No products in the cart.
Kalchek, tablets 10 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacodynamics
Amlodipine is a dihydropyridine derivative. Binding to dihydropyridine receptors, it blocks “slow” calcium channels, inhibits transmembrane calcium transfer in heart and vascular smooth muscle cells (more in vascular smooth muscle cells than in cardiomyocytes). It has hypotensive and antianginal effect.
The mechanism of hypotensive action of amlodipine is due to a direct relaxing effect on vascular smooth muscle.
Amlodipine reduces myocardial ischemia in the following two ways:
1. Dilates the arterioles and thus reduces total peripheral resistance (post-load) while keeping heart rate virtually unchanged, resulting in lower energy consumption and myocardial oxygen demand.
2. dilates coronary and peripheral arteries and arterioles in both normal and ischemic areas of the myocardium, which increases the flow of oxygen to the myocardium in patients with vasospastic angina (Prinzmetal angina) and prevents the development of coronarospasm caused by smoking.
In patients with arterial hypertension, a single daily dose of Kalchek provides reduction of blood pressure (BP) for 24 hours (both “lying” and “standing”). Because of the slow onset of action, amlodipine does not cause a sharp decrease in BP.
In patients with angina a single daily dose of the drug increases exercise time, delays onset of angina attack and ST-segment depression (by 1 mm) with exercise, decreases angina attacks frequency and nitroglycerin consumption.
The use in patients with coronary heart disease (CHD)
In patients with cardiovascular disease (including coronary atherosclerosis with lesion of one vessel and up to stenosis of 3 or more arteries and atherosclerosis of carotid arteries), who have had myocardial infarction, percutaneous transluminal angioplasty of coronary arteries (TPA) or suffering from angina pectoris, the use of Kalchek prevents the development of carotid artery intima-media thickening, stroke, THA, aortocoronary bypass surgery, results in fewer hospitalizations for unstable angina and progression of chronic heart failure (CHF), and reduces the frequency of interventions aimed at restoring coronary flow.
The use in patients with heart failure
Kalchek does not increase the risk of death or development of complications and fatal outcomes in patients with chronic heart failure (CHF) of functional class III-IV (according to NYHA) on the background of therapy with digoxin, diuretics and ACE inhibitors. In patients with CHF of III-IV functional class according to NYHA of non-ischemic etiology, there is a possibility of pulmonary edema when using Kalchek. Kalchek has no adverse effect on metabolism and blood plasma lipid concentration.
Pharmacokinetics
After oral administration, amlodipine is slowly absorbed (about 90%) from the gastrointestinal tract. Absolute bioavailability is 64-80%, the maximum concentration in blood serum is observed after 6-9 hours. Equilibrium concentrations are reached after 7-8 days of therapy. Food intake has no effect on absorption of amlodipine. The average volume of distribution is 21 l/kg body weight, indicating that most of the drug is in the tissues and a relatively smaller part of it is in the blood.
Most of the drug that is in the blood (97%) is bound to plasma proteins.
Amlodipine is metabolized in the liver to form inactive metabolites.
After a single oral dose the elimination half-life (T1/2) is on average 35 hours. About 60% of the dose taken orally is excreted by the kidneys mainly as metabolites, 10% – unchanged, and 20-25% – with the bile through the intestine.
In patients with arterial hypertension T1/2 is 48 hours, in elderly patients (over 65 years) excretion of amlodipine is delayed (T1/2 is 65 h) compared to younger patients, but this limit is not clinically relevant.
In patients with hepatic impairment, a prolongation of T1/2 is expected, and cumulation of the drug in the body will be higher with long-term administration (T1/2 up to 60 h).
Renal insufficiency has no significant effect on the kinetics of amlodipine.
The drug penetrates the blood-brain barrier. It is not eliminated by hemodialysis.
Indications
Indications
Arterial hypertension (in monotherapy or in combination with other antihypertensive drugs);
stable angina pectoris, vasospastic angina (Prinzmetal angina) (in monotherapy or in combination with other antianginal drugs).
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Amlodipine is a dihydropyridine derivative. By binding to dihydropyridine receptors, it blocks “slow” calcium channels, inhibits the transmembrane transition of calcium into the smooth muscle cells of the heart and blood vessels (to a greater extent into vascular smooth muscle cells than into cardiomyocytes). It has a hypotensive and antianginal effect.
The mechanism of the hypotensive effect of amlodipine is due to a direct relaxing effect on vascular smooth muscle.
Amlodipine reduces myocardial ischemia in the following two ways:
1. Dilates the arterioles and, thus, reduces the total peripheral resistance (afterload), while the heart rate remains virtually unchanged, which leads to a decrease in energy consumption and myocardial oxygen demand.
2. Expands coronary and peripheral arteries and arterioles in both normal and ischemic areas of the myocardium, which increases the supply of oxygen to the myocardium in patients with vasospastic angina (Prinzmetal angina) and prevents the development of coronary spasm caused by smoking.
In patients with arterial hypertension, a single daily dose of Kalchek provides a decrease in blood pressure (BP) for 24 hours (both in the “lying” and “standing” positions). Due to its slow onset of action, amlodipine does not cause a sharp decrease in blood pressure.
In patients with angina pectoris, a single daily dose of the drug increases the time of physical activity, delays the development of the next attack of angina and ST segment depression (by 1 mm) during physical activity, reduces the frequency of angina attacks and the consumption of nitroglycerin.
Use in patients with coronary heart disease (CHD)
In patients with cardiovascular diseases (including coronary atherosclerosis with damage to one vessel and up to stenosis of 3 or more arteries and atherosclerosis of the carotid arteries), who have had myocardial infarction, percutaneous transluminal angioplasty of the coronary arteries (PCA) or suffering from angina, the use of Kalchek prevents the development of thickening of the intima-media of the carotid arteries, stroke, TLP, coronary artery bypass grafting, leads to a reduction in the number of hospitalizations for unstable angina and progression of chronic heart failure (CHF), and reduces the frequency of interventions aimed at restoring coronary flow.
Use in patients with heart failure
Kalchek does not increase the risk of death or the development of complications and deaths in patients with chronic heart failure (CHF) functional class III–IV (according to NYHA) during therapy with digoxin, diuretics and ACE inhibitors. In patients with CHF of functional class III–IV according to TNRF of non-ischemic etiology, when using Kalchek, there is a possibility of pulmonary edema. Kalchek does not have any adverse effects on metabolism and plasma lipid concentrations.
Pharmacokinetics
After oral administration, amlodipine is slowly absorbed (about 90%) from the gastrointestinal tract. Absolute bioavailability is 64–80%, maximum serum concentration is observed after 6–9 hours. Equilibrium concentrations are achieved after 7–8 days of drug therapy. Food intake does not affect the absorption of amlodipine. The average volume of distribution is 21 l/kg body weight, which indicates that most of the drug is in the tissues, and a relatively smaller part is in the blood.
Most of the drug in the blood (97%) binds to blood plasma proteins.
Amlodipine is metabolized in the liver to form inactive metabolites.
After a single oral dose, the half-life (T1/2) averages 35 hours. About 60% of the dose taken orally is excreted by the kidneys mainly in the form of metabolites, 10% unchanged, and 20–25% with bile through the intestines.
In patients with arterial hypertension, T1/2 is 48 hours; in elderly patients (over 65 years of age), the elimination of amlodipine is slowed down (T1/2 is 65 hours) compared to young patients, but this limit is not clinically significant.
In patients with liver failure, a prolongation of T1/2 is expected, and with long-term administration, the accumulation of the drug in the body will be higher (T1/2 up to 60 hours).
Renal failure does not significantly affect the kinetics of amlodipine.
The drug penetrates the blood-brain barrier. It is not removed by hemodialysis.
Special instructions
Special instructions
During the treatment period, it is necessary to monitor body weight and sodium intake, and prescribe an appropriate diet.
It is necessary to maintain dental hygiene and frequent visits to the dentist (to prevent soreness, bleeding and gum hyperplasia).
The dosage regimen for elderly patients is the same as for patients of other age groups. When increasing the dose, careful monitoring of elderly patients is necessary.
Despite the absence of withdrawal syndrome in BMCC, a gradual dose reduction is recommended before stopping treatment.
Amlodipine does not affect plasma concentrations of potassium ions, glucose, triglycerides, total cholesterol, low-density lipoproteins, uric acid, creatinine and uric acid nitrogen.
Patients with low body weight, patients of short stature and patients with severe liver dysfunction may require a lower dosage.
The effectiveness and safety of the use of the drug Kalchek in hypertensive crisis has not been established.
Impact on the ability to drive vehicles and machinery
During the treatment period, caution should be exercised when driving vehicles and engaging in other activities that require concentration and speed of psychomotor reactions, due to the possibility of dizziness and drowsiness.
Active ingredient
Active ingredient
Amlodipine
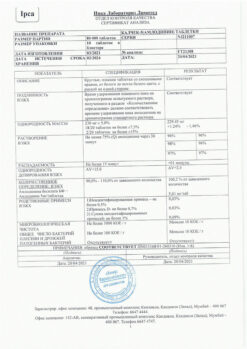
Composition
Composition
1 tablet contains:
active ingredient:
amlodipine besylate, which is equivalent to amlodipine 10 mg.
excipients:
corn starch,
calcium hydrogen phosphate,
talc,
colloidal silicon dioxide,
sodium carboxymethyl starch,
magnesium stearate.
Pregnancy
Pregnancy
The safety of amlodipine during pregnancy has not been established; therefore, use during pregnancy is possible only when the benefit to the mother outweighs the risk to the fetus.
There is no data indicating the excretion of amlodipine in breast milk.
However, it is known that other BMCCs, dihydropyridine derivatives, are excreted in breast milk. If it is necessary to prescribe amlodipine during lactation, the issue of stopping breastfeeding should be decided.
Contraindications
Contraindications
hypersensitivity to amlodnpine and/or other components of the drug Kalchek, as well as to other dihydropyridine derivatives;
severe arterial hypotension (systolic blood pressure less than 90 mmHg);
unstable angina (with the exception of Prinzmetal’s angina);
severe stenosis of the aortic mouth;
age under 18 years (efficacy and safety have not been established).
With caution: impaired liver function, sick sinus syndrome (severe bradycardia, tachycardia), chronic heart failure of non-ischemic etiology (III-IV functional class according to the NYHA classification), arterial hypotension, aortic stenosis, mitral stenosis, hypertrophic obstructive cardiomyopathy, acute myocardial infarction (and within 1 month after), old age.
Side Effects
Side Effects
From the cardiovascular system: palpitations, marked decrease in blood pressure, peripheral edema (swelling of the ankles and feet), rarely – heart rhythm disturbances (bradycardia, ventricular tachycardia, atrial flutter), myocardial infarction, chest pain, orthostatic hypotension, vasculitis, very rarely – development or worsening of heart failure, extrasystole, migraine.
From the central nervous system: headache, dizziness, increased fatigue, feeling of heat and “flushes” of blood to the skin of the face, drowsiness, mood changes, convulsions, rarely – loss of consciousness, hypoesthesia, nervousness, paresthesia, peripheral neuropathy, tremor, vertigo, asthenia, malaise, fainting, insomnia, emotional lability, depression, anxiety, unusual dreams, very rarely – ataxia, apathy, agitation, amnesia.
From the digestive system: nausea, vomiting, epigastric pain, rarely – increased activity of liver transaminases, hyperbilirubinemia, jaundice (due to cholestasis), pancreatitis, dry oral mucosa, thirst, hepatitis, flatulence, gum hyperplasia, constipation, diarrhea, anorexia, very rarely – gastritis, increased appetite.
From the hematopoietic organs: very rarely – thrombocytopenic purpura, leukopenia, thrombocytopenia.
From the respiratory system: shortness of breath, rhinitis, very rarely – cough.
From the genitourinary system: rarely – pollakiuria, painful urge to urinate, nocturia, sexual dysfunction (including decreased potency); very rarely – dysuria, polyuria.
From the skin: very rarely – xeroderma, dermatitis, purpura, skin pigmentation disorder.
Allergic reactions: skin itching, rash (including erythematous, maculopapular rash, urticaria), angioedema, erythema multiforme.
From the musculoskeletal system: rarely – arthralgia, muscle cramps, arthrosis, back pain, myalgia (with long-term use); very rarely – myasthenia.
Other: rarely – gynecomastia, gyneruricemia, weight gain/loss, hyperglycemia, blurred vision, diplopia, conjunctivitis, eye pain, tinnitus, dyspnea, nosebleeds, increased sweating; very rarely – cold sticky sweat, parosmia, impaired taste, impaired accommodation, xerophthalmia.
Interaction
Interaction
It can be expected that inhibitors of microsomal liver enzymes will increase the concentration of amlodipine in the blood plasma, increasing the risk of side effects, and inducers of microsomal liver enzymes will reduce it.
Unlike other BMCCs, there is no clinically significant interaction with non-steroidal anti-inflammatory drugs, especially with indomethacin.
Thiazide and loop diuretics, beta-blockers, verapamil, ACE inhibitors and nitrates enhance the antianginal and hypotensive effect of amlodipine.
Amiodarone, quinidine, inhalation anesthetics (hydrocarbon derivatives), alpha1-blockers, antipsychotics (neuroleptics) and BMCC may enhance the hypotensive effect.
Amlodipine does not affect the pharmacokinetic parameters of digoxin and warfarin.
Cimetidine: with simultaneous use of amlodipine with cimetidine, the pharmacokinetics of amlodipine does not change.
When amlodipine is used together with lithium preparations, it is possible to increase the manifestations of their neurotoxicity (nausea, vomiting, diarrhea, ataxia, tremor, tinnitus).
Calcium supplements can reduce the effect of BMCC.
Antiviral agents (ritonavir) increase plasma concentrations of BMCC, including amlodipine.
Isoflurane – enhances the hypotensive effect of dihydropyridine derivatives.
When BMCC is used together with lithium preparations, increased neurotoxicity is possible.
Repeated use of amlodipine at a dose of 10 mg and atorvastatin at a dose of 80 mg is not accompanied by significant changes in the pharmacokinetics of atorvastatin.
Simultaneous administration of 240 ml of grapefruit juice and 10 mg of amlodipine is not accompanied by significant changes in the pharmacokinetics of amlodipine.
Simultaneous administration of 100 mg of sildenafil in patients with essential hypertension does not affect the pharmacokinetic parameters of amlodipine.
Overdose
Overdose
Symptoms: marked decrease in blood pressure, tachycardia, excessive peripheral vasodilation (risk of developing severe and persistent arterial hypotension, including the development of shock).
Treatment: gastric lavage, administration of activated charcoal (especially in the first 2 hours after an overdose), maintaining the function of the cardiovascular system, monitoring indicators of heart and lung function, elevated position of the extremities, monitoring the volume of circulating blood and diuresis. To restore vascular tone, use vasoconstrictors (in the absence of contraindications to their use); to eliminate the effects of blockade of calcium channels – intravenous administration of calcium gluconate. Hemodialysis is ineffective.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Ipka Laboratories Limited, India
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Ipka Laboratories Limited, India |
| Medication form | pills |
| Brand | Ipka Laboratories Limited |
Other forms…
Related products
Buy Kalchek, tablets 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.