No products in the cart.
Lamotrigine Canon, tablets 25 mg 30 pcs
€17.19 €14.32
Description
Pharmacotherapeutic group:
antiepileptic agent
ATH code: N03AХ09
Pharmacological action:
Pharmacodynamics
Lamotrigine is a blocker of potential-dependent sodium channels. In neuronal culture, it causes potential-dependent blockade of continuously repetitive impulsation and suppresses the pathological release of glutamic acid (an amino acid that plays a key role in the development of epileptic seizures), as well as inhibits glutamate-induced depolarization.
Pharmacokinetics
Intake
Lamotrigine is rapidly and completely absorbed from the intestine, with little or no presystemic first-pass metabolism. The maximum plasma concentration (Cmax) is reached approximately 2.5 hours after oral administration. Time of reaching Cmax is slightly increased after meals, but the degree of absorption remains unchanged. Pharmacokinetics is linear with a single dose up to 450 mg (the highest dose studied).
Distribution
Lamotrigine binds to plasma proteins by approximately 55%. The volume of distribution (Vp) is 0.92-1.22 l/kg.
Metabolism
The enzyme uridine diphosphate glucuronyltransferase (UDF-glucuronyltransferase) is involved in lamotrigine metabolism. Lamotrigine increases its own metabolism to a small extent in a dose-dependent manner.
Elimination
In healthy adults, the clearance of lamotrigine at equilibrium concentrations averages 39 ± 14 mL/min. Lamotrigine is metabolized to glucuronides, which are excreted by the kidneys. Less than 10% of the drug is excreted unchanged by the kidneys, about 2% – by the intestine. Clearance and half-life (T½) do not depend on the dose. T½ in healthy adults averages 24 h to 35 h. In patients with Gilbert’s syndrome a 32 % decrease in drug clearance was observed compared to the control group, however, this was within the normal range for the general population. The average half-life is reduced to approximately 14 h when concomitantly administered with glucuronizing drugs such as carbamazepine and phenytoin, and increased to an average of 70 h when concomitantly administered with valproate.
In children, lamotrigine clearance per body weight is higher than in adults; it is highest in children under 5 years of age. T½ is usually shorter than in adults. It averages approximately 7 h when concomitantly administered with glucuronizing agents such as carbamazepine and phenytoin, and increases to an average of 45 to 50 h when concomitantly administered with valproate.
No clinically significant differences in lamotrigine clearance were found in elderly patients compared to younger patients.
In patients with significant impairment of renal function, a dose reduction of lamotrigine may be required.
In patients with moderate to severe hepatic impairment, doses of lamotrigine should be reduced (see section “Dosage and administration”).
Pharmacotherapeutic group: antiepileptic drug
Distribution
Lamotrigine binds to blood plasma proteins by approximately 55%. The volume of distribution (Vp) is 0.92-1.22 l/kg.
Metabolism
The enzyme uridine diphosphate glucuronyltransferase (UDF-glucuronyltransferase) is involved in lamotrigine metabolism. Lamotrigine increases its own metabolism to a small extent in a dose-dependent manner.
Elimination
In healthy adults, the clearance of lamotrigine at equilibrium concentrations averages 39 ± 14 mL/min. Lamotrigine is metabolized to glucuronides, which are excreted by the kidneys. Less than 10% of the drug is excreted unchanged by the kidneys, about 2% – by the intestine. Clearance and half-life (T½) do not depend on the dose. T½ in healthy adults averages 24 h to 35 h. In patients with Gilbert’s syndrome a 32 % decrease in drug clearance was observed compared to the control group, however, this was within the normal range for the general population. The average half-life is reduced to approximately 14 h when concomitantly administered with glucuronizing drugs such as carbamazepine and phenytoin, and increased to an average of 70 h when concomitantly administered with valproate.
In children, lamotrigine clearance per body weight is higher than in adults; it is highest in children under 5 years of age. T½ is usually shorter than in adults. It averages approximately 7 h when concomitantly administered with glucuronizing agents such as carbamazepine and phenytoin, and increases to an average of 45 to 50 h when concomitantly administered with valproate.
No clinically significant differences in lamotrigine clearance were found in elderly patients compared to younger patients.
In patients with significant impairment of renal function, a dose reduction of lamotrigine may be required.
In patients with moderate to severe hepatic impairment, doses of lamotrigine should be reduced (see section “Dosage and administration”).
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
One tablet contains:
Active substance: lamotrigine 25 mg
Associated substances:
Hyprolose (hydroxypropyl cellulose) 4.5 mg,
sodium carboxymethyl starch 3.5 mg,
p> lactose monohydrate 52 mg,
magnesium hydroxycarbonate 34 mg,
magnesium stearate 1 mg
How to take, the dosage
How to take, the dosage
Monotherapy: In adults and children over 12 years of age, an initial dose of 25 mg once daily for 2 weeks, then increasing to 50 mg once daily for 2 weeks. For optimal therapeutic effect, the dose is increased by 50-100 mg every 1 to 2 weeks. The maintenance dose is 100-200 mg/day at 1-2 doses. In some cases, a dose of 500 mg/day is required to achieve therapeutic effect.
In combination therapy with valproic acid in combination with other antiepileptic drugs or without them: the initial dose is 25 mg every other day for 2 weeks, then 25 mg once daily for 2 weeks. To achieve optimal therapeutic effect, the dose is increased by 25-50 mg every 1 to 2 weeks. Maintenance dose is 100-200 mg/day at 1-2 doses.
When antiepileptic drugs inducing “liver” enzymes (phenytoin, carbamazepine, phenobarbital and primidone), in combination with other antiepileptic drugs or without them (except valproic acid) are treated: the initial dose is 50 mg once daily for 2 weeks, then 100 mg/day in 2 doses for 2 weeks. To achieve optimal therapeutic effect, the dose is increased by a maximum of 100 mg every 1 to 2 weeks. The maintenance dose is 200-400 mg/day in 2 doses. Some patients may require a dose of 700 mg/day to achieve therapeutic effect.
In children from 2 to 12 years of age: the first 2 weeks – 2 mg/kg/day in 2 doses, then 2 weeks – 5 mg/kg/day, then increase by 2-3 mg/kg every 1-2 weeks until the effect (usually 5-15 mg/kg/day in 2 doses, maximum 400 mg/day).
In children aged 2 to 12 years, to achieve optimal therapeutic effect, the dosage regimen should be adjusted according to the changes in the child’s body weight. If the doses calculated with regard to body weight correspond to incomplete tablets, a smaller number of whole tablets should be taken.
It is likely that for children aged 2 to 6 years, a maintenance dose corresponding to the upper limit of recommended doses will be required.
The soluble/chewable tablets can be chewed, dissolved in a small amount of water (enough to cover the entire tablet), or swallowed whole with water.
Interaction
Interaction
It does not affect the plasma concentration, protein binding of concomitantly prescribed antiepileptic drugs, the concentration of ethinylestradiol and levonorgestrel after taking oral contraceptives.
Compatible with sedatives, antiepileptic drugs and anxiolytics.
The antiepileptic drugs (phenytoin, carbamazepine, phenobarbital, pyrimidone), paracetamol accelerate metabolism and shorten T1/2 of lamotrigine by 2 times.
Walproic acid inhibits liver enzymes, causes slowing of lamotrigine metabolism, resulting in a longer T1/2 to 70 h in adults and 45-55 h in children.
Myelotoxic drugs increase manifestations of hematotoxicity of the drug.
Special Instructions
Special Instructions
An objective criterion of effectiveness is the ability to reduce the frequency of spikes on EEG by 78-98%.
In individuals with bipolar disorders increases the frequency of suicidal behavior.
It weakly inhibits dihydrofolate reductase, due to which it may affect folate metabolism during long-term therapy.
If abruptly withdrawn, epilepsy manifestations may worsen, so withdrawal should be done gradually over a period of 2 weeks (except for cases requiring immediate withdrawal of the drug – if there are skin rashes).
Because early signs of skin rashes in children can be mistaken for infection, clinicians should consider the possibility of adverse reactions to the drug in children who develop rashes and fever during the first 8 weeks of therapy.
The increased risk of skin rash appears to be due to high initial doses of lamotrigine and failure to follow the recommended dose escalation schedule, with concomitant use of valproic acid, which almost doubles the T1/2 of lamotrigine.
If a skin rash occurs, the patient should be seen immediately and the drug should be stopped (unless there is evidence that the skin rash is unrelated to taking the drug).
There are reports that severe epileptic seizures, including status epilepticus, may lead to the development of rhabdomyolysis, multiple organ dysfunction, DIC, sometimes with fatal outcome. Similar conditions have been reported with lamotrigine therapy.
In children with a body weight of less than 17 kg, it is not possible to dose the drug accurately according to the above recommendations using the currently available soluble/chewable tablets of 5 mg.
There have been reports of dizziness, ataxia, diplopia, blurred vision and nausea in patients taking carbamazepine in combination with lamotrigine (these symptoms usually disappear when the dose of carbamazepine is reduced).
During treatment, caution should be exercised when driving vehicles and engaging in other potentially hazardous activities requiring increased concentration and rapid psychomotor reactions.
Contraindications
Contraindications
With caution
Disorders of the liver and kidneys.
Side effects
Side effects
The available information on adverse reactions is divided into 2 sections: adverse reactions in patients with epilepsy and adverse reactions in patients with bipolar disorder. However, when considering the safety profile of lamotrigine as a whole, information from both sections must be taken into account.
The WHO classification of the incidence of side effects:
very common â¥1/10 prescriptions (>10%);
common from â¥1/100 to < 1/10 appointments (>1% and <10%);
infrequently â¥1/1000 to <1/100 appointments (>0.1 % and < 1 %);
rarely from â¥1/10000 to < 1/1000 appointments (>0.01 % and < 0.1 %);
very rarely < 1/10000 appointments (< 0.01 %);
frequency is unknown (frequency cannot be determined from available data).
Epilepsy
Skin and subcutaneous tissue
Very common: skin rash.
Rare: Stevens-Johnson syndrome.
Very rare: toxic epidermal necrolysis.
Blood and lymphatic system
Very rare: neutropenia, leukopenia, anemia, thrombocytopenia, pancytopenia, aplastic anemia, agranulocytosis, lymphadenopathy.
Immune system disorders
Very rarely: hypersensitivity syndrome (including such symptoms as fever, lymphadenopathy, facial edema, disorders of the blood and liver function, disseminated intravascular coagulation (DIC), multiple organ failure).
Mental disorders
Often: aggressiveness, irritability.
Very rarely: tics, hallucinations, confusion.
Nervous system disorders
During monotherapy
Very common: headache; common: somnolence, insomnia, dizziness, tremor; infrequent: ataxia; rare: nystagmus.
As part of combination therapy
Very common: somnolence, ataxia, headache, dizziness; common: nystagmus, tremor, insomnia.
Rare: aseptic meningitis.
Very rarely: agitation, unsteady gait, motor disorders, worsening of Parkinson’s disease symptoms, extrapyramidal disorders, choreoathetosis, increased incidence of seizures.
Visually impaired
In monotherapy
Infrequent: diplopia, blurred vision.
As part of the combined therapy
Very common: diplopia, blurred vision; rarely: conjunctivitis.
Gastrointestinal tract
In monotherapy
Often: nausea, vomiting, diarrhea.
As part of combined therapy
Very common: nausea, vomiting.
Often: diarrhea.
Liver and biliary tract disorders
Very rare: increased “liver” enzymes activity, liver function impairment, liver failure. Liver function abnormalities usually develop in conjunction with symptoms of hypersensitivity, but in single cases observed in the absence of obvious signs of hypersensitivity.
Musculoskeletal and connective tissue
Very rare: lupus-like syndrome; frequency is unknown: osteomalacia, osteoporosis, bone fractures (especially in patients taking lamotrigine for a long time, in combination with other PEDs).
General disorders
Often: fatigue.
Bipolar affective disorder.
Skin and subcutaneous tissue
Very common: skin rash.
Rare: Stevens-Johnson syndrome.
In evaluating all studies (controlled and uncontrolled) of lamotrigine in patients with bipolar affective disorder, skin rash occurred in 12% of all patients receiving lamotrigine, whereas the incidence of skin rash in controlled studies alone was 8% in patients receiving lamotrigine and 6% in patients receiving placebo.
Nervous system
Very common: headache.
Often: agitation, drowsiness, dizziness.
Gastrointestinal system
Often: dry oral mucosa.
Musculoskeletal and connective tissue
Often: arthralgia.
General disorders
Often: pain, back pain.
Overdose:
Symptoms: single administration of doses 10-20 times the maximum therapeutic doses have been reported, including fatal cases. Overdose manifested with symptoms including nystagmus, ataxia, impaired consciousness and coma, and possible dilated QRS complex on ECG.
Treatment: hospitalization and supportive therapy according to the clinical picture or the recommendations of the national poison center are recommended.
Similarities
Similarities
Additional information
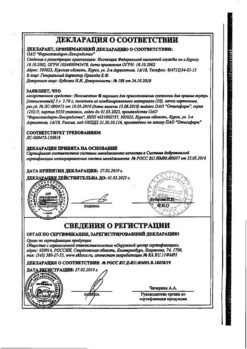
| Manufacturer | Kanonfarma Production ZAO, Russia |
|---|---|
| Medication form | pills |
| Brand | Kanonfarma Production ZAO |
Other forms…
Related products
Buy Lamotrigine Canon, tablets 25 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.