No products in the cart.
Description
Kaletra® is a combination drug that contains lopinavir and ritonavir.
Lopinavir is an inhibitor of HIV-1 and HIV-2 proteases of human immunodeficiency virus (HIV) and provides antiviral activity of the drug.
Inhibition of HIV proteases prevents synthesis of virus proteins and prevents cleavage of gag-pol polypeptide, which leads to formation of immature and unable to infect virus.
Ritonavir inhibits CYP3A isoenzyme-mediated metabolism of lopinavir in the liver, which leads to increased plasma concentrations of lopinavir. Ritonavir is also an HIV protease inhibitor.
Resistance
HIV-1 isolates with reduced sensitivity to lopinavir have been selected in vitro. The presence of ritonavir did not affect the isolation of lopinavir-resistant viruses in vitro.
In the phase III study, antiretroviral (ARV) treatment of previously untreated patients was analyzed with viral isolates from each patient with plasma HIV RNA concentrations greater than 400 copies/mL at weeks 24, 32, 40, and/or 48. All 37 evaluable patients treated with lopinavir/ritonavir showed no evidence of genotypic or phenotypic resistance to lopinavir/ritonavir. No lopinavir/ritonavir resistance was found in children who had not previously received antiretroviral therapy.
In phase II clinical trials of Kaletra® among 227 HIV-infected patients receiving and not receiving prior antiretroviral therapy, 4 of 23 patients with virologic ineffectiveness of therapy (HIV RNA >400 copies/mL) was found to decrease sensitivity to lopinavir after 12-100 weeks of therapy with Kaletra®; 3 of 4 patients had previously received one of the HIV protease inhibitors (nelfinavir, saquinavir or indinavir) and 1 of 4 patients had received combined therapy with HIV protease inhibitors (indinavir, saquinavir and ritonavir).
All 4 patients had at least 4 mutations associated with resistance to HIV protease inhibitors before starting therapy with Kaletra®. A further increase in viral load was associated with the emergence of additional mutations associated with the development of resistance to HIV protease inhibitors.
However, these data are insufficient to identify the mutations responsible for the development of lopinavir resistance.
Cross-resistance
There is insufficient data to date on the development of cross-resistance with lopinavir/ritonavir therapy.
The virologic response to lopinavir/ritonavir therapy was altered in the presence of three or more of the following amino acid substitutions in the HIV protease gene: L10F/I/R/V, K20M/N/R, L24I, L33F, M36I, I47V, G48V, I54L/T/V, V82A/C/F/S/T, I84V.
The clinical significance of reduced sensitivity to lopinavir was studied in vitro based on virologic response to lopinavir/ritonavir therapy depending on baseline genotype and virus phenotype in 56 patients with HIV RNA above 1000 copies/mL previously treated with nelfinavir, indinavir, saquinavir or ritonavir (study M98-957).
In this study, patients were treated with lopinavir/ritonavir at one of two doses in combination with efavirenz and nucleoside reverse transcriptase inhibitors. Prior to therapy, the EC50 (the drug concentration needed to suppress replication of 50% of viruses) of lopinavir against 56 strains of the virus was 0.5-96 times the EC50 for the “wild-type” virus. Fifty-five percent (31/56) of the virus strains exhibited more than a 4-fold decrease in sensitivity to lopinavir, with an average decrease in sensitivity to lopinavir of 27.9 times among the 31 strains.
Forty-eight weeks after initiation of lopinavir/ritonavir, efavirenz, and nucleoside reverse transcriptase inhibitors, HIV RNA concentrations ≤400 copies/mL were determined in 93% (25/27), 73% (11/15), and 25% (2/8) of patients with initial sensitivity to lopinavir reduced by a factor ≤10, 10-40, and ≥40 times, respectively. In these groups, HIV RNA concentrations were ≤50 copies/mL in 81% (22/27), 60% (9/15), and 25% (2/8) of patients, respectively.
Pharmacokinetics
The pharmacokinetics of lopinavir in combination with ritonavir were studied in healthy volunteers and HIV-infected patients; no significant differences were found between the two groups. Lopinavir is almost completely metabolized by the CYP3A isoenzyme. Ritonavir inhibits the metabolism of lopinavir and causes increased plasma concentrations.
When lopinavir/ritonavir was administered at a dose of 400/100 mg twice daily, average equilibrium plasma concentrations of lopinavir in HIV-infected patients were 15-20 times higher than those of ritonavir, and plasma concentrations of ritonavir were less than 7% of those when ritonavir was given at 600 mg twice daily. The in vitro EC50 of lopinavir is about 10 times lower than that of ritonavir. Thus, the antiviral activity of the combination of lopinavir and ritonavir is determined by lopinavir.
On ingestion, plasma concentrations of lopinavir and ritonavir after two 200/50 mg tablets are equivalent to three 133/33 mg capsules with minimal variability in pharmacokinetics.
Intake
Intake
. In a pharmacokinetic study involving HIV-positive patients (n=19), when 400/100 mg lopinavir/ritonavir was taken twice daily with food for three weeks, the mean maximum plasma concentration (Cmax) of lopinavir 9.8 ± 3.7 µg/mL was determined to be approximately four hours after taking the drug. The mean equilibrium concentration before the morning dose was 7.1 ± 2.9 µg/ml and the minimum concentration within the dosing interval was 5.5 ± 2.7 µg/ml.
The area under the concentration-time curve (AUC) of lopinavir averaged 92.6 ± 36.7 µg⋅h/mL within 12 hours of drug administration. Absolute bioavailability of lopinavir in combination with ritonavir in humans has not been established.
Distribution
In equilibrium, approximately 98 – 99% of lopinavir is bound to plasma proteins. Lopinavir binds to alpha1-acid glycoprotein (ACG) and albumin, but lopinavir has a higher affinity for ACG. In equilibrium, the binding of lopinavir to plasma proteins remains constant across the range of reported concentrations produced after administration of 400/100 mg lopinavir/rntonavir twice daily and is comparable in healthy volunteers and HIV-positive patients.
Metabolism
Lopinavir has been shown in in vitro studies to undergo predominantly oxidative metabolism involving the hepatocyte cytochrome P450 system, mainly through the CYP3A isoenzyme. Ritonavir is a potent inhibitor of CYP3A isoenzyme that inhibits lopinavir metabolism, which provides increased concentrations of lopinavir in blood plasma. After a single 400/100 mg dose of lopinavir/ritonavir (with 14C-labeled lopinavir), 89% of the radioactivity is provided by the original drug. At least 13 oxidative metabolites of lopinavir have been identified in humans.
Ritonavir is able to induce cytochrome P450 isoenzymes, leading to induction of its own metabolism. During long-term use, lopinovir concentrations before the next dose decreased over time, stabilizing after approximately 10-16 days.
Elevation
After 400/100 mg administration of 14C-lopinavir/ritonavir after eight days, approximately 10.4 ± 2.3% and 82.6 ± 2.5% of the 14C-lopinavir dose taken were detected in the urine and feces, respectively. And unchanged lopinavir is 2.2 and 19.8%, respectively. After long-term use, less than 3% of lopinavir doses are excreted unchanged through the kidneys. The clearance (CL/F) of lopinavir when taken orally is 5.98 +/- 5.75 l/h.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Interaction
Interaction
Special Instructions
Special Instructions
Contraindications
Contraindications
Side effects
Side effects
Overdose
Overdose
Additional information
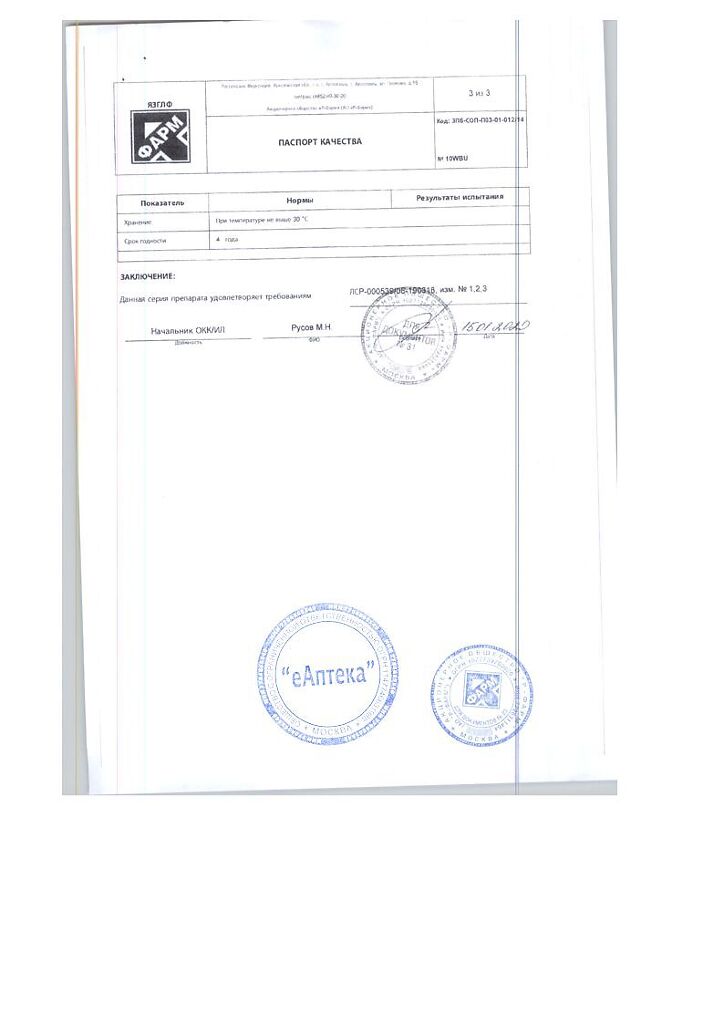
| Conditions of storage | At the temperature from 15 to 30 ° C. Keep out of reach of children. |
|---|---|
| Manufacturer | R-Pharm AO, Russia |
| Medication form | pills |
| Brand | R-Pharm AO |
Related products
Buy Kaletra, 200 mg+50 mg 120 pcs with delivery to USA, UK, Europe and over 120 other countries.