No products in the cart.
Description
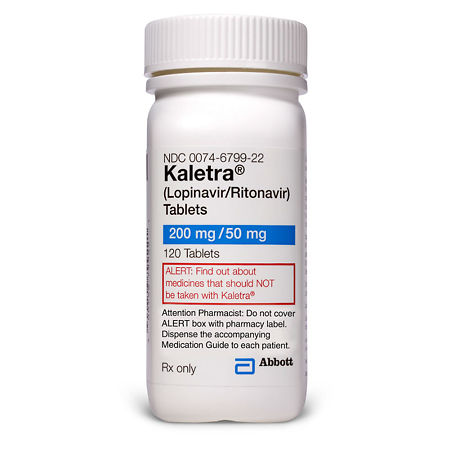
A combined antiviral drug that contains lopinavir and ritonavir.
Lopinavir is an inhibitor of HIV-1 and HIV-2 proteases and provides the antiviral activity of Kaletra. Inhibition of HIV proteases prevents the synthesis of viral proteins, which leads to the formation of immature and non-infectious virus.
Ritonavir is an inhibitor of HIV-1 and HIV-2 aspartyl-proteases and an active peptidomimetic. Inhibition of HIV proteases prevents the breakage of the gag-pol bond of the polyprotein, which also leads to the formation of an immature and incapable of infecting virus. Ritonavir has selective affinity for HIV protease and shows little activity against human aspartyl protease.
It inhibits CYP3A-mediated lopinavir metabolism in the liver, resulting in increased plasma lopinavir concentrations.
Indications
Indications
Acquired human immunodeficiency syndrome (HIV infection) in adults and children from 3 years old as part of combination therapy.
Active ingredient
Active ingredient
Composition
Composition
Tablets 200 mg+50 mg:
1 tabletcalopinavir 200 mg
ritonavir 50 mg
Associates:
copovidone K28 – 853.8 mg,
sorbitan laurate – 83.9 mg,
silicon dioxide colloid – 12 mg;
second layer – sodium stearyl fumarate – 12.3 mg,
silicon dioxide colloid – 8 mg.
How to take, the dosage
How to take, the dosage
The tablets should be taken orally, regardless of meals; they should be swallowed whole and should not be chewed or crushed.
Adults
For patients who have not previously received antiretroviral therapy, the recommended dose of Kaletra is 400/100 mg (2 tablets) 2 times daily or 800/200 mg (4 tablets) once daily.
For patients who have previously received antiretroviral therapy, the recommended dose of Kaletra is 400/100 mg (2 tablets) 2 times daily. Once-daily use has not been studied in these patients, so it is not recommended.
Companion therapy
The use of Kaletra tablets in combination with omeprazole and ranitidine does not require dose adjustments.
In combination with efavirenz, nevirapine, amprenavir, nelfinavir, Kaletra tablets may be used in a dose of 400/100 mg (2 tablets) 2 times daily without dose adjustment. Kaletra tablets should not be administered once daily if concomitantly taken with these drugs.
In children
In children with a body weight of 40 kg or more (or body surface area >1.3 m2), Kaletra tablets are administered in a dose of 400/100 mg (2 tablets) 2 times daily. In children with body weight ⤠40 kg (or body surface area 2) it is recommended to use Kaletra® solution for oral administration. The use of Kaletra tablets 1 time/day in children has not been studied.
The body surface area (BSA) can be calculated using the following formula: PPT (m2)= square root of (height in cm à body weight in kg/3600).
Interaction
Interaction
Lopinavir/ritonavir in vitro and in vivo inhibits CYP3A isoenzyme. Concomitant use of Kaletra and drugs metabolized by CYP3A isoenzymes (including dihydropyridine calcium antagonists, HMG-CoA reductase inhibitors, immunosuppressants and sildenafil) may increase their plasma concentrations and enhance or prolong therapeutic effect and side effects.
The risk of a significant increase in AUC (â¥3 times) during treatment with lopinavir/ritonavir is highest with concomitant use of drugs that are actively metabolized by CYP3A isoenzymes and are metabolized during first passage through the liver. The section “Contraindications” lists drugs that should not be combined with lopinavir/ritonavir, given the severity of the interaction and the possibility of serious adverse reactions.
Lopinavir/ritonavir does not inhibit the CYP2D6, CYP2C9, CYP2C19, CYP2E1, CYP2B6 and CYP1A2 isoenzymes at therapeutic levels.
Lopinavir/ritonavir has been found to induce its own metabolism in vivo and cause increased biotransformation of some drugs that are metabolized by cytochrome P450 system isoenzymes and by glucuronidation.
Lopinavir/ritonavir is metabolized by CYP3A isoenzymes. Concomitant use of lopinavir/ritonavir with inducers of this isoenzyme may reduce plasma concentrations of lopinavir and its therapeutic effect. Other drugs that inhibit CYP3A isoenzymes may cause an increase in plasma concentrations of lopinavir, although these changes have not been noted with concomitant use of ketoconazole.
Nucleoside reverse transcriptase inhibitors (NRTIs)
Stavudine and lamivudine
. No changes in the pharmacokinetics of lopinavir were observed when combined with ritonavir or when lopinavir/ritonavir was used in combination with stavudine and lamivudine.
Didanosine
Didanosine is recommended to be taken on an empty stomach. Because of this, didanosine can be prescribed together with lopinavir/ritonavir outside of meals.
Zidovudine and abacavir
Lopinavir/ritonavir induces glucuronidation; therefore, zidovudine and abacavir concentrations may be reduced. The clinical significance of a possible interaction is unknown.
Tenofovir
Lopinavir/ritonavir has been shown to cause increased concentrations of tenofovir. The mechanism of interaction is not known. In patients receiving lopinavir/ritonavir concomitantly with tenofovir, the side effects of the latter should be monitored.
All other NRTIs
In treatment with protease inhibitors, especially in combination with NRTIs, increased CPK activity, myalgia, myositis and rarely rhabdomyolysis have been observed.
Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
Nevirapine
In healthy volunteers treated with nevirapine and lopinavir/ritonavir, there was no change in the pharmacokinetics of lopinavir. In HIV-infected children, a decrease in lopinavir concentrations was observed with concomitant use of nevirapine. It is thought that the effect of nevirapine in HIV-positive adults may be similar to that in children, which may result in lower lopinavir concentrations. The clinical significance of the pharmacokinetic interaction is unknown.
Lopinavir/ritonavir should not be used once daily in combination with nevirapine.
Efavirenz
. Increasing the dose of lopinavir/ritonavir tablets to 600/150 mg (3 tablets) 2 times/day in combination with efavirenz results in a 36% increase in plasma lopinavir and 56% to 92% increase in ritonavir concentration compared to taking lopinavir/ritonavir tablets at 400/100 mg 2 times/day without efavirenz.
Efavirenz and nevirapine may induce CYP3A4 isoenzyme activity and therefore reduce concentrations of other protease inhibitors when used in combination with lopinavir/ritonavir. It is not recommended to use lopinavir/ritonavir once daily in combination with evafirenz.
Delavirdine
Delavirdine may cause increased plasma concentrations of lopinavir.
Protease inhibitors
Amprenavir
Lopinavir/ritonavir may cause increased concentrations of amprenavir. When treated with amprenavir at a dose of 750 mg 2 times/day in combination with lopinavir/ritonavir, there is an increase in AUC and Cmin compared to those when using amprenavir at a dose of 1200 mg 2 times/day, while Cmax is not significantly changed. Concomitant therapy with lopinavir/ritonavir and amprenavir causes a decrease in lopinavir concentrations. Lopinavir/ritonavir should not be used once daily in combination with amprenavir.
Fosamprenavir
The combined use of lopinavir/ritonavir and fosamprenavir has been shown to be associated with decreased concentrations of fosamprenavir and lopinavir. Adequate doses of the two drugs when used in combination have not been established (in terms of safety and efficacy).
Indinavir
Indinavir. Lopinavir/ritonavir may cause increased concentrations of indinavir (when combined with lopinavir/ritonavir at a dose of 600 mg twice daily, Cmax decreased and Cmin increased compared to those with indinavir at 800 mg three times daily, with no significant change in AUC). When prescribing lopinavir/ritonavir at a dose of 400/100 mg 2 times/day, it may be necessary to reduce the dose of indinavir. Lopinavir/ritonavir should not be used once daily in combination with indinavir.
Nelfinavir
Lopinavir/ritonavir may cause increased concentrations of nelfinavir and its M8 metabolite. Concomitant administration of nelfinavir at a dose of 1000 mg 2 times/day with lopinavir/ritonavir shows an increase in Cmin compared to that when treated with nelfinavir at a dose of 1250 mg 2 times/day, while the AUC and Cmax are not significantly changed. The combination of lopinavir/ritonavir with nelfinavir leads to a decrease in lopinavir concentrations. Lopinavir/ritonavir should not be used once daily in combination with nelfinavir.
Ritonavir
The concomitant use of lopinavir/ritonavir with ritonavir at a dose of 100 mg 2 times/day showed a 33% increase in lopinavir AUC and 64% increase in Cmin compared to those with lopinavir/ritonavir alone at 400/100 mg 2 times/day.
Saquinavir
Lopinavir/ritonavir may cause increased concentration of saquinavir. Concomitant administration of saquinavir at a dose of 800 mg 2 times/day with lopinavir/ritonavir resulted in increased AUC, Cmax and Cmin compared to those with saquinavir at a dose of 1200 mg 3 times/day. When prescribing lopinavir/ritonavir at a dose of 400/100 mg 2 times/day, it may be necessary to reduce the dose of saquinavir. The use of lopinavir/ritonavir in combination with saquinavir once daily has not been studied.
Tipranavir
The concomitant use of tipranavir at a dose of 500 mg 2 times daily with ritonavir at a dose of 200 mg 2 times daily and lopinavir/ritonavir at a dose of 400/100 mg 2 times daily decreases AUC and Cmin by 47% and 70%, respectively. Therefore, concomitant use of lopinavir/ritonavir and tipranavir with low-dose ritonavir is not recommended.
Other drugs
The antiarrhythmic drugs (amiodarone, bepridil, lidocaine and quinidine)
Concentrations of amiodarone, bepridil, lidocaine and quinidine may be increased when concomitantly administered with lopinavir/ritonavir. Caution should be exercised when combining Kaletra with the above drugs and, if possible, their plasma concentrations should be monitored.
Digoxin
Concomitant use with ritonavir at a dose of 300 mg every 12 hours significantly increases digoxin concentrations. Caution should be exercised when combining Kaletra with digoxin and serum concentrations of digoxin should be monitored.
Drugs prolonging the QT interval
Phenyramine, quinidine, erythromycin, clarithromycin may increase concentrations under lopinavir/ritonavir influence with subsequent prolongation of the QT interval and cardiac adverse events. Particular caution should be exercised when prescribing lopinavir/ritonavir with drugs that prolong the QT interval.
Antineoplastic agents
Concomitant use with ritonavir/lopinavir may increase plasma concentrations of anticancer drugs such as vincristine and vinblastine, with a subsequent potential increase in the frequency of adverse events that are common with these drugs.
Anticoagulants
Lopinavir/ritonavir may cause decreased warfarin concentrations. It is recommended to monitor the international normalized ratio (INR).
Antidepressants (trazodone)
The combination of ritonavir and trazodone may increase trazodone concentrations and cause side effects (including nausea, dizziness, hypotension, syncope). Concomitantly with a CYP3A isoenzyme inhibitor such as lopinavir/ritonavir, trazodone should be used cautiously, possibly with lowering the dose of trazodone.
Anticonvulsants
Phenobarbital, phenytoin and carbamazepine induce the CYP3A4 isoenzyme and may decrease lopinavir concentrations. Lopinavir/ritonavir should not be administered once daily in combination with phenobarbital, phenytoin or carbamazepine. Concomitant use of phenytoin and lopinavir/ritonavir may be accompanied by a moderate decrease in the equilibrium concentration of phenytoin; therefore, plasma concentrations of phenytoin should be monitored when taken with ritonavir/lopinavir.
Antifungal agents
The serum concentrations of itraconazole and ketoconazole may increase with lopinavir/ritonavir. Itraconazole and ketoconazole in high doses (>200 mg/day) in combination with lopinavir/ritonavir are not recommended.
Ritonavir at a dose of 400 mg every 12 hours caused an average reduction in the equilibrium AUC of voriconazole by 39%; accordingly, concomitant use of voriconazole with Kaletra is not recommended.
Antibacterials
Lopinavir/ritonavir may cause a moderate increase in the AUC of clerithromycin. In patients with impaired renal or hepatic function it is reasonable to reduce the dose of clarithromycin while taking lopinavir/ritonavir at the same time.
Antimycobacterials
Concomitant use of rifabutin and lopinavir/ritonavir for 10 days increases Cmax and AUC of rifabutin (the drug itself and the active 25-O-desacetyl metabolite) by 3.5 and 5.7 times, respectively. Given these data, a 75% reduction in the dose of rifabutin (i.e., to 150 mg daily or 3 times weekly) is recommended for lopinavir/ritonavir treatment. Additional dose reductions may be required.
Given the significant decrease in lopinavir concentrations when used concomitantly with rifampicin, rifampicin should not be prescribed in combination with Kaletra. This combination may lead to a worsening of the virologic response and potential development of resistance to lopinavir/ritonavir, the entire class of protease inhibitors or other antiretrovirals.
Antiparasitic agents
The treatment with lopinavir/ritonavir may decrease the therapeutic concentration of atovachone. It may be necessary to increase concentrations of the latter.
GCS
Dexamethasone may increase CYP3A4 isoenzyme activity and decrease lopinavir concentrations.
Combination with lopinavir/ritonavir may increase fluticasone concentrations and decrease serum cortisol concentrations.
Dihydropyridine calcium antagonists
The serum concentrations of felodipine, nifedipine and nicardipine may increase when combined with lopinavir/ritonavir.
Erectile enhancement agents
Sildenafil should be used cautiously at lower doses (25 mg every 48 hours) and adverse events should be monitored more frequently.
Tadalafil should be used cautiously at lower doses (no more than 10 mg every 72 hours) and adverse events should be monitored more frequently.
Vardenafil should be used cautiously at lower doses (no more than 2.5 mg every 72 hours) and more frequently monitored for adverse events.
Medicinal herbs
Prevent administration of preparations containing St. John’s wort in lopinavir/ritonavir treatment, because this combination leads to decreased plasma concentrations of lopinavir/ritonavir and decreased therapeutic efficacy or resistance, possibly due to induction of CYP3A4.
HMG-CoA reductase inhibitors
Lopinavir/ritonavir can cause significant increases in plasma concentrations of HMG-CoA reductase inhibitors that are metabolized by CYP3A4 isoenzyme, such as lovastatin and simvastatin. Increased concentrations of statins may lead to myopathy, including rhabdomyolysis, therefore their combination with lopinavir/ritonavir is not recommended.
Rosuvastatin and atorvastatin, whose metabolism is less dependent on the CYP3A4 enzyme, should be used with ritonavir/lopinavir with caution in minimal doses. When used in combination with lopinavir/ritonavir an increase in Cmax and AUC of atorvastatin 4.7 and 5.9 times was observed, respectively, which increases the risk of serious adverse reactions of myopathy and rhabdomyolysis.
There is no evidence of clinically significant interaction of lopinavir ritonavir with pravastatin. The metabolism of pravastatin and fluvastatin is independent of CYP3A4, so they should not interact with lopinavir/ritonavir. If treatment with HMG-CoA reductase inhibitors is indicated while lopinavir/ritonavir is in use, pravastatin or fluvastatin are recommended.
Special Instructions
Special Instructions
Hepatic impairment
Lopinavir/ritonavir is predominantly metabolized by the liver. Therefore, special caution should be exercised when using this drug in patients with reduced hepatic function. Lopinavir/ritonavir has not been studied in patients with severe hepatic impairment.
Pharmacokinetic data show an increase in plasma concentrations of lopinavir by approximately 30% and a decrease in plasma protein binding in patients co-infected with HIV and hepatitis C virus and mild to moderate hepatic impairment. Patients with basic hepatitis B or C disease or significant increase of liver transaminase activity before treatment can be in high risk group with further increase of transaminase activity.
There have been cases of hepatic dysfunction, including several deaths, since the drug was marketed, mostly among patients with advanced HIV infection who were simultaneously taking medications to treat the underlying disease, chronic hepatitis or cirrhosis. A causal relationship with lopinavir/ritonavir treatment has not been established. In these patients, more careful monitoring of AST/ALT activity is necessary, especially during the first few months of lopinavir/ritonavir treatment.
Diabetes mellitus/hyperglycemia
The initial diagnosis of diabetes mellitus, exacerbation of previously diagnosed diabetes mellitus, and hyperglycemia has been reported in post-marketing follow-up in HIV-positive patients treated with HIV protease inhibitors. Some patients required administration or adjustment of doses of insulin or oral hypoglycemic agents. In some cases, diabetic ketoacidosis occurred. In those patients who discontinued treatment with HIV protease inhibitors, hyperglycemia sometimes persisted. Because these effects were reported voluntarily during clinical practice, it is not possible to estimate the frequency of these effects or to establish a causal relationship between treatment with HIV protease inhibitors and these effects.
Pancreatitis
In patients treated with lopinavir/ritonavir, pancreatitis has been reported, including in those patients with significant elevations in triglyceride concentrations. Fatal cases have been reported. Although a causal relationship with lopinavir/ritonavir has not been established, significant increases in triglyceride concentrations are a risk for pancreatitis. Patients with advanced HIV infection may be at increased risk for increased triglyceride concentrations and pancreatitis, and patients with a history of pancreatitis may be at risk for recurrent pancreatitis during treatment with lopinavir/ritonavir.
Hemophilia
There have been reported cases of increased bleeding, including spontaneous formation of subcutaneous hematomas and development of hemarthrosis, in patients with hemophilia type A and B treated with HIV protease inhibitors. Additional doses of clotting factor VIII were administered to some patients. In more than half of the cases reported, treatment with HIV protease inhibitors was continued or started again. A causal relationship or mechanism of action between treatment with HIV protease inhibitors and the events mentioned has not been established.
Pr interval prolongation
Moderate asymptomatic PR interval prolongation has been reported in some patients on lopinavir/ritonavir. Grade II and III AV blockade has rarely been reported while taking lopinavir/ritonavir in patients with organic heart disease and preexisting conduction system disorders or in patients taking drugs that prolong the PR interval (such as verapamil or atazanavir). In these patients, lopinavir/ritonavir should be used with caution.
The electrocardiogram
The QTcF interval (corrected by Fridericia) was evaluated in a randomized, placebo-controlled crossover study with an active control (moxifloxacin 400 mg once daily) involving 39 healthy adult volunteers. Ten measurements were taken over 12 hours on day 3 of the study. The mean maximum difference in QTcF compared with placebo was 3.6 (6.3) ms and 13.1 (15.8) ms for the 400/100 mg 2 times/day and 800/200 mg 2 times/day doses of lopinavir/ritonavir, respectively. The changes observed with the above two regimens were approximately 1.5 and 3 times higher than those observed with the recommended doses of lopinavir/ritonavir 1 time/day or 2 times/day in equilibrium. No patients reported an increase in the QTcF > 60 ms interval from baseline; the QTcF interval did not exceed a potentially clinically meaningful threshold of 500 ms.
In the same study, patients taking lopinavir/ritonavir also showed a moderate increase in the PR interval on day 3. The maximum PR interval was 286 ms and no development of grade II or III atrial-ventricular block was observed.
The redistribution of adipose tissue
. Redistribution/accumulation of fat, including central obesity, increased fat deposition in the dorsocervical region (“bull hump”), peripheral wasting (decreased fat in the extremities), facial wasting, chest enlargement, and “cushingoid appearance,” have been observed in patients receiving antiretroviral therapy. The mechanism and long-term effects of these effects are currently unknown. A causal relationship has not been established.
Elevated lipid concentrations
Lopinavir/ritonavir treatment may increase cholesterol and triglyceride concentrations. Triglyceride and cholesterol concentrations should be tested before starting lopinavir/ritonavir and periodically during treatment. Appropriate treatment of lipid metabolism disorders should be given if necessary.
Contraindications
Contraindications
concomitant use with drugs whose clearance is significantly dependent on CYP3A-mediated metabolism, including astemizole, blonanserin, terfenadine, midazolam, triazolam, cisapride, pimozide, rifampicin, salmeterol, sildenafil (only if treated for pulmonary hypertension) vardenafil, voriconazole, ergot alkaloids (e.g. ergotamine and dihydroergotamine, ergometrine and methylergometrine), GmG-CoA reductase inhibitors (lovastatin, simvastatin), St John’s wort preparations, fosamprenavir;
1 use daily in combination with carbamazepine, phenobarbital or phenytoin; severe hepatic impairment;
Children under 3 years of age (children 6 months to 3 years of age are prescribed the drug in the oral dosage form);
hypersensitivity to lopinavir, ritonavir or to the excipients of the drug.
The drug should be used with caution in viral hepatitis B and C; cirrhosis of the liver;
mild to moderate hepatic impairment;
increased activity of liver enzymes; pancreatitis;
Hemophilia A and B; dyslipidemia (incl.Ñ. hypercholesterolemia, hypertriglyceridemia);
in elderly patients (over 65 years);
in patients with organic heart disease and pre-existing cardiac conduction abnormalities or in patients receiving drugs that prolong the PR interval (such as verapamil or atazanavir);
concomitantly with drugs for the treatment of erectile dysfunction (sildenafil, tadalafil);
concomitantly with fentanyl, rosuvastatin, atorvastatin, bupropion, with GCS for inhaled and intranasal use.
Side effects
Side effects
Children The profile of adverse events in children was similar to that in adults. The most frequently observed were perversion of taste, vomiting, diarrhea, and rash.
Digestive system disorders: constipation, pancreatitis, and hepatomegaly were common.
Hematopoietic system: often – increase of ACTV, decreased hemoglobin, decreased number of platelets, neutrophils. Dermatological reactions: often – dry skin.
Laboratory: often – increased sodium, potassium, calcium, increased bilirubin, increased ALT, AST, increased total cholesterol, increased amylase activity, increased uric acid, decreased sodium, potassium or calcium.
Others: often – viral infections, fever. Cases of toxic epidermal necrolysis, hepatitis, Stevens-Johnson syndrome, erythema multiforme and bradyarrhythmia have also been reported with lopinavir/ritonavir.
Adult patients
The most frequent side effect associated with lopinavir/ritonavir administration was mild to moderate diarrhea.
Possible causal side effects of the drug, both clinical and laboratory, are listed below by frequency: very common (â¥1/10), common (â¥1/100, but
Immune system disorders: infrequent hypersensitivity reactions; rare, immune reconstitution syndrome.
Digestive system disorders: very often – diarrhea; often – abdominal pain, flatulence, nausea, vomiting, irregular stools; infrequent – dyspepsia, abdominal discomfort, dry mouth, hemorrhagic enterocolitis, stool incontinence, gastritis, gastroesophageal reflux, pancreatitis, hepatitis; Rarely – dysphagia, lower abdominal pain, constipation, duodenitis, enterocolitis, enteritis, belching, esophagitis, stomach ulcers, hemorrhoids, mouth ulcers, periodontitis, rectal bleeding, stomatitis, hepatomegaly, cholecystitis, jaundice, steatosis of liver and liver pain; less than 2% – cholangitis.
Nervous system disorders: frequent – headache; infrequent – insomnia, paresthesia, decreased libido, depression, sleep disturbance, anxiety, nervousness, dizziness, peripheral neuropathy, somnolence, perversion of taste; Rarely, agitation, confusion, emotional lability, disorientation, thought disorders, amnesia, ataxia, dyskinesia, encephalopathy, extrapyramidal syndrome, facial nerve paresis, muscle tone, migraine, neuropathy, loss of taste and tremor; less than 2%, apathy, cerebral infarction and seizures.
Cardiovascular system disorders: infrequent – vascular disorders; rarely – increased BP, angina pectoris, AV blockade, myocardial infarction, palpitations, tricuspid valve failure, deep vein thrombosis, thrombophlebitis, varicose veins and vasculitis; less than 2% – atrial fibrillation, orthostatic hypotension.
Dermatological reactions: frequent – lipodystrophy; infrequent – rash, acne, alopecia, allergic dermatitis, maculopapular rash, itching and hyperhidrosis; rare – dry skin, eczema, idiopathic capillaritis, exfoliative dermatitis, facial edema, nail structure disorders, seborrhea, skin color changes, stretch marks, skin ulcers; less than 2% – skin hypertrophy.
Muscular system: infrequent – myalgia, arthralgia; rare – osteoarthritis, low back pain and bone necrosis, joint disease; less than 2% – muscle weakness.
Metabolism disorders: infrequent – dehydration, obesity, anorexia, weight loss or gain; rarely – decreased or increased appetite, hyperamylazemia, hyperlipazemia, hyperuricemia, hypophosphatemia, hypocholesterolemia, hypovitaminosis and hypothyroidism, lactacidosis, lipomatosis.
Endocrine system disorders: infrequent – diabetes mellitus, Icenko-Cushing’s syndrome; rare – male hypogonadism.
As to the urinary system: rarely – hematuria, nephrolithiasis, nephritis and abnormal laboratory values of urine, changes in urine odor.
Reproductive system disorders: infrequent – erectile dysfunction; rare: amenorrhea, ejaculation disorder, breast enlargement, gynecomastia, menorrhagia.
Respiratory system: infrequent – bronchitis; rare – cough, dyspnea, pulmonary edema; less than 2% – bronchospasm.
Hematopoietic system: rarely – anemia, leukopenia and lymphadenopathy.
Sensory system disorders: infrequent – tinnitus; rare – visual disturbances, hyperacusis, dizziness, balance disorders.
Infections: rarely – bacterial infection, bronchopneumonia, inflammation of subcutaneous fatty tissue, folliculitis, furunculosis, gastroenteritis, otitis media, perineal abscess, pharyngitis, rhinitis, sialoadenitis, sinusitis and viral infection (including flu). Novelties: rarely – neoplasms (including benign skin neoplasms), cysts.
General: frequently – asthenia; infrequently – pain, pain in the sternum, fever, edema, malaise; rarely – chills, peripheral edema, chest pain, splenomegaly.
Laboratory findings: very common – increased concentration of total cholesterol, triglycerides; increased GGT activity; common – increased concentration of glucose, abnormal liver tests, increased activity of serum ACT, ALT, amylase; infrequent – increased concentration of total bilirubin, abnormal in tests to determine the concentration of hormones and other laboratory tests, increased lipase activity, decreased IQ, decreased glucose tolerance, rare – neutropenia, increased ALP activity, less than 2% – increased uric acid concentration, increased CPK activity, decreased concentrations of inorganic phosphorus, hemoglobin.
Overdose
Overdose
Clinical experience with acute lopinavir/ritonavir overdose in humans is limited.
Treatment. There is no specific antidote. Measures are taken to maintain the body’s life support, including monitoring of vital systems and monitoring the patient’s clinical condition.
If necessary, the unabsorbed drug is removed by gastric lavage and activated charcoal is prescribed. Because lopinavir/ritonavir is highly bound to plasma proteins, the use of dialysis is not appropriate.
Pregnancy use
Pregnancy use
Prenatal use of the drug is possible only when the estimated benefit to the mother outweighs the potential risk to the fetus.
If it is necessary to use the drug during lactation, breastfeeding should be stopped.
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | The drug should be kept out of reach of children at 15 ° to 30 ° C. |
| Manufacturer | AbbWee Deutschland GmbH/Ortat, Russia |
| Medication form | pills |
| Brand | AbbWee Deutschland GmbH/Ortat |
Related products
Buy Kaletra, 200 mg+50 mg 120 pcs with delivery to USA, UK, Europe and over 120 other countries.