No products in the cart.
Description
The pharmacokinetic properties of darunavir concomitantly administered with ritonavir were evaluated in healthy, adult volunteers and HIV-1-infected patients. Exposure to darunavir was higher in HIV-1-infected patients than in healthy volunteers. The increased exposure to darunavir in HIV-1-infected patients compared with healthy subjects may be due to higher concentrations of alpha-1 acid glycoprotein in HIV-1
infected patients, resulting in increased plasma binding of darunavir to alpha-1 acid glycoprotein and, consequently, increased plasma concentrations.
Darunavir is predominantly metabolized by CYP3A. Ritonavir inhibits CYP3A, thereby increasing plasma concentrations of darunavir.
Expiration
Darunavir is rapidly absorbed after oral administration. Maximum plasma concentrations of darunavir in the presence of low-dose ritonavir are generally reached within 2.5-4.0 hours.
The absolute bioavailability with oral administration of a single dose of 600 mg of darunavir as monotherapy was approximately 37% and increased to approximately 82% in the presence of ritonavir 100 mg taken twice daily. The overall pharmacokinetic enhancement effect of ritonavir was approximately a 14-fold increase with systemic exposure to darunavir when a single 600 mg dose of darunavir was administered orally in combination with ritonavir 100 mg twice daily. The relative bioavailability of darunavir in the presence of a low dose of ritonavir was decreased when the drug was administered on an empty stomach compared to when it was taken together with food. Therefore, Kemeruvir tablets should be taken with ritonavir with food. Distribution
Darunavir is approximately 95% bound to plasma proteins. Darunavir binds mainly to alpha-1 acidic glycoprotein. After intravenous administration, the distribution of darunavir as monotherapy was 88.1 ± 59.01 (mean ± standard deviation) and increased to 131 ± 49.91 (mean ± standard deviation) in the presence of ritonavir 100 mg taken twice daily.
Biotransformation
In vitro experiments with human liver microsomes show that darunavir primarily undergoes oxidative metabolism. Darunavir is largely metabolized by the hepatic CYP system and almost exclusively by the CYP3A4 isoenzyme. A clinical study of 14C-darunavir in healthy volunteers showed that most of the radioactivity in plasma after administration of a single dose of darunavir with 400/100 mg ritonavir was due to the initial active ingredient. At least 3 oxidative metabolites of darunavir were identified in humans; the activity of all of these metabolites against wild-type HIV was less than 1/10 of that of darunavir itself.
Elevation
After a single dose of 400 mg of 14C-darunavir and 100 mg of ritonavir, about 79.5% and 13.9% of the radioactivity was detected in feces and urine, respectively. Unchanged darunavir accounted for about 41.2% and 7.7% of the radioactivity in feces and urine, respectively. The final elimination half-life of darunavir was about 15 h when administered in combination with ritonavir. The clearance of darunavir after intravenous administration of 150 mg was 32.8 L/h (without ritonavir) and 5.91 L/h in the presence of low-dose ritonavir.
Particular groups
Elderly patients
Population pharmacokinetic analysis in HIV-infected patients showed no significant differences in the pharmacokinetic parameters of darunavir in the 18 to 75 year age group (12 HIV-infected patients aged 65 years or older were included in this analysis). However, there are insufficient data on patients over 65 years of age.
Sex differences
Population pharmacokinetic analysis revealed slightly higher (16.8%) concentrations of darunavir in HIV-infected women than in HIV-infected men. This difference is not clinically significant.
Patients with renal impairment
The results of a study using 14C-darunavir in combination with ritonavir showed that about 7.7% of the dose of darunavir taken was excreted unchanged in the urine. The pharmacokinetics of darunavir were not studied in patients with impaired renal function, but population pharmacokinetic analysis showed no significant change in the pharmacokinetic parameters of darunavir in patients with moderate renal impairment (serum creatinine clearance 30-60 ml/min, n=20).
Patients with hepatic impairment
Darunavir is metabolized and excreted primarily by the liver. In a study with multiple administrations of cameruvir in combination with ritonavir (600/100 mg) twice daily, total plasma concentrations of darunavir in patients with mild (Child-Pugh class A, n=8) and moderate (Child-Pugh class B, n=8) hepatic impairment were similar to those in healthy patients. However, concentrations of unbound darunavir were approximately 55% (Child-Pugh grade A) and 100% (Child-Pugh grade B) higher, respectively. The effect of severe hepatic impairment on the pharmacokinetics of darunavir has not been studied.
Pharmacodynamics
Darunavir is an inhibitor of dimerization and catalytic activity of HIV-1 protease. The drug selectively inhibits the cleavage of Gag-Pol HIV polyproteins in virus-infected cells, preventing the formation of complete viral particles.
Darunavir is resistant to mutations that cause resistance to protease inhibitors. Darunavir does not inhibit any of the 13 human cellular proteases studied.
Indications
Indications
Inflammatory and degenerative joint diseases accompanied by pain:
rheumatoid arthritis;
osteoarthritis;
ankylosing spondylitis (ankylosing spondylitis).
Pharmacological effect
Pharmacological effect
The pharmacokinetic properties of darunavir co-administered with ritonavir have been evaluated in healthy adult volunteers and HIV-1-infected patients. Exposure to darunavir was higher in HIV-1 infected patients than in healthy volunteers. The increased exposure of darunavir in HIV-1 infected patients compared with healthy subjects may be explained by higher concentrations of alpha-1 acid glycoprotein in HIV-1
infected patients, which leads to increased binding of darunavir to alpha-1 acid glycoprotein in the blood plasma, and, consequently, to increased plasma concentrations.
Darunavir is predominantly metabolized by CYP3A. Ritonavir inhibits CYP3A, thereby increasing darunavir plasma concentrations.
Suction
Darunavir is rapidly absorbed after oral administration. The maximum plasma concentration of darunavir in the presence of a low dose of ritonavir is generally achieved within 2.5-4.0 hours.
The absolute oral bioavailability of a single 600 mg dose of darunavir as monotherapy was approximately 37% and increased to approximately 82% in the presence of 100 mg ritonavir given twice daily. The overall pharmacokinetic enhancement effect of ritonavir was approximately 14-fold greater than systemic exposure to darunavir when a single dose of darunavir 600 mg was administered orally in combination with ritonavir 100 mg twice daily. When administered on an empty stomach, the relative bioavailability of darunavir in the presence of a low dose of ritonavir is reduced compared to administration with food. Therefore, Kemeruvir tablets should be taken with ritonavir with food. Distribution
Darunavir is approximately 95% bound to plasma proteins. Darunavir binds primarily to alpha-1 acid glycoprotein. Following intravenous administration, the volume of distribution of darunavir as monotherapy was 88.1 ± 59.01 (mean ± standard deviation) and increased to 131 ± 49.91 (mean ± standard deviation) in the presence of ritonavir 100 mg twice daily.
Biotransformation
In vitro experiments with human liver microsomes indicate that darunavir is primarily subject to oxidative metabolism. Darunavir is extensively metabolized by the hepatic CYP system and almost exclusively by the CYP3A4 isoenzyme. A clinical study of 14C-darunavir in healthy volunteers showed that most of the radioactivity in plasma after a single dose of darunavir with ritonavir 400/100 mg was due to the parent active substance. At least 3 oxidative metabolites of darunavir have been identified in humans; The activity of all of these metabolites against wild-type HIV was less than 1/10 that of darunavir itself.
Removal
After a single dose of 400 mg 14C-darunavir and 100 mg ritonavir, approximately 79.5% and 13.9% of radioactivity was detected in feces and urine, respectively. Unmodified darunavir accounted for about 41.2 and 7.7% of the radioactivity in feces and urine, respectively. The terminal half-life of darunavir was approximately 15 hours when taken in combination with ritonavir. The clearance of darunavir after intravenous administration of 150 mg was 32.8 L/h (without ritonavir) and 5.91 L/h in the presence of a low dose of ritonavir.
Special groups
Elderly patients
A population pharmacokinetic analysis in HIV-infected patients showed no significant differences in the pharmacokinetic parameters of darunavir in the age group 18 – 75 years (12 HIV-infected patients aged 65 years and older were included in this analysis). However, there is insufficient data for patients over 65 years of age.
Sex differences
Population pharmacokinetic analysis revealed slightly higher (16.8%) darunavir concentrations in HIV-infected women than in HIV-infected men. This difference is not clinically significant.
Patients with renal failure
Results from a study using 14C-darunavir in combination with ritonavir showed that approximately 7.7% of the administered dose of darunavir was excreted unchanged in the urine. The pharmacokinetics of darunavir have not been studied in patients with impaired renal function, but a population pharmacokinetic analysis showed no significant change in the pharmacokinetic parameters of darunavir in patients with moderately severe renal impairment (serum creatinine clearance 30-60 ml/min, n=20).
Patients with liver failure
Darunavir is metabolized and eliminated primarily by the liver. In a multiple-dose study of Kemeruvir in combination with ritonavir (600/100 mg) twice daily, total plasma concentrations of darunavir in patients with mild (Child-Pugh A, n=8) and moderate (Child-Pugh B, n=8) hepatic impairment were similar to those in healthy patients. However, unbound darunavir concentrations were approximately 55% (Child-Pugh class A) and 100% (Child-Pugh class B) higher, respectively. The effect of severe hepatic impairment on the pharmacokinetics of darunavir has not been studied.
Pharmacodynamics
Darunavir is an inhibitor of dimerization and catalytic activity of HIV-1 protease. The drug selectively inhibits the cleavage of HIV Gag-Pol polyproteins in virus-infected cells, preventing the formation of full-fledged viral particles.
Darunavir is resistant to mutations causing resistance to protease inhibitors. Darunavir does not inhibit any of the 13 human cellular proteases tested.
Special instructions
Special instructions
Patients should be informed that current antiretroviral drugs do not cure HIV infection or prevent HIV transmission. Patients should be advised of the need to take appropriate precautions.
This dosage form with the indicated available dosage is not used in children under 12 years of age and with a body weight of less than 40 kg. Information on treatment with the darunavir/ritonavir combination in patients aged 65 years and older is very limited. Caution is required when treating patients in this age group with darunavir, since they are more likely to experience liver dysfunction, they are more likely to suffer from concomitant diseases, or receive concomitant therapy.
The absolute bioavailability after a single 600 mg dose of darunavir is approximately 37% and increases to approximately 82% when darunavir is administered in combination with 100 mg ritonavir twice daily. There was a 14-fold increase in the plasma concentration of darunavir after taking a single dose of 600 mg in combination with ritonavir (100 mg 2 times a day). Therefore, darunavir should only be taken in combination with a low dose of ritonavir (100 mg) as a pharmacokinetic enhancer. Increasing the indicated dose of ritonavir does not lead to a significant increase in the concentration of darunavir in plasma, therefore it is not recommended to increase the dose of ritonavir.
Severe skin reactions
In 0.4% of patients taking darunavir, severe skin reactions were observed, which may be accompanied by fever and/or increased levels of liver transaminases. Stevens-Johnson syndrome and DRESS syndrome (drug rash with eosinophilia and systemic manifestations) have been reported rarely (<0.1%).
In the post-marketing period, toxic epidermal necrolysis and acute generalized exentematous pustulosis have been reported very rarely (
Rash (all types) was observed in 10.3% of patients receiving darunavir. The rash was generally mild to moderate and was common during the first four weeks of treatment and decreased with continued therapy. In 0.5% of cases, rash was the reason for discontinuation of the darunavir/ritonavir combination.
Rash was observed more frequently in patients receiving both raltegravir and the darunavir/ritonavir combination compared to patients receiving raltegravir and the darunavir/ritonavir combination alone. Drug-related rashes occurred with equal frequency in all three groups. The rash was mild to moderate in severity and did not limit therapy. Rash was not a reason for discontinuation of therapy.
Darunavir contains a sulfonamide group. Darunavir should be used with caution in patients allergic to sulfonamides. In clinical trials of the darunavir/ritonavir combination, the severity and incidence of rash were similar in patients with and without a history of sulfonamide allergy.
Patients with liver disease
Caution is required when using the drug in patients with mild to moderate liver dysfunction. There are no data on the use of the drug in severe liver dysfunction.
Hepatotoxicity
When using the darunavir/ritonavir combination, drug-induced hepatitis (for example, acute hepatitis, cytolytic hepatitis) may develop. Hepatitis was observed in 0.5% of patients receiving darunavir/ritonavir combination therapy. In patients with impaired liver function, incl. with chronic active hepatitis B or C, there is an increased risk of severe liver side effects.
It is necessary to monitor relevant laboratory parameters before prescribing the darunavir/ritonavir combination and during treatment. Consideration should be given to monitoring increases in AST and ALT in patients with chronic hepatitis, liver cirrhosis, or in patients who have had elevated transaminases before starting therapy and especially during the first few months of darunavir/ritonavir combination therapy. If symptoms of liver dysfunction or their progression are detected (including clinically significant increases in liver enzymes and/or symptoms such as fatigue, anorexia, nausea, jaundice, dark urine, liver tenderness, hepatomegaly), the possibility of interrupting or discontinuing therapy with the darunavir/ritonavir combination should be considered.
Patients with kidney disease
The kidneys play a minor role in the clearance of darunavir, therefore, in patients with kidney disease, the overall clearance of darunavir is practically not reduced. Darunavir and ritonavir are highly bound to plasma proteins, so hemodialysis or peritoneal dialysis does not play a significant role in removing these drugs from the body.
Patients with hemophilia
There have been reports of increased bleeding, including spontaneous cutaneous hematomas and hemarthrosis, in patients with hemophilia types A and B treated with protease inhibitors. Some of these patients received clotting factor VIII. In more than half of the reported cases, treatment with protease inhibitors was continued without interruption or resumed after being suspended for some time. A causal relationship between protease inhibitor treatment and increased bleeding in patients with hemophilia has been suggested, but the mechanism of this relationship has not been established. Patients with hemophilia receiving the darunavir/ritonavir combination should be advised of the possibility of increased bleeding.
Diabetes mellitus/hyperglycemia
Newly diagnosed cases of diabetes mellitus, hyperglycemia, or worsening of existing diabetes mellitus have been described in patients receiving antiretroviral therapy, including protease inhibitors. In some of these patients, hyperglycemia was severe and in some cases accompanied by ketoacidosis. Many patients had concomitant diseases, some of which required treatment with drugs that contribute to the development of diabetes mellitus or hyperglycemia.
Fat redistribution and metabolic disorders
Combination antiretroviral therapy may cause redistribution of adipose tissue (lipodystrophy) in HIV-infected patients. An increased risk of lipodystrophy is associated with factors such as older age, as well as long-term therapy with antiretroviral drugs and associated metabolic disorders. When clinically assessing HIV-infected patients receiving antiretroviral drugs, attention should be paid to physical signs of fat redistribution. Determination of lipid levels and fasting blood glucose is recommended. Disorders of lipid metabolism must be treated with appropriate medications.
Osteonecrosis
Despite the multifactorial etiology (use of corticosteroids, alcohol, severe immunosuppression, increased body mass index), cases of osteonecrosis have been reported, especially in patients with advanced HIV disease and/or in patients receiving long-term combination antiretroviral therapy. Patients should be informed of the need to immediately consult a doctor if they experience joint pain or difficulty moving.
Immune reconstitution syndrome
In HIV-infected patients with severe immunodeficiency, when initiating combination antiretroviral therapy, an inflammatory response to asymptomatic or residual opportunistic infections may occur that causes serious clinical complications or worsening of symptoms. Typically, such reactions are observed in the first weeks or months of using combination antiretroviral therapy. The development of cytomegalovirus retinitis, generalized and/or local mycobacterial infections and pneumonia caused by Pneumocystis jiroveci is possible. The severity of any inflammatory symptoms must be determined and appropriate therapy administered. Autoimmune diseases (such as Graves’ disease) have also been reported in association with immune reconstitution inflammatory syndrome. However, the time of initial presentation varied, and the disease could occur many months after onset.
Use during pregnancy and lactation
There have been no comprehensive studies of darunavir in pregnant women. Animal studies have not revealed toxic activity or negative effects on reproductive function or fertility in darunavir. The drug combination darunavir/ritonavir can be prescribed to pregnant women only in cases where the expected benefit to the expectant mother outweighs the potential risk to the fetus. It is not known whether darunavir passes into breast milk in humans. Given the possibility of transmission of HIV through breast milk, and the risk of serious side effects in breastfeeding infants associated with exposure to darunavir, HIV-infected women receiving darunavir should avoid breastfeeding. Experimental studies on animals did not reveal the toxic activity of darunavir or its negative effect on reproductive function and fertility. Darunavir has been shown to be excreted in breast milk in lactating rats. FDA category of effect on the fetus is B.
Features of the effect of the drug on the ability to drive a vehicle or potentially dangerous mechanisms
There have been no studies on the effect of the use of the darunavir/ritonavir combination on the ability to drive a car or drive machinery. However, when considering a patient’s ability to drive and operate machinery, the patient’s clinical condition should be taken into account, as well as the nature of the side effects of darunavir.
Active ingredient
Active ingredient
Darunavir
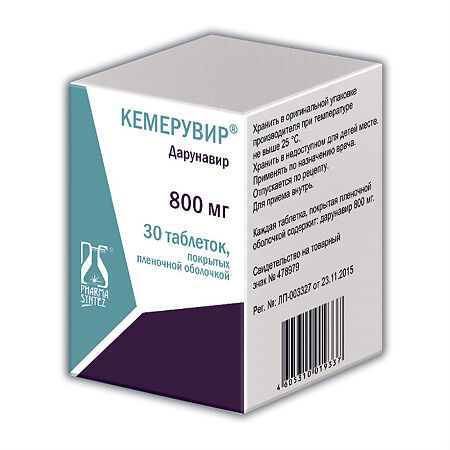
Composition
Composition
One tablet contains
active substance:
Darunavir (amorphous) 800 mg
excipients: low-substituted hyprolose, polysorbate 80, crospovidone, colloidal silicon dioxide, PROSOLV ® EASYtab SP
composition of the film water-soluble shell: hypromellose E5, iron dye yellow oxide (E172), macrogol 6000, talc, titanium dioxide (E171).
Contraindications
Contraindications
– hypersensitivity to darunavir or to any components of the drug.
– severe liver failure (Child-Pugh class C).
– simultaneous use with any of the following drugs is contraindicated due to the expected decrease in the concentration of darunavir and ritonavir in the blood plasma and the potential loss of therapeutic effect (see section “Drug Interactions”).
– simultaneous use of the drug lopinavir/ritonavir with the drug Kemeruvir (their combined use leads to a significant decrease in the concentration of darunavir, which, in turn, can lead to a clinically significant decrease in the therapeutic effect of darunavir.
– simultaneous use of herbal preparations containing St. John’s wort (Hypericum perforatum) with the drug Kemeruvir (due to the risk of reducing plasma concentrations and reducing the clinical effectiveness of darunavir).
– combined use of the drug Kemeruvir with ritonavir in low doses with a number of other drugs (see section “Drug interactions”).
Darunavir boosted with ritonavir inhibits the clearance of active substances that are highly dependent on CYP3A for clearance, resulting in increased exposure to concomitantly administered drugs. Therefore, simultaneous use with medicinal products for which increased plasma concentrations are due to serious and/or life-threatening adverse events is considered contraindicated (applies to darunavir boosted with ritonavir). These active ingredients include:
– alfuzosin (alpha-1 adrenergic receptor blocker)
– amiodarone, bepridil, dronedarone, quinidine, ranolazine, systemic lidocaine (antiarrhythmic/antianginal drugs)
– astemizole, terfenadine (antihistamines)
– colchicine when used in patients with renal and/or liver impairment (anti-gout drug) (see section 4.5)
– ergot derivatives (for example, dihydroergotamine, ergometrine, ergotamine, methylergonovine)
– cisapride (drugs for gastrointestinal motility)
– pimozide, quetiapine, sertindole (neuroleptics)
– triazolam, midazolam for oral administration (sedative/hypnotics) (with caution when administering parenteral midazolam)
– sildenafil – when used to treat pulmonary arterial hypertension, avanafil (PDE-5 inhibitors)
– simvastatin and lovastatin (HMG-CoA reductase inhibitors)
– ticagrelor (antiplatelet drugs).
Side Effects
Side Effects
The following classification of adverse reactions was used depending on the frequency of occurrence: very often (>1/10), often (>1/100.1/1000.1/10,000,
Very common: Diarrhea.
Often:
– nausea, vomiting, abdominal pain, increased amylase activity, dyspepsia, bloating, flatulence
– increase in alanine aminotransferase activity
-headache, peripheral neuropathy, dizziness, insomnia. – rash (macular, maculopapular, papular, erythematous and pruritic), itching. Diabetes mellitus, lipodystrophy (including lipohypertrophy, lipodystrophy, lipoatrophy), hypertriglyceridemia, hypercholesterolemia, hyperlipidemia
– asthenia, fatigue
Uncommon:
– thrombocytopenia, neutropenia, anemia, leukopenia
– tachycardia, increased blood pressure, hot flashes, angina pectoris, prolongation of the QT interval, myocardial infarction
– shortness of breath, cough, nosebleeds, sore throat
– hepatitis, incl. cytolytic, hepatic artery stenosis, hepatomegaly, hepatic steatosis, increased activity of transaminase, alkaline phosphatase, gammaglutamyltransferase, aspartate aminotransferase, increased bilirubin content in the blood.
– apathy, paresthesia, hypoesthesia, dysgeusia
– impaired concentration, memory impairment, lethargy, drowsiness
– depression, anxiety, disorientation, sleep disturbances, unusual dreams, nightmares, decreased libido.
– acute renal failure, nephrolithiasis, increased creatinine concentration, proteinuria, bilirubinuria, dysuria, nocturia, pollakiuria
– hyperemia of the conjunctiva, dryness of the cornea and conjunctiva of the eyes
– vertigo, immune reconstitution syndrome
– hypothyroidism, increased concentration of thyroid-stimulating hormone in the blood.
-generalized rash, allergic dermatitis, angioedema, urticaria, eczema, erythema, hyperhidrosis, night sweats, alopecia, acne, dry skin, changes in nail pigmentation
– myalgia, muscle spasms, muscle weakness, arthralgia, muscle rigidity, pain in the limbs, osteoporosis, increased creatinine phosphokinase activity, osteonecrosis
– erectile dysfunction, gynecomastia
– gout, anorexia, loss of appetite, weight loss, weight gain, hyperglycemia, insulin resistance, decreased concentration of high-density lipoproteins, increased appetite, polydipsia, increased blood lactate dehydrogenase activity. Increased body temperature, chest pain, peripheral edema, feeling of malaise, chills, feeling of heat, irritability, pain, pathological dry skin
– herpetic infection
Rarely:
– eosinophilia
– myocardial infarction, angina pectoris, QT interval prolongation, sinus bradycardia, palpitations
– rhinorrhea
– stomatitis, vomiting with blood, cheilitis, dry mucous membrane of the lips, coating on the tongue
– fainting, convulsions, sleep phase disturbance, ageusia, confusion, mood swings, anxiety
– decreased creatinine clearance
– visual impairment
– arthritis, joint stiffness, musculoskeletal stiffness.
– chills, feeling unwell, xerosis of the skin
– drug rash with eosinophilia and systemic manifestations (DRESS syndrome), Stevens-Johnson syndrome, erythema multiforme, skin lesions, xeroderma, dermatitis, seborrheic dermatitis. Identified in the post-marketing period: toxic epidermal necrolysis, acute generalized exentematous pustulosis
Description of some side effects
Rash
In clinical studies, mild to moderate rash was primarily observed. The rash most often appeared during the first four weeks of therapy and disappeared with continued use of the drug. If severe skin reactions develop, see the “Special Instructions” section.
In clinical trials in treatment-experienced patients, rash, regardless of cause, occurred more frequently with regimens containing darunavir and raltegravir than with darunavir without raltegravir and raltegravir without darunavir. Drug-related rashes occurred with similar frequency. Rash that occurred in clinical studies was mild to moderate and did not lead to discontinuation of therapy.
Lipodystrophy
Combination antiretroviral therapy causes fat redistribution (lipodystrophy) in patients with HIV. Lipodystrophy manifested itself as loss of peripheral and facial subcutaneous fat, increase in intra-abdominal and visceral fat, breast hypertrophy and accumulation of dorsocervical fat (“bull hump”).
Metabolic disorders
Combination antiretroviral therapy causes metabolic disorders such as hypertriglyceridemia, hypercholesterolemia, insulin resistance, hyperglycemia and hyperlactatemia
Musculoskeletal disorders
Increased creatine phosphokinase activity, myalgia, myositis and rhabdomyolysis (rarely) have been reported with the use of protease inhibitors, especially in combination with nucleoside reverse transcriptase inhibitors
Cases of osteonecrosis have been reported, particularly in patients with established risk factors, advanced HIV disease, or long-term combination antiretroviral therapy. The incidence of osteonecrosis is unknown
Immune reconstitution syndrome
In patients with HIV and severe immunodeficiency, inflammatory reactions to asymptomatic or residual infections may occur at the time of initiation of combination antiretroviral therapy. Autoimmune diseases (eg, Graves’ disease) have also been observed. However, the time to onset of illness may vary, and such illnesses may begin months after initiation of therapy.
Bleeding in patients with hemophilia
An increased incidence of spontaneous bleeding has been observed in patients with hemophilia receiving anti-retroviral protease inhibitors.
Patients with coinfections with viral hepatitis B and/or C
Patients with these infections were more likely to have increased liver transaminase activity than patients without concomitant viral hepatitis B or C.
Interaction
Interaction
Interaction studies were conducted in adults only.
Darunavir and ritonavir are inhibitors of the CYP3A isoenzyme. The simultaneous use of the combination of Kemeruvir/ritonavir and drugs that are predominantly metabolized by the CYP3A isoenzyme may cause an increase in plasma concentrations of such drugs, which, in turn, can lead to an increase in the overall exposure of such drugs, which may cause an increase or prolongation of the therapeutic effect, as well as cause side effects.
Kemeruvir, when used concomitantly with a low dose of ritonavir, should not be combined with drugs whose clearance is largely determined by the CYP3A isoenzyme and whose elevated plasma concentrations can cause serious and/or life-threatening adverse reactions (narrow therapeutic range). These drugs include amiodarone, bepridil, quinidine, systemic lidocaine, astemizole, alfuzosin, terfenadine, sildenafil (used to treat pulmonary arterial hypertension), oral midazolam, triazolam, cisapride, primozide, sertindole, simvastatin, lovastatin, and ergot alkaloids (eg, ergotamine, dihydroergotamine, ergonovine and methylergometrine).
The pharmacokinetic enhancement effect of ritonavir was an approximately 14-fold increase in the total exposure of darunavir when a single dose of darunavir 600 mg was administered orally in combination with ritonavir 100 mg twice daily. Therefore, Kemeruvir should only be used in combination with a low dose of ritonavir, which is used as an enhancer of pharmacokinetic properties.
A clinical study using a mixture of drugs metabolized by the cytochromes CYP2C9, CYP2C19 and CYP2D6 showed increased activity of CYP2C9 and CYP2C19 and inhibition of CYP2D6 activity in the presence of Kemeruvir/ritonavir, which may be attributable to the presence of low dose ritonavir. Concomitant use of darunavir and ritonavir and drugs that are predominantly metabolized by cytochrome CYP2D6 (such as flecainide, propafenone, metoprolol) may lead to increased plasma concentrations of these drugs, which may increase or prolong their therapeutic effect and adverse reactions. Concomitant use of darunavir and ritonavir and medicinal products that are predominantly metabolized by CYP2C9 (such as warfarin) and CYP2C19 (such as methadone) may result in a decrease in the overall effect of such medicinal products, which may reduce or reduce their therapeutic effect.
Although the effect on CYP2C8 has only been studied in vitro, concomitant use of darunavir and ritonavir and drugs that are predominantly metabolized by CYP2C8 (eg, paclitaxel, rosiglitazone, repaglinide) may lead to a decrease in the overall exposure of such drugs, which may reduce or reduce their therapeutic effect.
Medicines that affect the effect of darunavir/ritonavir
Darunavir and ritonavir are metabolized by the enzyme CYP3A. Drugs that induce CYP3A enzyme activity are expected to increase the clearance of darunavir and ritonavir, which in turn will lead to decreased plasma concentrations of darunavir and ritonavir (eg, rifampicin, St. John’s wort, lopinavir).
Concomitant use of darunavir and ritonavir and other medicinal products that inhibit the CYP3A enzyme may reduce the clearance of darunavir and ritonavir and may lead to increased plasma concentrations of darunavir and ritonavir (for example, indinavir, systematic azoles such as ketoconazole and clotrimazole).
Overdose
Overdose
Treatment: specific antidote is unknown. In case of overdose, general supportive therapy should be carried out with monitoring of basic physiological parameters. To remove unabsorbed drug, gastric lavage or a cleansing enema is indicated. Activated carbon can be used. Darunavir is highly bound to plasma proteins and is therefore not removed in significant quantities by dialysis.
Manufacturer
Manufacturer
Pharmasintez JSC, Russia
Additional information
| Manufacturer | Pharmasintez JSC, Russia |
|---|---|
| Medication form | pills |
| Brand | Pharmasintez JSC |
Related products
Buy Kemeruvir, 800 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.