No products in the cart.
L-Tyroxine, tablets 100 mcg 50 pcs
€3.44 €3.13
Description
L-Tyroxine is a synthetic left-handed isomer of thyroxine. In its action it is identical to the naturally occurring thyroid hormone. In small doses it has an anabolic effect. In medium doses it stimulates growth and development of the body, increases the need forSynthetic left-hand-rotating isomer of thyroxine. After partial conversion to triiodothyronine (in the liver and kidneys) and transfer to body cells, it affects development and growth of tissues and metabolism. In low doses it has an anabolic effect on protein and fat metabolism. In medium doses it stimulates growth and development, increases tissue oxygen demand, stimulates metabolism of proteins, fats and carbohydrates, increases functional activity of the cardiovascular system and the central nervous system. At high doses it inhibits the production of thyrotropin-releasing hormone of the hypothalamus and thyrotropic hormone of the pituitary gland.
Therapeutic effect is observed after 7-12 days, during the same time the action lasts after discontinuation of the drug. The clinical effect in hypothyroidism is seen after 3-5 days. Diffuse goiter decreases or disappears within 3-6 months. At high doses it inhibits production of thyrotropin-releasing hormone of hypothalamus and thyrotropic hormone of pituitary.
After the start of therapy the action comes after 3-5 days.
Pharmacokinetics
In oral administration levothyroxine sodium is absorbed almost exclusively in the upper small intestine. Up to 80% of the taken dose of the drug is absorbed. Food intake reduces the absorption of levothyroxine sodium. Cmax is reached approximately 5-6 hours after oral administration. After absorption, more than 99% of the drug is bound to serum proteins (thyroxine-binding globulin, thyroxine-binding prealbumin and albumin). In various tissues, approximately 80% levothyroxine sodium is monodeiodinated to form triiodothyronine (T3) and inactive products. Thyroid hormones are metabolized primarily in the liver, kidneys, brain, and muscles. A small amount of the drug undergoes deamination and decarboxylation, as well as conjugation with sulfuric and glucuronic acids (in the liver). Metabolites are excreted by the kidneys and through the intestine. The half-life of the drug is 6-7 days. In thyrotoxicosis the half-life is shortened to 3-4 days, and in hypothyroidism it is prolonged to 9-10 days.
Indications
Indications
Hypothyroid conditions of various etiologies (including those caused by surgical or drug effects);
prevention of recurrence of nodular goiter after resection of the thyroid gland;
diffuse euthyroid goiter;
diffuse toxic goiter – after creating a euthyroid state with thyreostatics (in the form of combination or monotherapy);
thyroid cancer after surgical treatment (to suppress tumor recurrence and as replacement therapy);
as a diagnostic tool when performing a thyroid suppression test.
As part of complex therapy: Graves’ disease, autoimmune thyroiditis.
Pharmacological effect
Pharmacological effect
L-Thyroxine is a synthetic levorotatory isomer of thyroxine. Its action is identical to the naturally occurring thyroid hormone. In small doses it has an anabolic effect. In medium doses, it stimulates the growth and development of the body, increases the need for synthetic levorotatory isomer of thyroxine. After partial conversion into triiodothyronine (in the liver and kidneys) and passage into the cells of the body, it affects the development and growth of tissues and metabolism. In small doses it has an anabolic effect on protein and fat metabolism. In medium doses, it stimulates growth and development, increases the need for oxygen in tissues, stimulates the metabolism of proteins, fats and carbohydrates, and increases the functional activity of the cardiovascular system and central nervous system. In large doses, it inhibits the production of thyrotropin-releasing hormone of the hypothalamus and thyroid-stimulating hormone of the pituitary gland.
The therapeutic effect is observed after 7-12 days, during the same time the effect persists after discontinuation of the drug. The clinical effect for hypothyroidism appears after 3-5 days. Diffuse goiter decreases or disappears within 3-6 months. tissues in oxygen, stimulates the metabolism of proteins, fats and carbohydrates, the activity of the cardiovascular system and the central nervous system. In high doses, it inhibits the production of thyrotropin-releasing hormone of the hypothalamus and thyroid-stimulating hormone of the pituitary gland.
After starting therapy, the effect occurs within 3-5 days.
Pharmacokinetics
When taken orally, levothyroxine sodium is absorbed almost exclusively in the upper small intestine. Up to 80% of the dose taken is absorbed. Eating reduces the absorption of levothyroxine sodium. Cmax is reached approximately 5-6 hours after oral administration. After absorption, more than 99% of the drug binds to serum proteins (thyroxine-binding globulin, thyroxine-binding prealbumin and albumin). Approximately 80% of levothyroxine sodium is monodeiodinated in various tissues to form triiodothyronine (T3) and inactive products. Thyroid hormones are metabolized mainly in the liver, kidneys, brain and muscles. A small amount of the drug undergoes deamination and decarboxylation, as well as conjugation with sulfuric and glucuronic acids (in the liver). Metabolites are excreted by the kidneys and through the intestines. The half-life of the drug is 6-7 days. With thyrotoxicosis, the half-life is shortened to 3-4 days, and with hypothyroidism it is extended to 9-10 days.
Special instructions
Special instructions
In case of hypothyroidism caused by damage to the pituitary gland, it is necessary to find out whether there is simultaneous insufficiency of the adrenal cortex. In this case, replacement therapy with glucocorticosteroids should be started before treatment of hypothyroidism with thyroid hormones is started in order to avoid the development of acute adrenal insufficiency.
It is recommended to periodically determine the concentration of thyroid-stimulating hormone (TSH) in the blood, an increase in which indicates an insufficient dose.
The drug does not affect activities related to driving vehicles and operating machinery.
Active ingredient
Active ingredient
Levothyroxine sodium
Composition
Composition
1 tab.
levothyroxine sodium
100 mcg
Contraindications
Contraindications
Hypersensitivity;
untreated thyrotoxicosis;
acute myocardial infarction;
acute myocarditis;
untreated adrenal insufficiency (must be compensated before starting therapy).
Side Effects
Side Effects
Tachycardia;
heart rhythm disturbance;
chest pain;
tremor;
anxiety;
insomnia;
hyperhidrosis;
weight loss;
diarrhea;
alopecia;
dysfunction of the adrenal glands (with pituitary or hypothalamic hypothyroidism);
kidney function disorder in children, allergic reactions (skin rash, skin itching).
Interaction
Interaction
Levothyroxine sodium enhances the effect of indirect anticoagulants, which may require a reduction in their dose. The use of tricyclic antidepressants with levothyroxine sodium may lead to increased effects of the antidepressants. Thyroid hormones may increase the need for insulin and oral hypoglycemic agents. More frequent monitoring of blood glucose concentrations is recommended during periods of initiation of treatment with levothyroxine sodium, as well as when changing its dosage regimen. Levothyroxine sodium reduces the effect of cardiac glycosides. With simultaneous use of cholestyramine, colestipol and aluminum hydroxide, they reduce the plasma concentration of levothyroxine sodium by inhibiting its absorption in the intestine. When used simultaneously with anabolic steroids, asparaginase, tamoxifen, pharmacokinetic interaction is possible at the level of protein binding. When used simultaneously with phenytoin, salicylates, clofibrate, furosemide in high doses, the content of levothyroxine sodium and thyroxine (T4) not bound to blood plasma proteins increases. Taking estrogen-containing medications increases thyroxine-binding globulin levels, which may increase the need for levothyroxine sodium in some patients. Somatotropin, when used simultaneously with levothyroxine sodium, can accelerate the closure of epiphyseal growth zones. Taking phenobarbital, carbamazepine and rifampicin may increase the clearance of levothyroxine sodium and require an increase in dose.
The distribution and metabolism of the drug is influenced by amiodarone, aminoglutethimide, PAS, ethionamide, antithyroid drugs, beta-blockers, carbamazepine, chloral hydrate, diazepam, levodopa, dopamine, metoclopramide, lovastatin, somatostatin.
When used simultaneously with phenytoin, salicylates, furosemide (in high doses), clofibrate, the concentration of the drug in the blood increases.
Phenytoin reduces the amount of protein bound levothyroxine and T4 concentration by 15 and 25%, respectively.
Overdose
Overdose
In case of an overdose of the drug, symptoms characteristic of thyrotoxicosis are observed:
heartbeat;
heart rhythm disturbance;
heart pain;
anxiety;
tremor;
sleep disturbance;
increased sweating;
increased appetite;
weight loss;
diarrhea.
Depending on the severity of symptoms, the doctor may recommend reducing the daily dose of the drug, a break in treatment for several days, or prescribing beta-blockers. After side effects disappear, treatment should be started with caution at a lower dose.
Storage conditions
Storage conditions
The drug should be stored in a dry place, protected from light, at a temperature not exceeding 25°C. Keep out of the reach of children.
Shelf life
Shelf life
3 years.
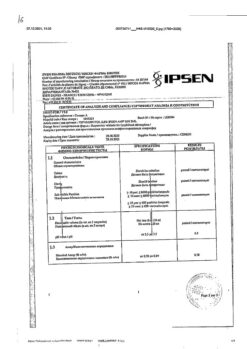
Manufacturer
Manufacturer
Ozon, Russia
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store the drug in a dry place protected from light at a temperature not exceeding 25°C. Keep out of reach of children. |
| Manufacturer | Ozon, Russia |
| Medication form | pills |
| Brand | Ozon |
Other forms…
Related products
Buy L-Tyroxine, tablets 100 mcg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.