No products in the cart.
Ketoprovel, 100 mg 30 pcs.
€5.27 €4.68
Description
Pharmacotherapeutic group: nonsteroidal anti-inflammatory drug (NSAID)
ATC code: M01AE03
Pharmacological properties
Pharmacodynamics
Ketoprofen is a non-steroidal anti-inflammatory drug (NSAID). It has anti-inflammatory, analgesic and antipyretic effects. Ketoprofen blocks the action of the enzyme cyclooxygenase 1 and 2 (COX-1 and COX-2) and, partially, lipoxygenase, which leads to suppression of prostaglandin synthesis (including in the central nervous system (CNS), most likely in the hypothalamus). Stabilizes in vitro and in vivo liposomal membranes and inhibits bradykinin and leukotrienes synthesis at high in vitro concentrations.
Ketoprofen has no negative effect on articular cartilage.
Pharmacokinetics
Absorption
Ketoprofen is easily absorbed from the gastrointestinal tract (GIT), bioavailability –
90%. The binding to plasma proteins is 99%. When oral administration of 100 mg of ketoprofen the maximum concentration (Cmax) in blood plasma (10.4 mcg/ml) is reached after 1 hour and 22 minutes.
Distribution
Ketoprofen is 99% bound to blood proteins, mainly to the albumin fraction. The volume of distribution is 0.1 l/kg. Ketoprofen penetrates into the synovial fluid and reaches there a concentration equal to 30% of the blood plasma concentration. Plasma clearance of ketoprofen is approximately 0.08 l/kg/h.
Metabolism and excretion
Ketoprofen is extensively metabolized by liver microsomal enzymes, the half-life (T1/2) is less than 2 hours. Ketoprofen binds to glucuronic acid and is excreted as glucuronide. Ketoprofen has no active metabolites. Up to 80% of ketoprofen is eliminated by the kidneys within 24 hours, mainly in the form of ketoprofen glucuronide. When using ketoprofen at a dose of 100 mg or more, excretion by the kidneys may be difficult.
In patients with hepatic impairment the plasma concentration of ketoprofen is doubled (probably due to hypoalbuminemia and the consequent high level of unbound active ketoprofen): in these patients the minimum therapy dose of ketoprofen should be given.
In patients with renal impairment the clearance of ketoprofen is decreased, but dose adjustment is required only in severe renal impairment. In severe renal failure, most of the ketoprofen is excreted through the intestine. When taking high doses, hepatic clearance is also increased. Up to 40% of ketoprofen is excreted through the intestine. In elderly patients the metabolism and excretion of ketoprofen is slower, which is of clinical importance only in patients with severe renal insufficiency.
Indications
Indications
Symptomatic therapy of painful and inflammatory processes of different origin, including inflammatory and degenerative diseases of the musculoskeletal system:
– rheumatoid arthritis;
– seronegative arthritis: Ankylosing spondyloarthritis (Bechterew’s disease), psoriatic arthritis, reactive arthritis (Reiter’s syndrome);
– gout, pseudopodagra;
– osteoarthritis;
– tendinitis, bursitis, myalgia, neuralgia, radiculitis;
– pain syndrome, including mild, moderate and severe;
– headache;
– toothache;
– Post-traumatic and postoperative pain syndrome;
– pain syndrome in cancer;
– algodysmenorrhea.
Active ingredient
Active ingredient
Composition
Composition
Per tablet:
The active ingredient: ketoprofen – 100 mg.
Auxiliary substances: hyprolose (hydroxypropylcellulose), mannitol (mannitol), croscarmellose sodium (primellose), microcrystalline cellulose, colloidal silicon dioxide (aerosil), magnesium stearate; coating composition: opadray 03F180011 white (hypromellose, titanium dioxide, macrogol).
How to take, the dosage
How to take, the dosage
Orally.
The drug should be swallowed whole during or after a meal, with water or milk (volume of liquid should be at least 100 ml).
Generally, 1 tablet 2 times a day is taken.
Outerine ketoprofen can be combined with rectal suppositories, e.g., a patient can take 1 tablet (100 mg) of ketoprofen in the morning and 1 suppository (100 mg) rectally in the evening.
The maximum dose of ketoprofen is 200 mg/day.
It is not recommended to exceed the maximum daily dose of the drug.
In order to decrease the risk of gastrointestinal (GI) adverse events, patients with risk factors are recommended to take proton pump inhibitors at the same time.
Interaction
Interaction
Ketoprofen may weaken the effect of diuretics and hypotensive drugs and increase the effect of hypoglycemic oral medications and some anticonvulsants (phenytoin).
Combined use with other NSAIDs, salicylates, glucocorticosteroids, ethanol increases the risk of GI adverse events.
Concomitant use with anticoagulants (heparin, warfarin), thrombolytics, antiaggregants (ticlopidine, clopidogrel), pentoxifylline increases the risk of bleeding.
Concomitant use with potassium salts, potassium-saving diuretics, ACE inhibitors, NSAIDs, low molecular weight heparin, cyclosporine, tacrolimus and trimethoprim increases the risk of hyperkalemia.
Ketoprofen increases plasma concentrations of cardiac glycosides, slow calcium channel blockers, lithium drugs, cyclosporine, methotrexate and digoxin. Increases the toxicity of methotrexate and nephrotoxicity of cyclosporine. Concomitant use with probenecid significantly reduces the clearance of ketoprofen in blood plasma.
The concomitant use with glucocorticosteroids and other NSAIDs (including COX-2 selective inhibitors) increases the possibility of side effects (in particular, gastrointestinal side effects).
NSAIDs may decrease the effectiveness of mifepristone. NSAIDs should not be started until 8-12 days after mifepristone has been withdrawn.
Special Instructions
Special Instructions
Ketoprofen should not be combined with other NSAIDs and/or COX-2 inhibitors. During long-term use of NSAIDs it is necessary to periodically assess the clinical blood count, monitor renal and hepatic function, especially in elderly patients (over 65 years), conduct stool analysis for occult blood.
Cautious and more frequent monitoring of blood pressure is necessary when using ketoprofen in patients with arterial hypertension, cardiovascular disease, which leads to fluid retention in the body.
In case of visual disturbances, treatment should be stopped immediately.
Like other NSAIDs, ketoprofen may mask the symptoms of infectious and inflammatory diseases. If there are signs of infection or if there is a deterioration of well-being during the use of the drug, it is necessary to consult a physician immediately.
If there is a history of gastrointestinal contraindications (bleeding, perforation, ulcers), long-term therapy and use of high doses of ketoprofen the patient must be under close medical supervision.
Because of the important role of prostaglandins in maintaining renal blood flow, special caution should be exercised when using ketoprofen in patients with cardiac or renal insufficiency, as well as when treating elderly patients taking diuretics and patients who, for whatever reason, have decreased circulating blood volume. The use of the drug should be discontinued before major surgical intervention.
The use of ketoprofen may affect female fertility, so patients with infertility (including those undergoing evaluation) are not recommended to use the drug.
Influence on the ability to drive vehicles, machinery
There are no data on the negative effect of ketoprofen in the recommended doses on the ability to drive or operate machinery. However, patients who have drowsiness, dizziness or other nerve discomfort, including visual impairment, while using the drug, should refrain from driving and engaging in potentially dangerous activities which require increased concentration and quick psychomotor reactions.
Synopsis
Synopsis
Round biconvex film-coated white or almost white tablets. On the cross section there is a white or almost white color core.
Contraindications
Contraindications
– hypersensitivity to ketoprofen or other components of the drug, as well as salicylates or other NSAIDs;
– Complete or incomplete combination of bronchial asthma, recurrent nasal and paranasal sinus polyposis, and intolerance to acetylsalicylic acid or other NSAIDs (including a history);
– gastric or duodenal ulcer in the acute stage;
– ulcerative colitis Crohn’s disease;
– hemophilia and other blood clotting disorders;
– severe hepatic failure;
– severe renal failure (creatinine clearance less than 30 ml/min);
– decompensated heart failure;
– postoperative period after aortocoronary bypass;
– gastrointestinal, cerebrovascular, or other bleeding (or suspected bleeding);
– progressive renal disease, diverticulitis, active liver disease, inflammatory bowel disease, confirmed hyperkalemia;
– chronic dyspepsia;
– childhood under 15 years of age;
– third trimester of pregnancy;
– breastfeeding period.
With caution
A history of bronchial asthma, clinically significant cardiovascular, cerebro-vascular and peripheral arterial disease, dyslipidemia, progressive liver disease, liver failure, hyperbilirubinemia, alcoholic cirrhosis, renal failure (creatinine clearance 30-60 ml/min), chronic heart failure, arterial hypertension, blood disorders, dehydration, diabetes, anamnestic evidence of gastrointestinal ulceration, presence of Helicobacter pilory infection, severe somatic diseases, advanced age, smoking, concomitant therapy with anticoagulants (e.g., warfarin), anticoagulants (e.g., acetylsalicylic acid), oral glucocorticosteroids (e.g., prednisolone), selective serotonin reuptake inhibitors (e.g., citalopram, sertraline), prolonged use of NSAIDs; elderly patients taking diuretics; patients with decreased blood volume.
Side effects
Side effects
The frequency of side effects has been determined according to the World Health Organization (WHO) classification: very frequently (>1/10), frequently (>1/100, <1/10), infrequently (>1/1000,
<1/100), rarely (>1/10000, < 1/1000), very rare (<1/10000), frequency unknown (frequency of occurrence cannot be determined from available data).
Disorders of the blood and lymphatic system: rare – hemorrhagic anemia; frequency is unknown – agranulocytosis, thrombocytopenia, impaired bone marrow function.
Immune system disorders: frequency unknown – anaphylactic reactions (including anaphylactic shock).
Nervous system disorders: infrequent – headache, dizziness, somnolence; rarely – paresthesias; frequency unknown – seizures, taste disorders.
Psychiatric disorders: frequency unknown – emotional lability.
Visual disorders: rare – blurred vision.
Hearing and labyrinth disorders: rare – tinnitus.
Cardiac disorders: frequency is unknown – heart failure.
Vascular disorders: frequency unknown – increased blood pressure, vasodilation.
Respiratory system, thoracic and mediastinal disorders: rare – exacerbation of bronchial asthma; frequency unknown – bronchospasm (especially in patients with hypersensitivity to NSAIDs), rhinitis.
Gastro-intestinal disorders: frequently – nausea, vomiting, dyspepsia, abdominal pain; infrequently – constipation, diarrhea, bloating, gastritis; rarely – peptic ulcer, stomatitis; very rarely – relapse of ulcerative colitis or Crohn’s disease, gastrointestinal bleeding, perforation.
Hepatic and biliary tract disorders: rare – hepatitis, increased “hepatic” transaminase activity, increased bilirubin concentration.
Skin and subcutaneous tissue disorders: infrequent – skin rash, itching, frequency unknown – photosensitization, alopecia, urticaria, angioedema, erythema, bullous rash, including Stevens-Johnson syndrome, toxic epidermal necrolysis. Renal and urinary tract disorders: frequency unknown – acute renal failure, interstitial nephritis, nephritic syndrome, nephrotic syndrome, abnormal values of renal function parameters.
General disorders and disorders at the site of administration: infrequent – edema; rarely – weight gain; frequency unknown – increased fatigue.
Overdose
Overdose
Symptoms
As with other NSAIDs, ketoprofen overdose may cause nausea, vomiting, abdominal pain, vomiting blood, melena, impaired consciousness, respiratory depression, seizures, renal failure and renal failure.
In case of overdose, gastric lavage and use of activated charcoal are indicated.
Treatment
The treatment is symptomatic. The effects of ketoprofen on the gastrointestinal tract may be alleviated with the use of agents that reduce gastric gland secretion (such as proton pump inhibitors) and prostaglandins.
Pregnancy use
Pregnancy use
Inhibition of prostaglandin synthesis may have undesirable effects on the course of pregnancy and/or fetal development. Evidence from epidemiological studies of the use of prostaglandin synthesis inhibitors in early pregnancy confirms an increased risk of spontaneous abortion and formation of heart defects (about 1-1.5%).
The drug may be used in pregnant women in the first and second trimesters of pregnancy only if the potential benefit to the mother exceeds the possible risk to the fetus.
The use of ketoprofen is contraindicated in pregnant women during the third trimester of pregnancy due to the possibility of development of uterine labor weakness and/or premature closure of the arterial duct, possible increase of bleeding time, oliguria and renal failure.
There are currently no data on excretion of ketoprofen into the breast milk, so if it is necessary to use ketoprofen during breastfeeding, it should be decided to stop breastfeeding.
Similarities
Similarities
Additional information
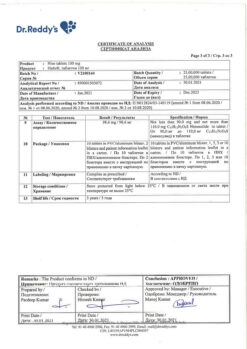
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In a light-protected place at a temperature not exceeding 25 oC. Keep out of the reach of children. |
| Manufacturer | Welfarm, Russia |
| Medication form | pills |
| Brand | Welfarm |
Related products
Buy Ketoprovel, 100 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.