for thrombosis and thromboembolism: smoking, thrombosis (including a history of anamnesis), myocardial infarction or stroke at young age in any of the closest relatives; obesity with BMI less than 30 kg/m2; dyslipoproteinemia; controlled arterial hypertension; migraine without focal neurological symptoms; heart valve disease without complications; heart rhythm disorders;
– other diseases in which peripheral circulatory disorders may be noted: diabetes mellitus; systemic lupus erythematosus; hemolytic-uremic syndrome; Crohn’s disease and ulcerative colitis; sickle cell anemia; and superficial vein phlebitis;
– hereditary angioedema;
– hypertriglyceridemia;
– liver disease;
– diseases that first appeared or worsened during pregnancy or on previous use of sex hormones (e.g., jaundice, cholestasis, cholelithiasis, otosclerosis with hearing impairment, porphyria, herpes of pregnancy, Sydenham’s chorea);
– postpartum period.
Side effects
Side effects
Data from clinical studies
The frequency of adverse reactions, presented according to the Medical Dictionary of Regulatory Affairs (MedDRA) classification: Very common (>10%), common (â¥1% < 10%), infrequent (â¥0.1% < 1%), rare (â¥0.01% < 0.1%), very rare (< 0.01%), frequency unknown (it is not possible to determine frequency from available data).
Infectious and parasitic diseases: infrequent oral candidiasis, vaginal candidiasis, herpes simplex.
Infection of the immune system: infrequent – allergic reactions, rarely – bronchial asthma; frequency unknown – hypersensitivity reactions.
Blood and lymphatic system disorders: rarely – anemia, thrombocytopenia.
Mental disorders: frequent – emotional lability; infrequent – depression, nervousness, sleep disorders; rarely – anorgasmia.
Nervous system disorders:often – headache; infrequently – paresthesia, dizziness, migraine; rarely – tremor.
Visual organ: infrequent – conjunctivitis, “dry eye” syndrome, visual disturbances.
Hearing organ and labyrinth disorders: rarely – decreased hearing.
Cardiac disorders: infrequent – extrasystoles, tachycardia.
vascular disorders: infrequent – pulmonary embolism, increased BP, decreased BP, varicose veins; rarely – arterial and venous thromboembolism, syncope.
As for the respiratory system, chest and mediastinum organs:pharyngitis.
Gastrointestinal disorders:often – nausea; infrequently – vomiting, gastroenteritis, diarrhea; rarely – constipation, abdominal pain, abdominal bloating.
With the liver and biliary tract: rarely – cholecystitis.
Skin and subcutaneous tissue disorders: infrequent – skin itching, rash, seborrhea, acne; rarely – alopecia, dry skin, eczema, photodermatitis, acneiform dermatosis, hypertrichosis, stretch marks, erythema nodosa, erythema multiforme.
Musculoskeletal and connective tissue disorders: infrequent – pain in the neck, extremities, lumbar region; muscle cramps.
Kidney and urinary tract disorders: infrequently – cystitis.
From the genitals and mammary gland: frequently – pain in the mammary glands, breast engorgement, metrorrhagia, absence of menstrual-like bleeding; infrequent – breast neoplasms, galactorrhea, ovarian cysts, “hot flashes”, vaginal mucosa dryness, pelvic pain, changes in Pap smear results, decreased libido, breast enlargement, painful menstrual-like bleeding, scant menstrual-like bloody discharge; rare – cystic fibrosis, vaginitis, cervical polyps, cervical neoplasia, endometrial atrophy, heavy menstrual bleeding, dyspareunia, postcoital bleeding, abortion bleeding, increased uterine size.
Endocrine system disorders:very rarely, changes in glucose tolerance or effects on insulin resistance.
General disorders and disorders at the site of administration:often, increased body weight; infrequently, increased appetite, decreased body weight, anorexia, edema, asthenia, excessive thirst, sweating.
Laboratory and instrumental data: infrequent – hyperkalemia, hyponatremia.
Data on postmarketing use
The following serious adverse reactions with unknown frequency in women taking OCs have been reported: venous thromboembolic complications, arterial thromboembolic complications, increased blood pressure, and liver neoplasms.
The association with OC use is not conclusive with the occurrence or worsening of the following conditions: Crohn’s disease, ulcerative colitis, epilepsy, uterine myoma, porphyria, systemic lupus erythematosus, herpes of pregnancy, Sydenham’s chorea, hemolytic-uremic syndrome, cholestatic jaundice, chloasma.
Acute and chronic liver dysfunction may require withdrawal of OC until markers of hepatic function return to normal.
In women with hereditary angioedema, exogenous estrogens may cause a manifestation or exacerbation of the disease.
The incidence of breast cancer among women taking OCs is slightly increased, although a causal association with OC use has not been established.
Overdose
Overdose
To date, there have been no cases of Leia overdose.
In view of clinical experience with OCs, the following symptoms may occur in case of overdose: nausea, vomiting, “smeary” bloody discharge or metrorrhagia.
There is no antidote and treatment is symptomatic.
Similarities
Similarities
Additional information
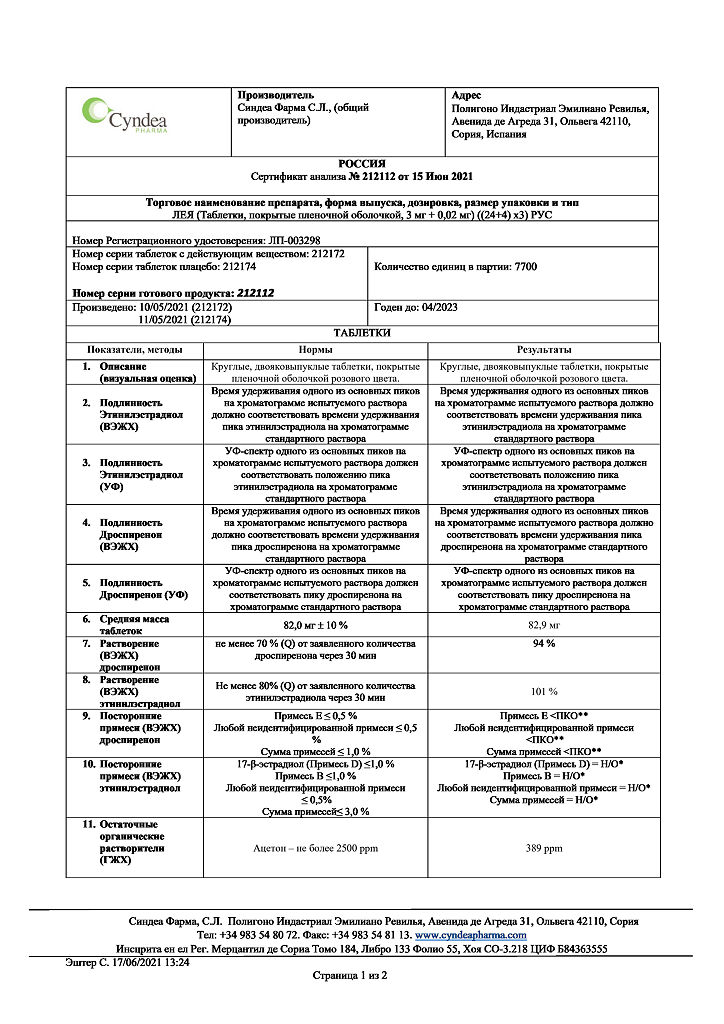
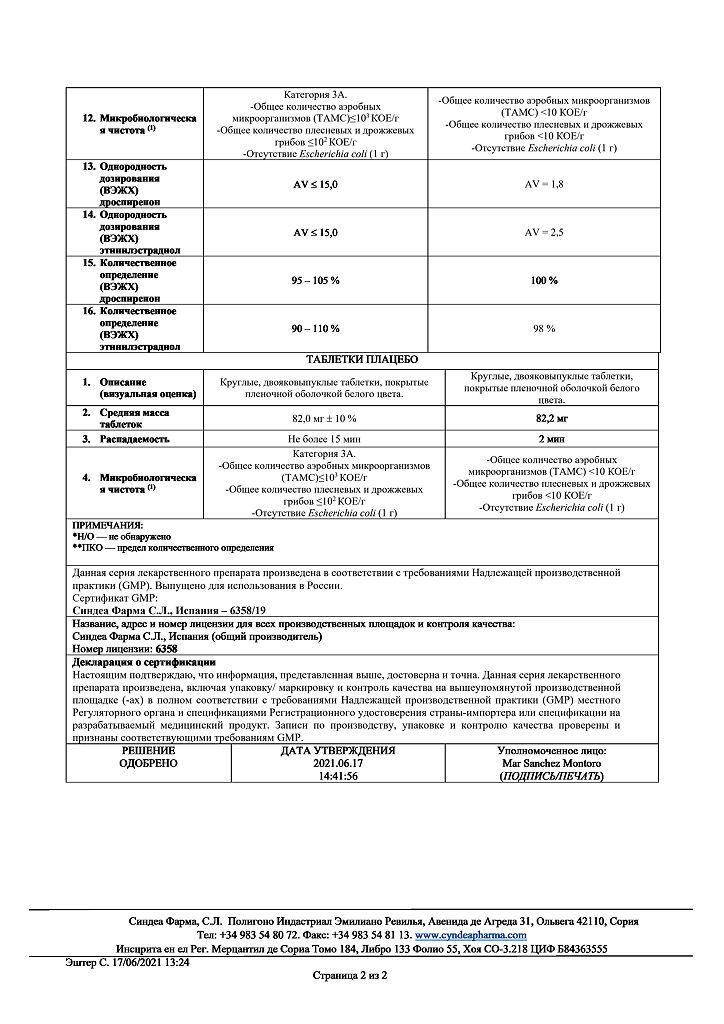
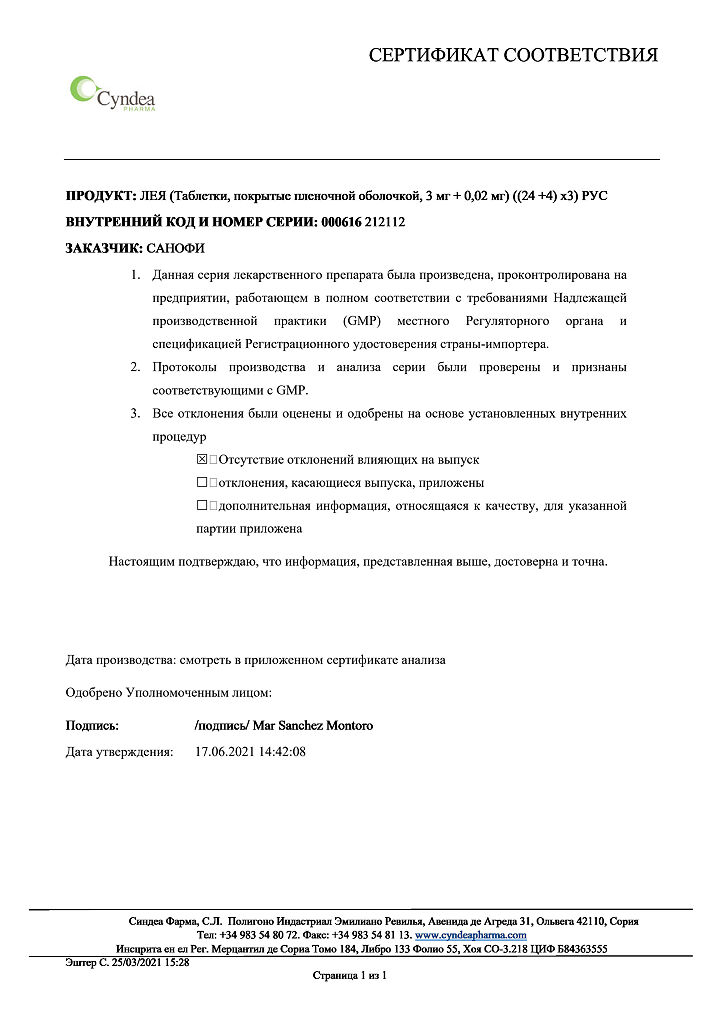
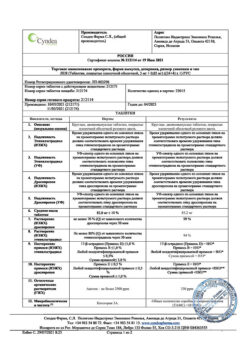
| Manufacturer | Sindea Pharma S.L., Spain |
|---|---|
| Medication form | pills |
| Brand | Sindea Pharma S.L. |
Other forms…
Related products
Gynecology and Obstetrics
Prepidil, intracervical gel 0.5 mg/3 g syringes with catheter
Gynecology and Obstetrics
Gynecology and Obstetrics
Buy Leia, 3 mg+0.02 mg 84 pcs with delivery to USA, UK, Europe and over 120 other countries.