No products in the cart.
L-Tyroxine-100 Berlin Chemi, 100 mcg tablets 100 pcs
€4.55 €4.04
Description
After partial conversion to liothyronine (in the liver and kidneys) and transfer to body cells, it influences tissue development and growth and metabolism. In small doses it has an anabolic effect on protein and fat metabolism. In medium doses it stimulates growth and development, increases tissue oxygen demand, stimulates metabolism of proteins, fats and carbohydrates, increases functional activity of the cardiovascular system and CNS. At high doses it inhibits the production of thyrotropin-releasing hormone of the hypothalamus and thyrotropic hormone of the pituitary gland.
Pharmacodynamics
Therapeutic effect is observed in 7-12 days, during the same time the effect after discontinuation of the drug is maintained. Clinical effect in hypothyroidism is seen in 3-5 days. Diffuse goiter decreases or disappears within 3-6 months.
Pharmacokinetics
When taken orally levothyroxine is absorbed almost exclusively in the upper small intestine. Up to 80% of the dose taken is absorbed. Food intake reduces the absorption of levothyroxine. Cmax in blood serum is reached 6 hours after intake.
After absorption, more than 99% of the drug is bound to serum proteins. In various tissues levothyroxine monodeidation occurs with the formation of triiodothyronine and inactive products. Thyroid hormones are metabolized mainly in the liver, kidneys, brain and muscles.
A small amount of the drug undergoes deamination and decarboxylation as well as conjugation with sulfuric and glucuronic acids (in the liver). Metabolites are excreted in the urine and bile. T1/2 is 6-8 days.
Indications
Indications
Hypothyroidism (underfunction of the thyroid gland) of any origin: primary and secondary hypothyroidism, after operations for struma, as a result of therapy with radioactive iodine (as replacement therapy).
Prevention of relapse (re-formation) of nodular goiter after surgery for goiter with normal thyroid function.
Diffuse goiter with normal function.
As part of combination therapy in the treatment of hyperfunction of the thyroid gland with thyreostatics after achieving its normal function.
Malignant tumor of the thyroid gland, mainly after surgery to suppress tumor recurrence and as replacement therapy.
Pharmacological effect
Pharmacological effect
After partial conversion into liothyronine (in the liver and kidneys) and passage into the cells of the body, it affects the development and growth of tissues and metabolism. In small doses it has an anabolic effect on protein and fat metabolism. In medium doses, it stimulates growth and development, increases tissue oxygen demand, stimulates the metabolism of proteins, fats and carbohydrates, and increases the functional activity of the cardiovascular system and central nervous system. In large doses, it inhibits the production of thyrotropin-releasing hormone of the hypothalamus and thyroid-stimulating hormone of the pituitary gland.
Pharmacodynamics
The therapeutic effect is observed after 7–12 days, during the same time the effect persists after discontinuation of the drug. The clinical effect for hypothyroidism appears after 3–5 days. Diffuse goiter decreases or disappears within 3–6 months.
Pharmacokinetics
When taken orally, levothyroxine is absorbed almost exclusively in the upper small intestine. Up to 80% of the dose taken is absorbed. Eating reduces the absorption of levothyroxine. Cmax in blood serum is achieved 6 hours after administration.
After absorption, more than 99% of the drug is bound to serum proteins. In various tissues, monodeiodination of levothyroxine occurs to form triiodothyronine and inactive products. Thyroid hormones are metabolized mainly in the liver, kidneys, brain and muscles.
A small amount of the drug undergoes deamination and decarboxylation, as well as conjugation with sulfuric and glucuronic acids (in the liver). Metabolites are excreted in urine and bile. T1/2 – 6–8 days.
Special instructions
Special instructions
In case of hypothyroidism caused by damage to the pituitary gland, it is necessary to find out whether there is simultaneous insufficiency of the adrenal cortex. In this case, replacement therapy with GCS should be started before treatment of hypothyroidism with thyroid hormones is started in order to avoid the development of acute adrenal insufficiency.
Impact on the ability to drive vehicles and operate machinery
The drug does not affect the ability to drive vehicles or work requiring increased concentration.
Active ingredient
Active ingredient
Levothyroxine sodium
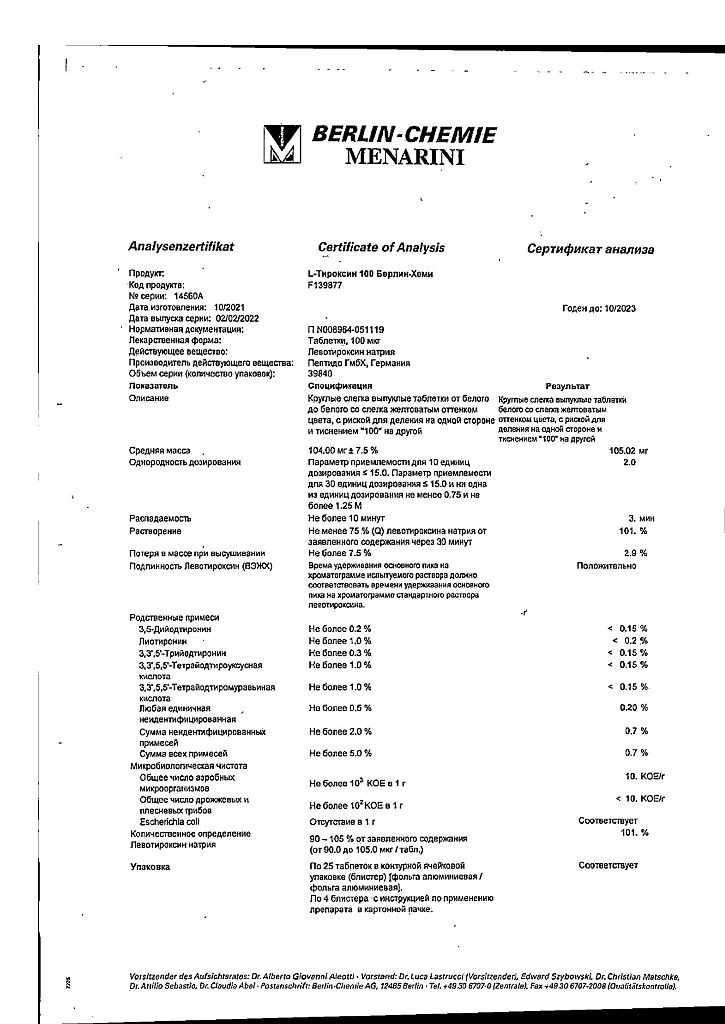
Composition
Composition
1 tablet levothyroxine sodium 100 mcg
Excipients:
calcium hydrogen phosphate dihydrate,
microcrystalline cellulose,
sodium carboxymethyl starch (type A),
dextrin,
long chain partial glycerides.
Pregnancy
Pregnancy
During pregnancy and breastfeeding, treatment should be continued. The use of the drug in combination with thyreostatics during pregnancy is contraindicated. Since thyreostatics, unlike levothyroxine, can cross the placenta, the fetus may develop hypothyroidism.
In children, the initial daily dose is 12.5-50 mcg. For a long course of treatment, the dose of the drug is determined from an approximate calculation of 100-150 mcg/m2 of body surface area.
For infants and children under 3 years of age, the daily dose of L-Thyroxine Berlin-Chemie is given in one dose 30 minutes before the first feeding. The tablet is dissolved in water to a thin suspension, which is prepared immediately before taking the drug.
Contraindications
Contraindications
Increased individual sensitivity to the drug;
acute myocardial infarction;
high blood pressure;
liver and kidney dysfunctions;
untreated adrenal insufficiency;
hyperfunction of the thyroid gland.
With caution:
– for diseases of the cardiovascular system – ischemic heart disease (atherosclerosis, angina pectoris, history of myocardial infarction), arterial hypertension, arrhythmia;
– for diabetes mellitus; severe long-term hypothyroidism; malabsorption syndrome (dose adjustment is possible).
Side Effects
Side Effects
Allergic reactions (skin rash, itchy skin).
When used in excessively high doses – hyperthyroidism (changes in appetite, dysmenorrhea, chest pain, diarrhea, tachycardia, arrhythmia, fever, tremor, headache, irritability, muscle cramps of the lower extremities, nervousness, sweating, difficulty falling asleep, vomiting, weight loss).
When used in insufficiently effective doses – hypothyroidism (dysmenorrhea, constipation, dryness, puffiness of the skin, headache, lethargy, myalgia, drowsiness, weakness, apathy, weight gain).
Interaction
Interaction
Levothyroxine enhances the effect of indirect anticoagulants, which may require a reduction in their dose.
The use of tricyclic antidepressants with levothyroxine may result in increased antidepressant effects.
Thyroid hormones may increase the need for insulin and oral hypoglycemic agents. More frequent monitoring of blood glucose levels is recommended during periods of initiation of treatment with levothyroxine, as well as when changing the dose of the drug.
Levothyroxine reduces the effect of cardiac glycosides. With simultaneous use of cholestyramine, colestipol and aluminum hydroxide, they reduce the plasma concentration of levothyroxine by inhibiting its absorption in the intestine.
When used simultaneously with anabolic steroids, asparaginase, tamoxifen, pharmacokinetic interaction is possible at the level of protein binding.
When used simultaneously with phenytoin, salicylates, clofibrate, furosemide in high doses, the content of levothyroxine and T4 unbound to blood plasma proteins increases.
Somatotropin, when used simultaneously with levothyroxine, can accelerate the closure of epiphyseal growth plates.
Taking phenobarbital, carbamazepine and rifampicin may increase the clearance of levothyroxine and require an increase in dose.
Estrogens increase the concentration of the thyroglobulin-bound fraction, which may lead to a decrease in the effectiveness of the drug.
Amiodarone, aminoglutethimide, PAS, ethionamide, antithyroid drugs, beta-blockers, carbamazepine, chloral hydrate, diazepam, levodopa, dopamine, metoclopramide, lovastatin, somatostatin affect the synthesis, secretion, distribution and metabolism of the drug.
Overdose
Overdose
Symptoms characteristic of thyrotoxicosis: palpitations, irregular heart rhythm, heart pain, anxiety, tremors, sleep disturbance, increased sweating, loss of appetite, weight loss, diarrhea.
Treatment: a reduction in the daily dose of the drug, a break in treatment for several days, and the appointment of beta-blockers may be recommended. After side effects disappear, treatment should be started with caution at a lower dose. Antithyroid drugs are not recommended.
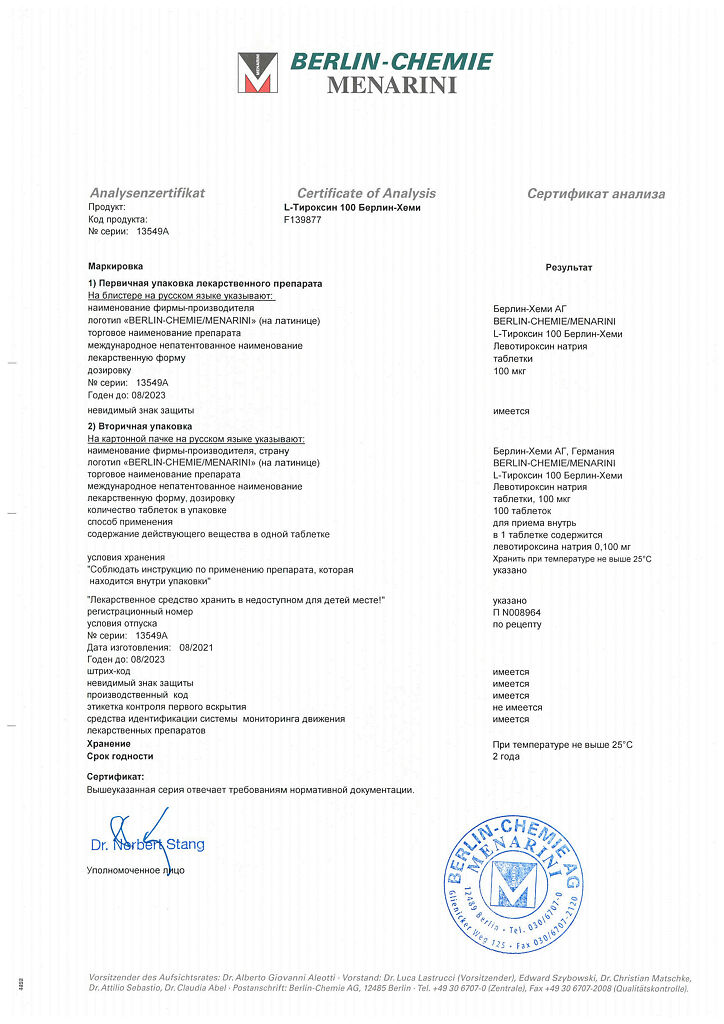
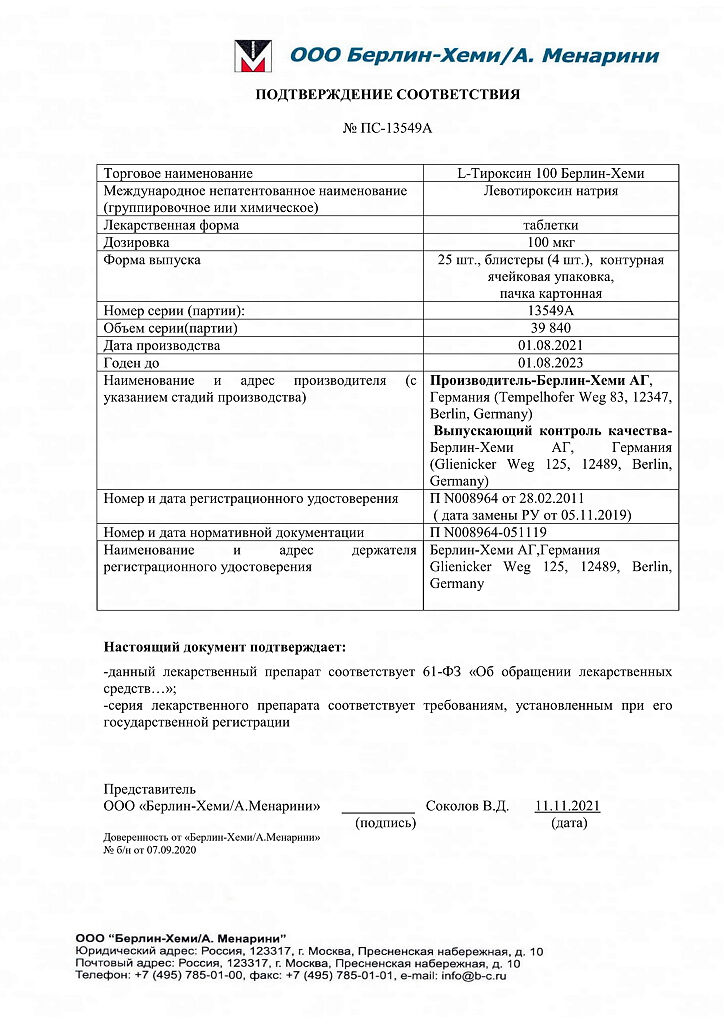
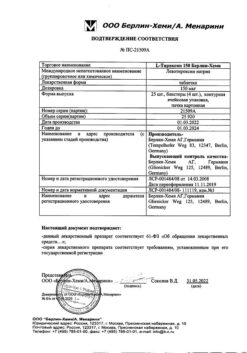
Storage conditions
Storage conditions
Store at a temperature not exceeding 25°C.
Shelf life
Shelf life
2 years.
Manufacturer
Manufacturer
Berlin-Chemie AG, Germany
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store at the temperature not more than 25 ° C. |
| Manufacturer | Berlin-Chemie AG, Germany |
| Medication form | pills |
| Brand | Berlin-Chemie AG |
Other forms…
Related products
Buy L-Tyroxine-100 Berlin Chemi, 100 mcg tablets 100 pcs with delivery to USA, UK, Europe and over 120 other countries.