No products in the cart.
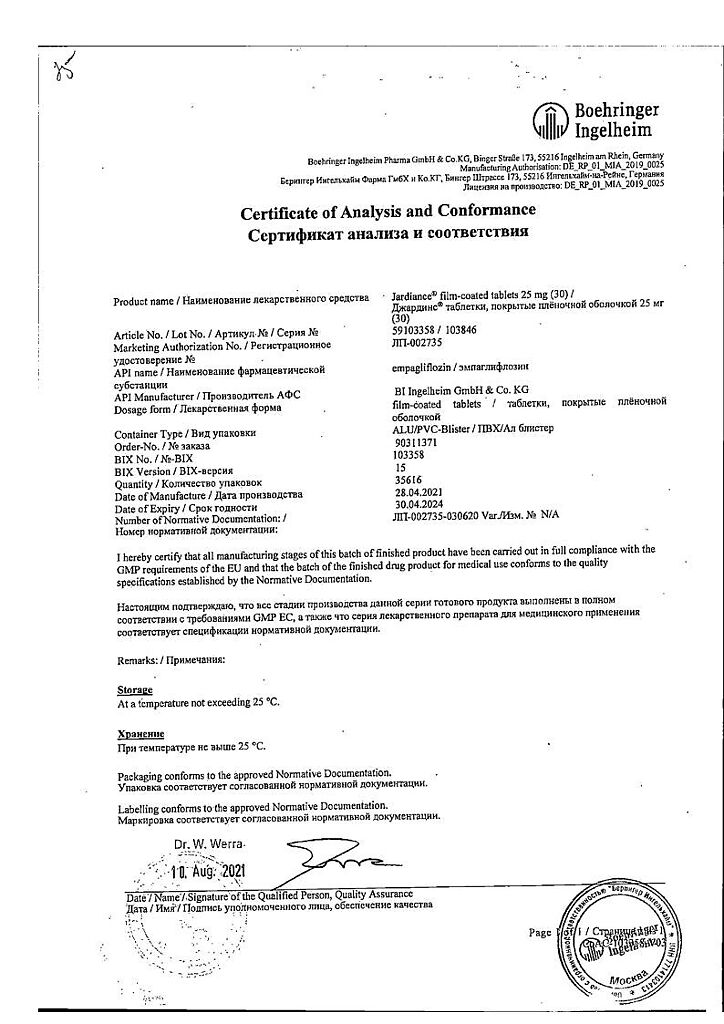
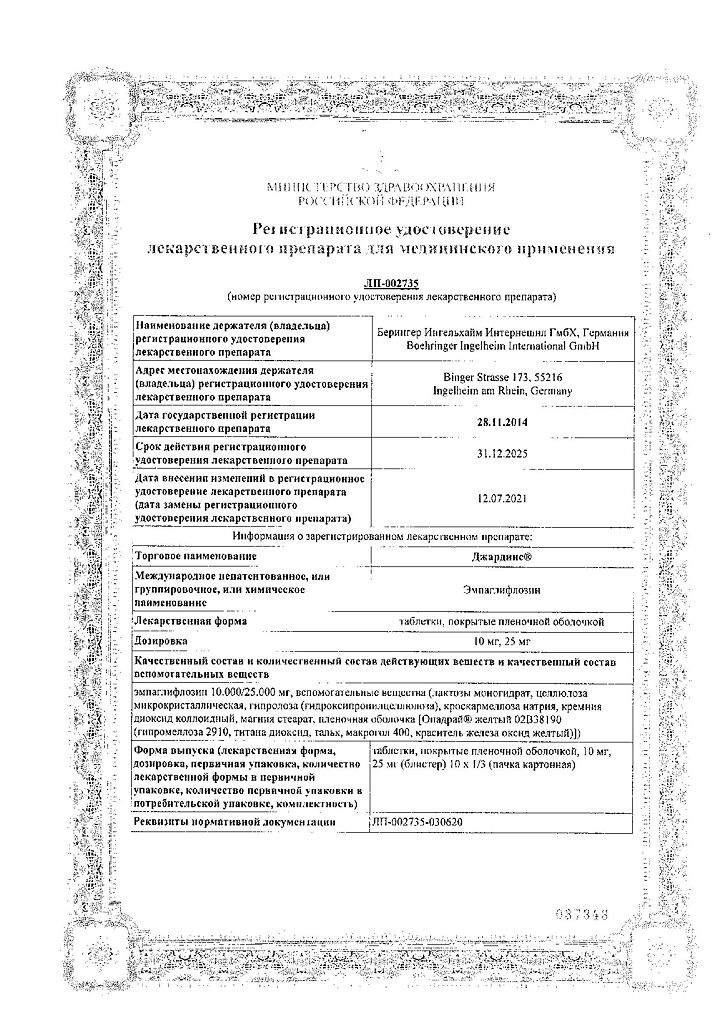
Jardins, 25 mg 30 pcs.
€79.87 €66.56
Description
Empagliflozin is a reversible, highly active, selective and competitive inhibitor of the type 2 sodium-dependent glucose transporter with a concentration required to inhibit 50% of the enzyme activity (IC50) equal to 1.3 nmol. The selectivity of empagliflozin to the sodium-dependent glucose transporter type 2 is 5000 times greater than the selectivity to the sodium-dependent glucose transporter type 1, responsible for glucose absorption in the intestine.
Empagliflozin was also found to be highly selective against other glucose transporters responsible for glucose homeostasis in various tissues.
The sodium-dependent glucose transporter type 2 is the main glucose transporter protein responsible for reabsorption of glucose from the renal glomeruli back into the bloodstream.
Empagliflozin improves glycemic control in patients with type 2 diabetes mellitus (T2DM) by reducing glucose reabsorption in the kidneys. The amount of glucose excreted by the kidneys through this mechanism depends on blood glucose concentration and GFR. Inhibition of the type 2 sodium-dependent glucose transporter in patients with DM 2 and hyperglycemia results in excretion of excess glucose by the kidneys.
In a 4-week clinical trial, it was found that in patients with DM 2, renal glucose excretion increased immediately after the first dose of empagliflozin; this effect lasted for 24 hours. Increased renal glucose excretion persisted until the end of treatment, averaging approximately 78 g/day when empagliflozin was administered at a dose of 25 mg once daily. In patients with DM 2, increased renal excretion of glucose led to an immediate decrease in plasma glucose concentrations.
Empagliflozin (10 mg and 25 mg doses) decreases plasma glucose concentrations both when taken on an empty stomach and after meals.
The mechanism of action of empagliflozin does not depend on the functional state of pancreatic β-cells and insulin metabolism, which promotes low risk of possible hypoglycemia. A positive effect of empagliflozin on surrogate markers of β-cell function, including the NOMA-β index (homeostasis-β assessment model) and the proinsulin/insulin ratio, has been noted. In addition, additional glucose excretion by the kidneys causes caloric loss, which is accompanied by a decrease in adipose tissue volume and body weight.
Glucosuria seen during empagliflozin administration is accompanied by a slight increase in diuresis, which may contribute to a moderate decrease in BP.
In clinical trials using empagliflozin as monotherapy; combination therapy with metformin; combination therapy with metformin in patients with newly diagnosed DM2; combination therapy with metformin and sulfonylurea derivatives; combination therapy with pioglitazone ± metformin; combination therapy with linagliptin in patients with newly diagnosed DMD 2; combination therapy with linagliptin added to metformin therapy; combination therapy with linagliptin compared to placebo in patients with inadequate glycemic control on linagliptin and metformin; combination therapy with metformin versus glimepiride (data from a 2-year study); combination therapy with insulin (multiple insulin injection regimen) ± metformin; combination therapy with basal insulin; combination therapy with dipeptidyl peptidase-4 (DPP-4) inhibitor, metformin ± another hypoglycemic oral medication was shown to statistically significantly reduce glycosylated hemoglobin (HbA1c), decrease fasting plasma glucose concentration, and decrease BP and body weight.
The clinical trial investigated the effect of JARDINS® on the incidence of cardiovascular events in patients with DM2 and high cardiovascular risk (defined as having at least one of the following diseases and/or conditions CHD (history of myocardial infarction, coronary artery bypass grafting, CHD with a single coronary vessel lesion, CHD with multiple coronary vessels lesions), history of ischemic or hemorrhagic stroke, peripheral artery disease with or without symptoms) receiving standard therapy that included hypoglycemic drugs and medications for cardiovascular disease. Cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke were assessed as the primary endpoint. Additional pre-specified end points were cardiovascular death, overall mortality, development of nephropathy or progressive worsening of nephropathy, and hospitalization for heart failure.
Empagliflozin improved overall survival by reducing cardiovascular death and reduced the risk of hospitalization for heart failure. JARDINS® was also shown in a clinical trial to reduce the risk of nephropathy or progressive worsening of nephropathy.
In patients with baseline macroalbuminuria, JARDINS® was found to result in sustained normo- or microalbuminuria significantly more often than placebo (hazard ratio 1.82 [95% CI 1.40; 2.37]).
Indications
Indications
Diabetes mellitus type 2:
as monotherapy in patients with inadequate glycemic control only on the background of diet and exercise, the administration of metformin to whom is considered inappropriate due to intolerance;
as a combination therapy with other hypoglycemic agents, including insulin, when the therapy used together with diet and exercise does not provide the necessary glycemic control.
Pharmacological effect
Pharmacological effect
Empagliflozin is a reversible, highly active, selective and competitive inhibitor of sodium glucose transporter type 2 with a concentration required to inhibit 50% of enzyme activity (IC50) of 1.3 nmol. The selectivity of empagliflozin for sodium-dependent glucose transporter type 2 is 5000 times greater than the selectivity for sodium-dependent glucose transporter type 1, which is responsible for the absorption of glucose in the intestine.
In addition, empagliflozin was found to be highly selective for other glucose transporters responsible for glucose homeostasis in various tissues.
Sodium-dependent glucose transporter type 2 is the primary transport protein responsible for the reabsorption of glucose from the glomeruli back into the bloodstream.
Empagliflozin improves glycemic control in patients with type 2 diabetes mellitus (T2DM) by reducing renal glucose reabsorption. The amount of glucose excreted by the kidneys through this mechanism depends on the blood glucose concentration and GFR. Inhibition of sodium-dependent glucose transporter type 2 in patients with type 2 diabetes and hyperglycemia leads to the excretion of excess glucose by the kidneys.
A 4-week clinical study found that in patients with type 2 diabetes, renal glucose excretion increased immediately after the first dose of empagliflozin; this effect lasted for 24 hours. The increase in glucose excretion by the kidneys persisted until the end of treatment, amounting to an average of about 78 g/day when using empagliflozin at a dose of 25 mg 1 time/day. In patients with type 2 diabetes, an increase in renal glucose excretion led to an immediate decrease in plasma glucose concentrations.
Empagliflozin (at a dose of 10 mg and 25 mg) reduces the concentration of glucose in the blood plasma both when taken on an empty stomach and after a meal.
The mechanism of action of empagliflozin does not depend on the functional state of pancreatic β-cells and insulin metabolism, which contributes to a low risk of the possible development of hypoglycemia. Positive effects of empagliflozin on surrogate markers of β-cell function, including the HOMA-β (Homeostasis Model Assessment-β) index and proinsulin-to-insulin ratio, were observed. In addition, additional excretion of glucose by the kidneys causes a loss of calories, which is accompanied by a decrease in the volume of adipose tissue and a decrease in body weight.
Glucosuria observed during the use of empagliflozin is accompanied by a slight increase in diuresis, which may contribute to a moderate decrease in blood pressure.
In clinical studies using empagliflozin as monotherapy; combination therapy with metformin; combination therapy with metformin in patients with newly diagnosed type 2 diabetes; combination therapy with metformin and sulfonylurea derivatives; combination therapy with pioglitazone ± metformin; combination therapy with linagliptin in patients with newly diagnosed type 2 diabetes; combination therapy with linagliptin added to metformin therapy; combination therapy with linagliptin compared with placebo in patients with inadequate glycemic control while taking linagliptin and metformin; combination therapy with metformin compared with glimepiride (data from a 2-year study); combination therapy with insulin (regimen of multiple insulin injections) ± metformin; combination therapy with basal insulin; Combination therapy with a dipeptidyl peptidase-4 (DPP-4) inhibitor, metformin ± another hypoglycemic oral drug showed a statistically significant decrease in glycosylated hemoglobin (HbA1c), a decrease in fasting plasma glucose concentration, as well as a decrease in blood pressure and body weight.
A clinical trial examined the effect of JARDINS® on the incidence of cardiovascular events in patients with type 2 diabetes and high cardiovascular risk (defined as the presence of at least one of the following diseases and/or conditions: coronary artery disease (history of myocardial infarction, coronary artery bypass grafting, single coronary artery disease, multiple coronary artery disease), ischemic or hemorrhagic stroke history of peripheral arterial disease with or without symptoms) receiving standard therapy, which included hypoglycemic drugs and drugs for the treatment of cardiovascular diseases. The primary endpoint was cardiovascular death, non-fatal myocardial infarction and non-fatal stroke. Additional prespecified endpoints included cardiovascular death, all-cause mortality, development of nephropathy or progressive worsening of nephropathy, and hospitalization for heart failure.
Empagliflozin improved overall survival by reducing cardiovascular death and reducing the risk of hospitalization for heart failure. JARDINS® was also shown to reduce the risk of nephropathy or progressive worsening of nephropathy in a clinical trial.
In patients with baseline macroalbuminuria, it was found that JARDINS® resulted in sustained normo- or microalbuminuria significantly more often than placebo (risk ratio 1.82 [95% CI 1.40; 2.37]).
Special instructions
Special instructions
Jardins is not recommended for use in patients with type 1 diabetes mellitus or for the treatment of diabetic ketoacidosis.
The maximum daily dose of Jardins contains 113 mg of lactose, so the drug should not be used in patients with rare hereditary disorders such as lactase deficiency, lactose intolerance, and glucose-galactose malabsorption.
Clinical studies have shown that treatment with empagliflozin does not increase cardiovascular risk. The use of empagliflozin at a dose of 25 mg does not prolong the QT interval.
When using Jardins concomitantly with sulfonylureas or insulin, a reduction in the dose of sulfonylureas/insulin may be required due to the risk of hypoglycemia.
Combinations of hypoglycemic drugs that have not been studied
Empagliflozin has not been studied in combination with glucagon-like peptide 1 (GLP-1) analogues.
Monitoring kidney function
The effectiveness of Jardines depends on kidney function. Therefore, it is recommended to monitor renal function before prescribing it and periodically during treatment (at least once a year), as well as before prescribing concomitant therapy that may adversely affect renal function. For patients with renal failure (GFR less than 45 ml/min), the drug is not recommended.
Elderly patients
Patients aged 75 years or older have an increased risk of dehydration. These patients receiving empagliflozin were more likely to experience adverse reactions due to hypovolemia (compared to patients receiving placebo). Experience with empagliflozin in patients over 85 years of age is limited, and therefore it is not recommended to prescribe Jardins to patients over 85 years of age.
Use in patients at risk of developing hypovolemia
According to the mechanism of action, taking the drug Jardins can lead to a moderate decrease in blood pressure. Therefore, the drug should be used with caution in cases where a decrease in blood pressure is undesirable, for example, in patients with cardiovascular diseases; patients taking antihypertensive drugs (with a history of arterial hypotension), as well as in patients over 75 years of age.
If a patient taking Jardins develops conditions that may lead to fluid loss (for example, diseases of the gastrointestinal tract), the patient’s condition, blood pressure, and hematocrit and electrolyte balance should be carefully monitored. It may be necessary to temporarily stop taking the drug until water balance is restored.
Urinary tract infections
The incidence of side effects such as urinary tract infections was comparable with empagliflozin 25 mg and placebo, and higher with empagliflozin 10 mg. Complicated urinary tract infections (such as pyelonephritis and urosepsis) were reported at similar rates in patients treated with empagliflozin and placebo. If complicated urinary tract infections develop, temporary discontinuation of empagliflozin therapy is necessary.
Laboratory urine analysis
According to the mechanism of action, glucose is detected in the urine in patients taking Jardins.
Impact on the ability to drive vehicles and machinery
Clinical studies on the effect of empagliflozin on the ability to drive vehicles and operate machinery have not been conducted. Patients should be careful when driving vehicles and machinery, as hypoglycemia may develop when using Jardins (especially in combination with sulfonylurea derivatives and/or insulin).
Active ingredient
Active ingredient
Empagliflozin
Composition
Composition
1 tablet contains:
Active substance:
empagliflozin 25 mg;
Excipients:
lactose monohydrate,
microcrystalline cellulose,
hyprolose (hydroxypropylcellulose),
croscarmellose sodium,
colloidal silicon dioxide,
magnesium stearate.
Film shell composition:
opadry yellow (02B38190) (hypromellose 2910, titanium dioxide (E171), talc, macrogol 400, iron oxide yellow (E172)).
Contraindications
Contraindications
hypersensitivity to any component of the drug;
type 1 diabetes mellitus;
diabetic ketoacidosis;
rare hereditary disorders (lactase deficiency, lactose intolerance, glucose-galactose malabsorption);
renal failure with GFR < 45 ml/min per 1.73 m2 (due to ineffectiveness);
pregnancy and breastfeeding;
age over 85 years;
use in combination with glucagon-like peptide 1 analogues (due to the lack of data on efficacy and safety);
children under 18 years of age (due to insufficient data on effectiveness and safety).
With caution
patients at risk of developing hypovolemia (use of antihypertensive drugs with a history of arterial hypotension);
for gastrointestinal diseases leading to fluid loss;
age over 75 years;
use in combination with sulfonylurea derivatives or insulin;
infections of the genitourinary system.
Side Effects
Side Effects
The overall incidence of adverse events in patients receiving empagliflozin or placebo in clinical studies was similar. The most common adverse reaction was hypoglycemia, observed when empagliflozin was used in combination with sulfonylureas or insulin (see description of individual adverse reactions).
Adverse reactions observed in patients receiving empagliflozin in placebo-controlled studies are presented in the Table below (adverse reactions classified by organ system and according to MedDRA preferred terms) and their absolute frequency. Frequency categories are defined as follows: very common (≥1/10), common (≥1/100 to
Table. Side effects observed in placebo-controlled studies
Classification by organs and systems
Very frequent
Frequent
Infectious and parasitic diseases
Vaginal candidiasis, vulvovaginitis, balanitis and other genital infections
Urinary tract infections
Metabolic and nutritional disorders
Hypoglycemia (when used together with sulfonylureas or insulin)
Hypovolemia
Renal and urinary tract disorders
Frequent urination
Description of selected adverse reactions
Hypoglycemia
The incidence of hypoglycemia depended on the concomitant hypoglycemic therapy used.
Mild hypoglycemia (blood glucose 3.0 – 3.8 mmol/l (54-70 mg/dl))
The incidence of mild hypoglycemia was similar in patients receiving empagliflozin or placebo alone, when empagliflozin was added to metformin, and when empagliflozin was added to pioglitazone (± metformin). When empagliflozin was given in combination with metformin and a sulfonylurea, the incidence of hypoglycemia was higher (10 mg: 10.3%; 25 mg: 7.4%) than when placebo was prescribed in the same combination (5.3%).
Severe hypoglycemia (blood glucose below 3 mmol/L (54 mg/dL))
The incidence of severe hypoglycemia was similar in patients receiving empagliflozin and placebo alone. When empagliflozin was prescribed in combination with metformin and sulfonylureas, the incidence of hypoglycemia was higher (10 mg: 5.8%; 25 mg: 4.1%) than when placebo was prescribed in the same combination (3.1%).
Frequent urination
The incidence of urinary frequency (measured by symptoms such as pollakiuria, polyuria, nocturia) was higher with empagliflozin (10 mg dose: 3.4%, 25 mg dose: 3.2%) than with placebo (1%). The incidence of nocturia was comparable in the group of patients taking empagliflozin and in the group of patients taking placebo (less than 1%). The intensity of these side effects was mild to moderate.
Urinary tract infections
The incidence of urinary tract infections was similar between empagliflozin 25 mg and placebo (7.6%) but higher with empagliflozin 10 mg (9.3%). As with placebo, urinary tract infections with empagliflozin were more common in patients with a history of chronic or recurrent urinary tract infections. The incidence of urinary tract infections was similar between patients taking empagliflozin and placebo. Urinary tract infections were more common in women.
Genital infections
The incidence of adverse events such as vaginal candidiasis. vulvovaginitis, balanitis and other genital infections were higher with empagliflozin (10 mg dose: 4.1%, 25 mg dose: 3.7%) than with placebo (0.9%). Genital infections were more common in women. The intensity of genital infections was mild or moderate.
Hypovolemia
The incidence of hypovolemia (expressed as decreased blood pressure, orthostatic hypotension, dehydration, syncope) was similar between empagliflozin (10 mg dose: 0.5% and 25 mg dose: 0.3%) and placebo (0.3%). In patients over 75 years of age, the incidence of hypovolemia was comparable in patients taking empagliflozin 10 mg (2.3%) and placebo (2.1%), but higher in patients taking empagliflozin 25 mg (4.4%).
Interaction
Interaction
In vitro assessment of drug interactions
Empagliflozin does not inhibit, inactivate or induce CYP450 isoenzymes. The main pathway of metabolism of empagliflozin in humans is glucuronidation with the participation of uridine 5′-diphospho-glucuronosyltransferases UGT2B7, UGT1A3, UGT1A8 and UGT1A9. Empagliflozin does not inhibit UGT1A1. Drug interactions between empagliflozin and drugs that are substrates of the CYP450 and UGT1A1 isoenzymes are considered unlikely.
Empagliflozin is a substrate for P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP), but does not inhibit these proteins at therapeutic doses. Based on data obtained from in vitro studies, it is believed that the ability of empagliflozin to interact with drugs that are substrates of P-glycoprotein (P-gp). unlikely. Empagliflozin is a substrate for the organic anion transporters OAT3, OATP1B1 and OATP1B3, but is not a substrate for organic anion transporter 1 (OAT1) and organic cationic transporter 2 (OCT2). However, drug interactions between empagliflozin and drugs that are substrates for the transporter proteins described above are considered unlikely.
In vivo assessment of drug interactions
The pharmacokinetics of empagliflozin does not change in healthy volunteers when co-administered with metformin. glimepiride, pioglitazone, sitagliptin, linagliptin, warfarin, verapamil, ramipril, simvastatin, torsemide and hydrochlorothiazide. When empagliflozin was co-administered with gemfibrozil, rifampicin and probenecid, there was an increase in empagliflozin AUC by 59%, 35% and 53%, respectively, but these changes were not considered clinically significant.
Empagliflozin does not have a clinically significant effect on the pharmacokinetics of metformin, glimepiride, pioglitazone, sitagliptin, linagliptin, warfarin, digoxin, ramipril, simvastatin, hydrochlorothiazide, torsemide and oral contraceptives.
Diuretics
Empagliflozin may enhance the diuretic effect of thiazide and loop diuretics, which in turn may increase the risk of dehydration and arterial hypotension.
Insulin and drugs that enhance its secretion
Insulin and drugs that increase insulin secretion, such as sulfonylureas, may increase the risk of hypoglycemia. Therefore, when using empagliflozin simultaneously with insulin and drugs that enhance its secretion, it may be necessary to reduce their dose to avoid the risk of hypoglycemia.
Overdose
Overdose
Symptoms
In controlled clinical trials, single doses of empagliflozin up to 800 mg (32 times the maximum daily dose) in healthy volunteers and multiple doses up to 100 mg (4 times the maximum daily dose) in patients with type 2 diabetes were well tolerated. The observed increase in urine volume was independent of the dose and had no clinical significance. There is no experience with doses exceeding 800 mg.
Treatment
In case of overdose, it is recommended to remove the unabsorbed drug from the gastrointestinal tract, carry out clinical monitoring and carry out symptomatic treatment.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25°C. Keep out of the reach of children.
Shelf life
Shelf life
3 years
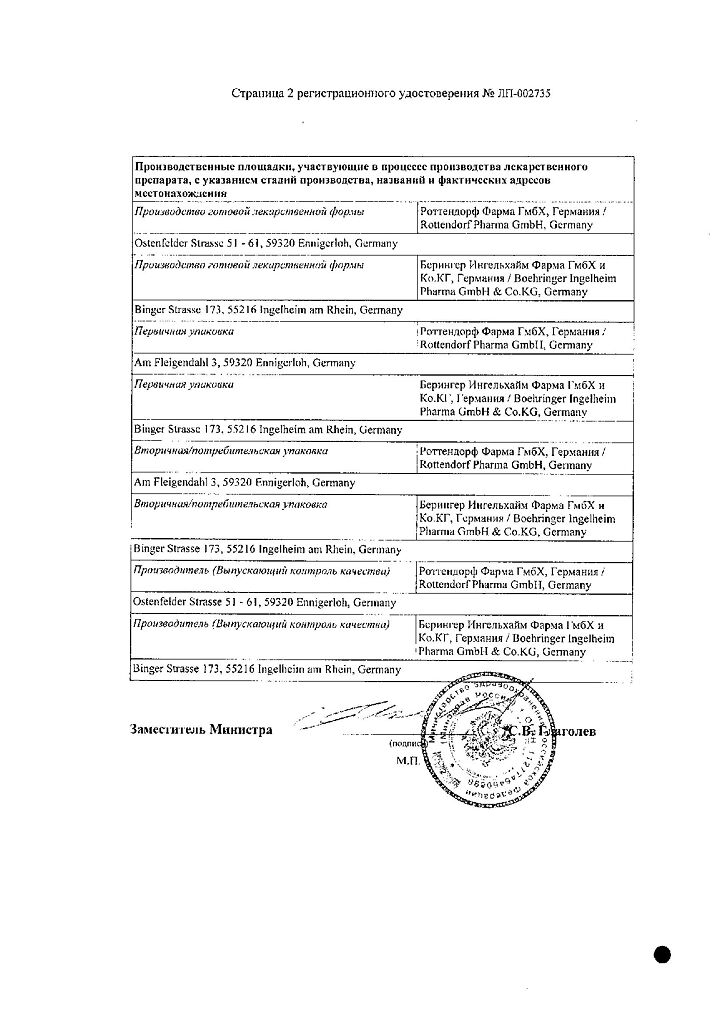
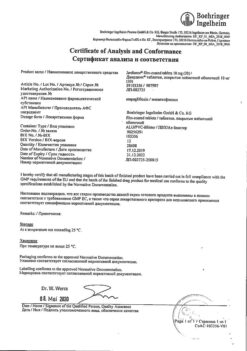
Manufacturer
Manufacturer
Boehringer Ingelheim International GmbH, Germany
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25°C. Keep out of reach of children. |
| Manufacturer | Boehringer Ingelheim International GmbH, Germany |
| Medication form | pills |
| Brand | Boehringer Ingelheim International GmbH |
Other forms…
Related products
Buy Jardins, 25 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.