No products in the cart.
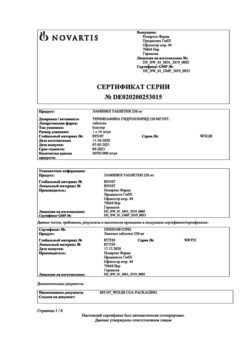
Itraconazole, 100 mg capsules 14 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group:antifungal agent.
ATH code: J02AC02
Pharmacokinetics
Due to non-linear pharmacokinetics, itraconazole accumulates in blood plasma when taken repeatedly. The equilibrium concentration (Css) of itraconazole is usually reached within about 15 days, while the maximum concentration (Cmax) and AUC (area under the curve “concentration-time”) values of itraconazole during multiple administration are 4-7 times higher than when administered single time. Maximum equilibrium plasma concentration (Cssmax) of itraconazole is about 2 mcg/ml when administered 200 mg itraconazole once daily. Final elimination half-life (T1/2) usually is 16-28 hours in single dose and 34-42 hours in multiple dose. Concentration of itraconazole in plasma decreases to almost undetectable value during 7-14 days after discontinuation of therapy, depending on the dose prescribed and the duration of treatment. Clearance of itraconazole decreases at higher doses due to saturation of its metabolization pathways in the liver.
Absorption
Itraconazole is rapidly absorbed after oral administration. Cssmax of unchanged itraconazole in plasma is reached within 2-5 hours after oral administration. Absolute bioavailability (F) of itraconazole after oral administration is about 55%. During oral administration maximum F of itraconazole is observed when taking capsules immediately after a meal.
Absorption of itraconazole in capsules is decreased in patients with low acidity of gastric juice, for example, during usage of medicines suppressing secretion of hydrochloric acid in stomach (such as H2-histamine ‑receptor antagonists‑, proton pump inhibitors), or in patients with achlorhydria during different diseases. Absorption of itraconazole on an empty stomach in such patients is increased when taking the drug simultaneously with acidic beverages (such as non-diet coke). Absorption of itraconazole remains unchanged at a dose of 200 mg once daily on an empty stomach together with non-dietic cola after prior use of H2-histamine ‑receptor ‑antagonist ‑ranitidine.
Exposure to itraconazole is lower when taking itraconazole as a capsule compared with exposure to itraconazole.
Distribution
Itraconazole binds 99.8% to plasma proteins, mainly to albumin (hydroxyitraconazole binds to albumin by 99.6%). Affinity to lipids is also noted. Only 0.2% of itraconazole remains unbound in plasma. Apparent volume of distribution (Vd) >700 l, indicating its significant distribution in tissues. Concentrations in the lungs, kidneys, bones, stomach, spleen and muscles, are 2-3 times higher than the corresponding concentrations in plasma, while the drug concentration in tissues containing keratin, especially in the skin, is about 4 times higher than the concentration in plasma. Concentration in cerebrospinal fluid is significantly lower than in plasma, however, the effectiveness of itraconazole against infectious agents present in cerebrospinal fluid has been demonstrated.
Metabolism
As shown in in vitro studies, CYP3A4 is the main isoenzyme involved in the metabolism of itraconazole. Itraconazole undergoes active metabolism in the liver with the formation of numerous metabolites. The main metabolite is hydroxyitraconazole, which in vitro has antifungal activity comparable with itraconazole. Concentrations of hydroxyitraconazole in plasma are about 2 times higher than concentrations of itraconazole.
Excretion
Itraconazole is excreted mainly as inactive metabolites with urine (35%) and feces (54%) for 1 week after oral solution administration. Renal excretion of itraconazole and its active metabolite hydroxyitraconazole is less than 1% of the dose of the drug administered intravenously. On the basis of results of studying pharmacokinetics of 14Cmethylated ‑drug after oral administration the excretion of unchanged itraconazole with feces varies from 3% to 18% of the dose taken.
As redistribution of itraconazole from tissues containing keratin is insignificant, excretion of itraconazole from these tissues is associated with regeneration of epidermis. In ‑contrast to blood plasma, the concentration of itraconazole in the skin is maintained for 2 to 4 weeks after stopping the 4-week ‑treatment, and the concentration in the nail keratin, where itraconazole can be detected as early as 1 week after starting treatment, is maintained for at least 6 months after the end of the 3-month ‑course of treatment.‑
Special patient categories
. Impaired liver function
Itraconazole is predominantly metabolized in the liver. A pharmacokinetic study compared the pharmacokinetic parameters of patients with cirrhosis and healthy volunteers. In patients with cirrhosis, the mean plasma Cmax was significantly lower (by 47%) than in healthy volunteers when a single dose of 100 mg of itraconazole was administered. The mean T1/2 on a single dose was increased in patients with cirrhosis and was 37 ± 17 hours compared to 16 ± 5 hours for healthy volunteers. Mean exposure of itraconazole (AUC) was similar in patients with cirrhosis and in healthy volunteers. There are no data on long-term use of itraconazole in patients with cirrhosis (see sections “Dosage and administration” and “Cautions”).
Renal dysfunction.
There are limited data on oral use of itraconazole in patients with renal dysfunction. In patients with uremia who had a mean creatinine clearance (CK) of 13 mL/min × 1.73 m2, the systemic exposure (AUC) of itraconazole was slightly lower compared to the main population. There was no significant effect of hemodialysis or long-term outpatient peritoneal dialysis on itraconazole pharmacokinetics (Tmax, Cmax and AUC0-8 h).
After a single intravenous administration of the drug, the final T1/2 of itraconazole in patients with mild (defined in the study as CK 50-79 ml/min), moderate (CK 20-49 ml/min) or severe renal impairment (CK < 20 ml/min) similar to that in healthy subjects (range of mean values 42-49 hours compared to 48 hours in patients with impaired renal function and healthy volunteers, respectively). Total exposure to itraconazole, based on the AUC score, was reduced in patients with moderate and severe renal impairment by approximately 30% and 40%, respectively, compared to patients with no renal impairment.
Data on long-term use of itraconazole in patients with renal impairment are not available. Dialysis has no effect on the T1/2 or clearance of itraconazole or hydroxyitraconazole.
Children
Data on the pharmacokinetics of itraconazole in pediatric patients are limited. Clinical studies of pharmacokinetics in children and adolescents aged 5 months to 17 years were conducted using itraconazole in capsules, oral solution, and intravenous solution. Individual doses of the drug in capsule form and oral solution ranged from 1.5 to 12.5 mg/kg/day when taken once or twice daily. When receiving itraconazole in the same daily dose twice a day compared to once daily administration, Cmax and Cmin were comparable to those in adult patients when taking itraconazole once a day. There were no significant age-related differences in AUC and total clearance of itraconazole; in rare cases a slight correlation between the age of patients and values of Vd of the drug, Cmax and final T1/2 was observed. The established clearance of itraconazole and its Vd depend on the body weight of patients.
Pharmacodynamics
Itraconazole is a synthetic antifungal agent of broad spectrum action, a triazole derivative. Mechanism of action of itraconazole is inhibition of ergosterol biosynthesis – the main component of the cell membrane of fungus, involved in maintaining the structural integrity of the membrane. Violation of ergosterol synthesis leads to changes in membrane permeability and cell lysis, which determines antifungal effect of the drug.
Itraconazole is active against infections caused by fungi:
– dermatophytes (Trichophyton spp, Microsporum spp., Epidermophyton floccosum);
– yeast-like fungi (Candida spp, including C. albicans, C. tropicalis, C. parapsilosis, C. krusei, Cryptococcus neoformans, Malassezia spp., Trichosporon spp., Geotrichum spp.); Aspergillus spp, including H. capsulatum; Paracoccidioides brasiliensis; Sporothrix schenckii; Fonsecaea spp.; Cladosporium spp.; Blastomyces dermatitidis; Coccidioides immitis, Pseudallescheria boydii; Penicillium marneffei and many others.
Candida krusei, Candida glabrata and Candida tropicalis are the least sensitive Candida species to the action of itraconazole.
The main types of fungi whose development is not inhibited by itraconazole are Zygomyces (Rhizopus spp, Rhizomucor spp., Mucor spp. and Absidia spp.), Fusarium spp., Scedosporium spp. and Scopulariopsis spp.
Resistance to azoles develops slowly and is often the result of several genetic mutations. Described mechanisms for the development of resistance include overexpression of the ERG11 gene encoding the 14α-demethylase enzyme, which is the primary target of azole action, and point mutations in ERG11 that result in reduced enzyme binding to azoles and/or activation of transport systems, resulting in increased azole excretion. Cross-resistance of Candida spp. to azole group drugs has been observed, although resistance to one drug of this group does not necessarily mean resistance to other drugs of the azole group. Aspergillus fumigatus strains resistant to itraconazole have been reported.
Indications
Indications
– Lesions of the skin and mucous membranes: vulvovaginal candidiasis; ringworm; pityriasis versicolor; candidiasis of the oral mucosa; fungal keratitis.
– Onychomycosis caused by dermatophytes and/or yeast-like fungi.
– Systemic mycoses: systemic aspergillosis and candidiasis; cryptococcosis (including cryptococcal meningitis): in immunocompromised patients and all patients with central nervous system cryptococcosis, itraconazole should be prescribed only in cases where first-line treatment is not applicable or effective; histoplasmosis; sporotrichosis; paracoccidioidomycosis; blastomycosis; other rare systemic or tropical mycoses.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antifungal agent.
ATX code: J02AC02
Pharmacokinetics
Due to nonlinear pharmacokinetics, itraconazole accumulates in the blood plasma after repeated doses. Steady-state concentrations (Css) of itraconazole are generally achieved within approximately 15 days, with the values of the maximum concentration (Cmax) of itraconazole and AUC (area under the concentration-time curve) with repeated dosing being 4-7 times higher than with a single dose. The maximum steady-state concentration of itraconazole in plasma (Cssmax) is about 2 mcg/ml when 200 mg of itraconazole is administered once a day. The terminal half-life (T1/2) is usually 16–28 hours with a single dose and 34–42 hours with multiple doses. The concentration of itraconazole in the blood plasma decreases to an almost undetectable value within 7-14 days after discontinuation of therapy, depending on the prescribed dose and duration of treatment. Clearance of itraconazole decreases at higher doses due to saturation of its metabolic pathways in the liver.
Absorption
Itraconazole is rapidly absorbed after oral administration. Cssmax of unchanged itraconazole in plasma is achieved within 2-5 hours after oral administration. The absolute bioavailability (F) of itraconazole after oral administration is approximately 55%. When administered orally, the maximum Fmax of itraconazole is observed when taking capsules immediately after meals.
Absorption of itraconazole capsules is reduced in patients with low gastric acidity, for example, while taking drugs that suppress the secretion of hydrochloric acid in the stomach (such as H2-histamine receptor antagonists, proton pump inhibitors), or in patients with achlorhydria due to various diseases. Fasting absorption of itraconazole in these patients is increased when the drug is taken concomitantly with acidic drinks (such as non-diet cola). Absorption of itraconazole remains unchanged when administered at a single dose of 200 mg on an empty stomach with non-diet cola after prior administration of the H2-receptor antagonist ranitidine.
Itraconazole exposure is lower with itraconazole capsules compared to exposure with itraconazole. when taking the same dose as an oral solution.
Distribution
Itraconazole is 99.8% bound to plasma proteins, mainly to albumin (hydroxyitraconazole is 99.6% bound to albumin). Affinity for lipids has also been noted. Only 0.2% of itraconazole remains in unbound form in the plasma. The apparent volume of distribution (Vd) is >700 L, indicating significant tissue distribution. Concentrations in the lungs, kidneys, bones, stomach, spleen and muscles are 2-3 times higher than the corresponding plasma concentrations, while drug concentrations in keratin-containing tissues, especially the skin, are approximately 4 times higher than plasma concentrations. Concentrations in cerebrospinal fluid are significantly lower than in plasma, however, itraconazole has been demonstrated to be effective against pathogens present in the cerebrospinal fluid.
Metabolism
CYP3A4 has been shown to be the main isoenzyme involved in the metabolism of itraconazole in in vitro studies. Itraconazole undergoes active metabolism in the liver with the formation of many metabolites. The main metabolite is hydroxyitraconazole, which in vitro has antifungal activity comparable to itraconazole. Plasma concentrations of hydroxyitraconazole are approximately 2 times higher than those of itraconazole.
Excretion
Itraconazole is excreted primarily as inactive metabolites in urine (35%) and feces (54%) within one week after dosing the oral solution. Renal excretion of itraconazole and its active metabolite hydroxyitraconazole is less than 1% of the dose administered intravenously. Based on the results of studying the pharmacokinetics of the 14C-labeled drug after oral administration, excretion of unchanged itraconazole in feces varies from 3% to 18% of the dose taken.
Since the redistribution of itraconazole from tissues containing keratin is negligible, the elimination of itraconazole from these tissues is associated with epidermal regeneration. In contrast to blood plasma, itraconazole concentrations in the skin persist for 2 to 4 weeks after cessation of 4 weeks of treatment, and concentrations in nail keratin, where itraconazole can be detected as early as 1 week after initiation of treatment, persist for at least 6 months after completion of a 3-month course of treatment.
Special categories of patients
Liver dysfunction
Itraconazole is predominantly metabolized in the liver. The pharmacokinetic study compared the pharmacokinetic parameters of patients with cirrhosis and healthy volunteers. In patients with liver cirrhosis, with a single dose of 100 mg itraconazole, the average Cmax in plasma was significantly lower (47%) than in healthy patients. The mean T1/2 with a single dose was increased in patients with cirrhosis and was 37 ± 17 hours compared to 16 ± 5 hours for healthy volunteers. The mean itraconazole exposure (AUC) was similar in patients with cirrhosis and healthy volunteers. There are no data on long-term use of itraconazole in patients with liver cirrhosis (see sections “Dosage and Administration” and “Special Instructions”).
Renal dysfunction.
There are limited data on the use of oral itraconazole in patients with renal impairment. In patients with uremia, whose mean creatinine clearance (CC) was 13 ml/min × 1.73 m2, systemic itraconazole exposure (AUC) was slightly lower compared with the general population. There was no significant effect of hemodialysis or long-term peritoneal dialysis performed in an outpatient setting on the pharmacokinetics of itraconazole (Tmax, Cmax and AUC0-8 h).
After a single intravenous administration of the drug, the final half-life of itraconazole in patients with mild (defined in the study as CK 50-79 ml/min), moderate (CR 20-49 ml/min) or severe renal impairment (CR < 20 ml/min) is similar to that in healthy people (mean range 42-49 hours compared with 48 hours in patients with impaired renal function and healthy volunteers, respectively). Total exposure to itraconazole, based on AUC, was reduced in patients with moderate to severe renal impairment by approximately 30% and 40%, respectively, compared with patients without impaired renal function.Data on long-term use of itraconazole in patients with impaired renal function are not available. Dialysis does not affect T1/2 or clearance of itraconazole or hydroxyitraconazole.ChildrenData on the pharmacokinetics of itraconazole in pediatric patients are limited. Clinical pharmacokinetic studies in children and adolescents aged 5 months to 17 years were conducted using itraconazole capsules, oral solution and intravenous solution. Individual doses of the drug in the form of capsules and oral solution ranged from 1.5 to 12.5 mg/kg/day when taken 1 or 2 times a day. When taking itraconazole at the same daily dose twice a day compared with once a day, Cmax and Cmin were comparable to those in adult patients when taking itraconazole once a day. There were no significant age-related differences in itraconazole AUC or total clearance; in rare cases, a slight relationship was observed between the age of patients and the values of Vd of the drug, Cmax and final T1/2. The established clearance of itraconazole and its Vd depend on the body weight of the patients.PharmacodynamicsItraconazole is a synthetic broad-spectrum antifungal agent, a triazole derivative. The mechanism of action of itraconazole is to inhibit the biosynthesis of ergosterol, a major component of the fungal cell membrane involved in maintaining the structural integrity of the membrane. Violation of ergosterol synthesis leads to changes in membrane permeability and cell lysis, which determines the antifungal effect of the drug.Itraconazole is active against infections caused by fungi:– dermatophytes (Trichophyton spp., Microsporum spp., Epidermophyton floccosum);– yeast-like fungi (Candida spp., including C. albicans, C. tropicalis, C. parapsilosis, C. krusei, Cryptococcus neoformans, Malassezia spp., Trichosporon spp., Geotrichum spp.); Aspergillus spp.; Histoplasma spp., including H. capsulatum; Paracoccidioides brasiliensis; Sporothrix schenckii; Fonsecaea spp.; Cladosporium spp.; Blastomyces dermatitidis; Coccidioides immitis, Pseudallescheria boydii; Penicillium marneffei and many others.Candida krusei, Candida glabrata and Candida tropicalis are the least sensitive Candida species to the effects of itraconazole.The main types of fungi that are not inhibited by itraconazole are Zygomyces (Rhizopus spp., Rhizomucor spp., Mucor spp. and Absidia spp.), Fusarium spp., Scedosporium spp. and Scopulariopsis spp.Azole resistance develops slowly and is often the result of several genetic mutations. Described mechanisms for the development of resistance include overexpression of the ERG11 gene, encoding the enzyme 14α-demethylase, which is the main target of azoles, and point mutations in ERG11, leading to a decrease in the binding of enzymes to azoles and/or activation of transport systems, which leads to increased excretion of azoles. Cross-resistance of Candida spp. has been observed. to drugs of the azole group, although resistance to one drug of this group does not necessarily mean resistance to other drugs of the azole group. Strains of Aspergillus fumigatus resistant to itraconazole have been reported.
Special instructions
Special instructions
Effect on cardiac function: In a study of intravenous itraconazole, a transient asymptomatic decrease in left ventricular ejection fraction was observed, which normalized until the next infusion of the drug. The clinical significance of these data for oral dosage forms is unknown.
Itraconazole has a negative inotropic effect. Cases of chronic heart failure associated with itraconazole have been reported. At a daily dose of 400 mg of itraconazole, an increased incidence of heart failure was observed; at lower daily doses such a pattern was not revealed. The risk of chronic heart failure is presumably proportional to the daily dose. The drug should not be taken by patients with chronic heart failure or with a history of this symptom complex, unless the possible benefit significantly outweighs the potential risk. When individually assessing the balance of benefit and risk, factors such as the severity of the indications, dosage regimen and individual risk factors for heart failure (coronary heart disease, valvular disease, obstructive pulmonary disease, renal failure and other diseases accompanied by edema) should be taken into account. Such patients should be informed about the signs and symptoms of chronic heart failure and monitored for their occurrence during the course of treatment. If such signs appear, the drug should be stopped.
Life-threatening cardiac arrhythmias and/or sudden death have been reported in patients receiving methadone concomitantly.
Drug interactions: Concomitant use of certain drugs with itraconazole may result in changes in the effectiveness of itraconazole and/or concomitant drugs, life-threatening adverse reactions and/or sudden death. Drugs that should not be taken concomitantly with itraconazole, are not recommended for concomitant use, and/or are recommended for concomitant use with itraconazole with caution are listed in the Interactions with Other Drugs section.
Cross-hypersensitivity: There is limited data regarding the presence of cross-hypersensitivity between itraconazole and other azole antifungals. If hypersensitivity to other azoles is present, itraconazole should be prescribed with caution.
Interchangeability: The interchangeable use of itraconazole capsule and oral solution is not recommended due to the fact that exposure to itraconazole is higher when it is used in oral solution than in capsule form, even when taking the same doses of itraconazole.
Reduced acidity of gastric juice: with reduced acidity of gastric juice, the absorption of itraconazole from capsules is impaired. In patients with reduced gastric acidity due to medical conditions (eg, patients with achlorhydria) or due to medications (eg, gastric suppressants), it is recommended that itraconazole be taken concomitantly with acidic drinks (such as non-diet cola). The antifungal activity of the drug should be monitored and the dose of itraconazole should be increased if necessary.
Effect on liver function: In very rare cases, severe toxic liver damage has occurred with the use of the drug, including several cases of acute liver failure with a fatal outcome. In most cases, this occurred in patients who already had liver disease, in patients with other serious diseases for whom the drug was prescribed for the treatment of systemic diseases, as well as in patients receiving other drugs that have hepatotoxic effects. However, some patients had no comorbidities or obvious risk factors for liver damage. Several such cases occurred in the first month of therapy, and some in the first week of treatment. In this regard, it is recommended to regularly monitor liver function in patients receiving itraconazole therapy. If symptoms suggestive of hepatitis occur, namely anorexia, nausea, vomiting, weakness, abdominal pain and dark urine, treatment should be stopped immediately and liver function testing should be performed. Patients with elevated liver enzymes or active liver disease, or history of liver toxicity due to other medications, should not be treated with itraconazole unless the expected benefit justifies the risk of liver damage. In such cases, it is necessary to monitor the activity of liver enzymes during treatment. Itraconazole is predominantly metabolized in the liver. Since the total half-life of itraconazole is slightly increased in patients with impaired liver function, it is recommended to monitor itraconazole plasma concentrations and adjust the dose of the drug if necessary.
Renal impairment: Data on the use of the drug in patients with impaired renal function are limited, and exposure to itraconazole may be reduced in some patients with impaired renal function. Therefore, such patients should be prescribed the drug with caution. It is recommended to monitor plasma concentrations of itraconazole and, if necessary, adjust the dose of the drug.
Immunocompromised patients: The oral bioavailability of itraconazole may be reduced in some immunocompromised patients, such as neutropenic patients, patients with AIDS, or those undergoing organ transplantation.
Patients with life-threatening systemic fungal infections: Due to the pharmacokinetic characteristics of itraconazole, its use is not recommended for the initiation of treatment of life-threatening systemic mycoses in patients.
Patients with AIDS: The attending physician should evaluate the need for maintenance therapy in patients with AIDS who have previously been treated for systemic fungal infections, such as sporotrichosis, blastomycosis, histoplasmosis, or cryptococcosis (both meningeal and nonmeningeal), and who are at risk of relapse.
Use in pediatric practice: Since there is insufficient clinical data on the use of itraconazole in children, it is recommended to prescribe the drug to children only if the possible benefits of treatment outweigh the potential risks.
Women of childbearing potential taking itraconazole should use adequate contraception throughout the course of treatment until the first menstrual period after completion of treatment.
Treatment should be discontinued if peripheral neuropathy occurs, which may be associated with Itraconazole.
In systemic candidiasis suspected to be caused by fluconazole-resistant Candida strains, sensitivity to itraconazole cannot be assumed, and it is therefore recommended to test sensitivity before initiating itraconazole therapy.
Hearing loss: Temporary or permanent hearing loss has been reported in patients taking itraconazole. In some cases, hearing loss occurred during concomitant use with quinidine (see sections “Contraindications” and “Interaction with other drugs”). Hearing usually recovers after completion of Itraconazole therapy, but in some patients hearing loss is irreversible.
Fertility: Animal studies have not shown reproductive toxicity with itraconazole.
Cystic fibrosis: In patients with cystic fibrosis, variability in itraconazole plasma concentrations was observed when itraconazole oral solution was administered at a dose of 2.5 mg/kg twice daily. As a result, the therapeutic equilibrium concentration of itraconazole in blood plasma may not be achieved. Steady-state concentrations >250 ng/mL were achieved in approximately 50% of patients over 16 years of age and were not achieved in any patient under 16 years of age. If there is no response to Itraconazole therapy, switching to alternative therapy should be considered.
Impact on the ability to drive vehicles and machinery
Studies have not been conducted to study the effect of itraconazole on the ability to drive vehicles and operate machinery. It is necessary to take into account the possibility of adverse reactions, such as dizziness, blurred vision and hearing loss (see “Side effects”). If the described adverse events occur, you should refrain from performing these activities.
Active ingredient
Active ingredient
Itraconazole
Composition
Composition
Each capsule contains itraconazole pellets (22%) – 0.460 g.
Pellet composition:
active substance: itraconazole – 0.100 g;
excipients: hypromellose (hydroxypropyl methylcellulose E-5) – 0.1472 g, butyl methacrylate, dimethylaminoethyl methacrylate and methyl methacrylate copolymer [1:2:1] (eudragit E-100) – 0.0046 g, sucrose (sugar) – 0.2070 g.
Composition of the capsule shell:
body: gelatin, titanium dioxide (E 171), azorubine (carmoisine) E 122;
cap: gelatin, titanium dioxide (E 171), indigo carmine – F D&C Blue 2 (E 132).
Pregnancy
Pregnancy
Pregnancy
Itraconazole should not be used during pregnancy, except in life-threatening cases and if the expected benefit to the mother outweighs the possible harm to the fetus.
Itraconazole has been shown to have reproductive toxicity in preclinical studies. There is insufficient data on the use of itraconazole during pregnancy. During the clinical use of the drug after registration, cases of congenital anomalies were noted. Such cases included developmental disorders of vision, skeleton, genitourinary and cardiovascular systems, as well as chromosomal disorders and multiple malformations. However, whether the use of itraconazole is the cause of these disorders has not been reliably established.
Epidemiological data regarding exposure to itraconazole during the first trimester of pregnancy, mainly in patients receiving short-term therapy for vulvovaginal candidiasis, did not reveal an increased risk of congenital anomalies compared with controls not exposed to any known teratogens.
Women of childbearing potential taking itraconazole should use highly effective methods of contraception throughout the course of treatment until the first menstrual period after completion of treatment.
Breastfeeding period
Very small amounts of itraconazole are excreted in breast milk. When prescribing itraconazole to breastfeeding women, it is necessary to weigh the expected benefits and risks. If in doubt, a woman should refuse to breastfeed.
Contraindications
Contraindications
Hypersensitivity to itraconazole or excipients.
Concomitant use of drugs that are substrates of the CYP3A4 isoenzyme (see section “Interaction with other drugs”), such as:
Levacetylmethadol, methadone;
· disopyramide, dofetilide, dronedarone, quinidine;
Telithromycin in patients with severe renal or hepatic impairment;
· ticagrelor;
· halofantrine;
· astemizole, mizolastine, terfenadine;
Ergot alkaloids: dihydroergotamine, ergometrine (ergonovine), ergotamine, methylergometrine (methylergonovine), eletriptan;
irinotecan;
lurasidone, oral midazolam, pimozide, sertindole, triazolam;
· bepridil, felodipine, lercanidipine, nisoldipine;
· ivabradine, ranolazine;
· eplerenone;
· cisapride, domperidone;
lovastatin, simvastatin, atorvastatin;
fesoterodine in patients with moderate or severe renal or hepatic impairment, solifenacin in patients with severe renal impairment and moderate or severe hepatic impairment;
Colchicine in patients with impaired liver or kidney function.
Chronic heart failure currently or in history (with the exception of treatment of life-threatening or other dangerous infections, see section “Special Instructions”).
Fructose intolerance, sucrase/isomaltase deficiency, glucose-galactose malabsorption.
Children under 3 years of age.
Pregnancy and breastfeeding.
With caution
With cirrhosis of the liver; severe impairment of liver and kidney function; hypersensitivity to azoles; in elderly patients; in children.
Side Effects
Side Effects
According to the World Health Organization (WHO), undesirable effects are classified according to the frequency of their development as follows: very often (≥1/10), often (>1/100 and 1/1000 and 1/10000 and <1/1000) and very rarely (<1/10000), including isolated cases; frequency unknown - cannot be calculated from available data.Data obtained from clinical studiesThe safety of treatment was assessed in 107 open-label and double-blind clinical studies involving 8499 patients, in which all patients took at least one dose of itraconazole.Infectious and parasitic diseases:
Uncommon: rhinitis, sinusitis, upper respiratory tract infections.
Disorders of the hematopoietic and lymphatic systems:
Rare: leukopenia;
Frequency unknown: neutropenia.
Immune system disorders:
Uncommon: hypersensitivity.
Nervous system disorders:
Often: headache;
Rarely: hypoesthesia, paresthesia.
Hearing and labyrinthine disorders:
Rare: ringing in the ears.
Gastrointestinal disorders:
Common: abdominal pain, nausea;
Uncommon: dyspepsia, constipation, flatulence, diarrhea, vomiting;
Rarely: dysgeusia.
Liver and biliary tract disorders:
Uncommon: hyperbilirubinemia, liver dysfunction.
Disorders of the skin and subcutaneous fat:
Uncommon: rash, itching, urticaria.
Renal and urinary tract disorders:
Rarely: pollakiuria.
Disorders of the reproductive system and mammary glands:
Uncommon: menstrual irregularities;
Rare: erectile dysfunction.
General complications and reactions at the injection site:
Rarely: edematous syndrome.
The following is a list of adverse reactions associated with the administration of itraconazole oral solution and/or intravenous solution (excluding adverse reactions classified as injection site inflammation, since these adverse reactions are specific to the intravenous solution dosage form).
Disorders of the hematopoietic and lymphatic systems:
Granulocytopenia, thrombocytopenia.
Immune system disorders:
Anaphylactoid reactions.
Metabolic disorders:
Hyperglycemia, hyperkalemia, hypokalemia, hypomagnesemia.
Mental disorders:
Confusion.
Nervous system disorders:
Peripheral neuropathy, dizziness, drowsiness.
Cardiovascular system disorders:
Heart failure, left ventricular failure, tachycardia, arterial hypertension, arterial hypotension.
Disorders of the respiratory system, chest and mediastinal organs:
Pulmonary edema, dysphonia, cough.
Gastrointestinal disorders:
Gastrointestinal disorders.
Liver and biliary tract disorders:
Hepatitis, jaundice, liver dysfunction.
Skin and subcutaneous tissue disorders:
Erythematous rash, hyperhidrosis.
Musculoskeletal and connective tissue disorders:
Myalgia, arthralgia.
Renal and urinary tract disorders:
Renal failure, urinary incontinence.
General disorders and disorders at the injection site:
Generalized edema, facial swelling, chest pain, pyrexia, pain, fatigue, chills.
Influence on the results of laboratory parameters and instrumental studies:
Increased alanine aminotransferase activity, increased aspartate aminotransferase activity, increased alkaline phosphatase activity in blood plasma, increased lactate dehydrogenase activity in blood plasma, increased blood urea concentration, increased gamma-glutamyl transferase activity, increased liver enzyme activity, abnormal urinalysis.
Children
The safety of itraconazole was assessed in 14 clinical studies (4 double-blind, placebo-controlled studies, 9 open-label studies, and 1 open-label followed by double-blind study) involving 165 children aged 1 to 17 years. During the studies, it was noted that the most common adverse reactions were: headache, vomiting, abdominal pain, diarrhea, liver dysfunction, nausea, urticaria. The nature of adverse reactions occurring in children is similar to what is observed in adult patients; however, the incidence of adverse reactions is higher in children.
Side effects registered in the post-registration period (data obtained from spontaneous reports)
The presented frequency of adverse reactions is based on clinical experience with the use of itraconazole in capsule form after registration.
From the immune system:
Very rare: serum sickness, angioedema, anaphylactic, anaphylactoid and allergic reactions.
Metabolic disorders:
Very rare: hypertriglyceridemia.
Nervous system disorders:
Very rare: tremor.
From the side of the organ of vision:
Very rare: blurred vision, diplopia.
Hearing and labyrinthine disorders:
Very rare: permanent or temporary hearing loss.
From the cardiovascular system:
Very rare: chronic heart failure.
From the respiratory system:
Common: shortness of breath.
From the gastrointestinal tract:
Very rare: pancreatitis.
From the hepatobiliary system:
Very rare: severe toxic liver damage (including some cases of acute liver failure with death).
For the skin and subcutaneous fat:
Very rare: toxic epidermal necrolysis, Stevens-Johnson syndrome, acute generalized exanthematous pustulosis, erythema multiforme, exfoliative dermatitis, leukocytoclastic vasculitis, alopecia, photosensitivity.
Influence on the results of laboratory parameters and instrumental studies:
Very rare: increased activity of blood creatine phosphokinase.
Interaction
Interaction
Itraconazole is predominantly metabolized by the CYP3A4 isoenzyme. Other drugs that are also metabolized by this isoenzyme or alter its activity may affect the pharmacokinetics of itraconazole. Similarly, itraconazole may affect the pharmacokinetics of drugs that are also metabolized by this isoenzyme. Itraconazole is a strong inhibitor of the CYP3A4 isoenzyme and P-glycoprotein. When using itraconazole together with other drugs, it is recommended to read the instructions for use to determine the method of metabolism of the drug and decide whether it is necessary to change its dose.
Medicines that may decrease plasma concentrations of itraconazole
Medicines that reduce gastric acidity (for example, antacids such as aluminum hydroxide or acid suppressants such as H2 receptor antagonists and proton pump inhibitors) interfere with the absorption of Itraconazole. These drugs are recommended to be used with caution in combination with itraconazole:
– Itraconazole is recommended to be taken with acidic drinks (such as non-diet cola) when taking medications that reduce stomach acid.
– It is recommended to take medications that neutralize hydrochloric acid (for example, aluminum hydroxide) at least 1 hour before or 2 hours after taking Itraconazole.
– When taking drugs together, it is recommended to monitor the antifungal activity of itraconazole and increase the dose of the drug if necessary.
Concomitant use of itraconazole with strong inducers of the CYP3A4 isoenzyme may reduce the bioavailability of itraconazole and hydroxyitraconazole to such an extent that the effectiveness of the drug will be reduced. Examples include the following drugs:
– Antibacterial agents: isoniazid, rifabutin, rifampicin.
– Anticonvulsants: carbamazepine, phenobarbital, phenytoin.
– Antiviral drugs: efavirenz, nevirapine.
Therefore, the use of strong CYP3A4 inducers with itraconazole is not recommended. It is recommended to avoid prescribing these medications for 2 weeks before starting to take itraconazole and during treatment with the drug, unless the expected benefit outweighs the potential risk associated with a decrease in the effectiveness of itraconazole. When taking drugs together, it is recommended to monitor the antifungal activity of itraconazole and increase the dose of the drug if necessary.
Medicines that may cause an increase in plasma concentrations of itraconazole
Concomitant use of itraconazole and strong inhibitors of the CYP3A4 isoenzyme may lead to an increase in the bioavailability of itraconazole. Examples of strong inhibitors of the CYP3A4 isoenzyme:
– Antibacterial drugs: ciprofloxacin, clarithromycin, erythromycin.
– Antivirals: darunavir boosted with ritonavir, fosamprenavir boosted with ritonavir, indinavir, ritonavir and telaprevir.
These drugs are recommended to be used with caution in combination with itraconazole. It is recommended to carefully monitor the condition of patients taking itraconazole together with strong inhibitors of the CYP3A4 isoenzyme, for timely detection of symptoms and signs of increased or prolonged pharmacological effects of itraconazole, and if necessary, a reduction in the dose of itraconazole is possible. If possible, it is recommended to monitor the concentration of itraconazole in the blood plasma.
Medicines whose plasma concentrations may increase when used together with itraconazole
Itraconazole and its main metabolite hydroxyitraconazole may interfere with the metabolism of drugs metabolized by the CYP3A4 isoenzyme and interfere with the transport of drugs by P-glycoprotein. This may lead to increased plasma concentrations of these drugs and/or their active metabolites when taken together with itraconazole. Increased plasma concentrations, in turn, may increase or prolong both the therapeutic and undesirable effects of these drugs, resulting in potentially life-threatening conditions. Thus, increasing the concentration of certain drugs (terfenadine, astemizole, bepridil, mizolastine, cisapride, dofetilide, quinidine, pimozide, sertindole, levomethadone) can lead to an increase in the QT interval and ventricular tachyarrhythmia, including cases of torsade de pointes (TdP), which is a potentially life-threatening condition. After cessation of treatment, plasma concentrations of itraconazole decrease to virtually undetectable within 7 to 14 days, depending on the dose of the drug and duration of treatment. In patients with cirrhosis or those taking concomitant CYP3A4 enzyme inhibitors, the decrease in drug concentrations may be even slower. This is especially important when initiating therapy with drugs whose metabolism is affected by itraconazole.
Interacting drugs are divided into the following categories:
– “Contraindicated”: Under no circumstances should this drug be used in combination with itraconazole and for 2 weeks after stopping itraconazole.
– “Not recommended”: It is recommended to avoid the use of this drug during treatment and for 2 weeks after stopping use of itraconazole, unless the expected benefit outweighs the potential risk associated with the therapy. If the use of this combination of drugs cannot be avoided, it is recommended to monitor the patient’s condition to promptly identify symptoms and signs of increased or prolonged drug effects or the development of side effects; if necessary, treatment can be interrupted or the dose of drugs can be reduced. If possible, it is recommended to monitor plasma concentrations of drugs.
– “Use with caution”: Careful monitoring should be undertaken when using the drug together with itraconazole. When using drugs together, it is recommended to monitor the patient’s condition for timely detection of symptoms and signs of increased or prolonged drug effects or the development of side effects; if necessary, treatment can be interrupted or the dose of drugs can be reduced. If possible, it is recommended to monitor plasma concentrations of drugs.
Below are examples of drugs whose plasma concentrations may be increased by itraconazole. The drugs are divided into classes, and recommendations for combined use with itraconazole are also given:
Drug class
Contraindicated
Not recommended
Use with caution
Alpha – adrenergic blockers
Tamsulosin
Narcotic analgesics
Levacetylmethadol (levomethadyl), methadone
Fentanyl
Alfentanil, intravenous and sublingual buprenorphine, oxycodone, sufentanil
Antiarrhythmic drugs
Disopyramide, dofetilide, dronedarone, quinidine
Digoxin
Antibacterial agents
Telithromycin in patients with severe renal or hepatic impairment
Rifabutina
Telithromycin
Anticoagulants and antiplatelet agents
Ticagrelor
Apixaban, rivaroxaban
Coumarins, cilostazol, dabigatran
Anticonvulsants
Carbamazepine
Antidiabetic drugs
Repaglinide, saxagliptin
Anthelminthic and antiprotozoal agents
Halofantrine
Praziquantel
Antihistamines
Astemizole, mizolastine, terfenadine
Bilastine, ebastine
Anti-migraine medications
Ergot alkaloids such as dihydroergotamine, ergometrine (ergonovine), ergotamine, methylergometrine (methylergonovine), eletriptan
Antitumor drugs
Irinotecan
Axitinib, dafrafenib, dasatinib, ibrutinib, nilotinib sunitinib, trabectedin
Bortezomib, busulfan, docetaxel, erlotinib, gefitinib, imatinib, ixabepilone, lapatinib, ponatinib, trimetrexate, vinca alkaloids
Neuroleptics, anxiolytics and hypnotics
Lurasidone, oral midazolam, pimozide, sertindole, triazolam
Alprazolam, aripiprazole, brotizolam, buspirone, haloperidol, intravenous midazolam, perospirone, quetiapine, ramelteon, risperidone
Antiviral drugs
Simeprevir
Maraviroc, indinavirb, ritonavirb, saquinavir
Beta blockers
Nadolol
Blockers
“slow” calcium channels
Bepridil, felodipine, lercanidipine, nisoldipine
Other dihydropyridines, verapamil
Other drugs acting on the cardiovascular system
Ivabradine, ranolazine
Aliskiren, sildenafil in the treatment of pulmonary hypertension
Bosentan, riociguat
Diuretics
Eplerenone
Drugs affecting the gastrointestinal tract
Cisapride, domperidone
Aprepitant
Immunosuppressants
Everolimus
Budesonide, ciclesonide, cyclosporine, dexamethasone, fluticasone, methylprednisolone,
rapamycin (also known as sirolimus), tacrolimus, temsirolimus
Drugs that regulate lipid metabolism
Atorvastatin, lovastatin, simvastatin
Drugs used to treat respiratory diseases
Salmeterol
SSRIs,
tricyclics and other antidepressants
Reboxetine
Drugs used in urology
Fesoterodine
patients with
moderate or severe renal or hepatic insufficiency,
solifenacin in patients with severe renal impairment and moderate or severe hepatic impairment
Darifenacin, vardenafil
Fesoterodine, imidafenacin, oxybutynin, sildenafil in the treatment of erectile dysfunction, solifenacin, tadalafil, tolterodine
Other
Colchicine in patients with impaired liver or kidney function
Colchicine, conivaptan, tolvaptan
Alitretinoin (oral dosage forms), cinacalcet, mozavaptan.
a See also “Drugs that may reduce plasma concentrations of itraconazole”.
b See also section “Drugs that may increase plasma concentrations of itraconazole.”
Drugs whose plasma concentrations may be decreased by itraconazole
Concomitant use of itraconazole with the non-steroidal anti-inflammatory drug meloxicam may reduce plasma concentrations of meloxicam. It is recommended to prescribe meloxicam concomitantly with itraconazole with caution, and to carefully monitor the patient’s clinical condition and the occurrence of side effects. If necessary, the dose of meloxicam should be adjusted.
Children
Drug interactions have only been studied in adults.
Overdose
Overdose
The symptoms observed with itraconazole overdose were comparable to the dose-related adverse reactions observed with normal doses of the drug.
Treatment
There is no specific antidote. In case of overdose, maintenance therapy should be carried out, gastric lavage should be done with sodium bicarbonate solution, and activated charcoal should be given. Itraconazole is not removed from the body by hemodialysis.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after the expiration date indicated on the package.
Manufacturer
Manufacturer
Biocom JSC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C. Store out of the reach of children. |
| Manufacturer | Biocom AO, Russia |
| Medication form | capsules |
| Brand | Biocom AO |
Other forms…
Related products
Buy Itraconazole, 100 mg capsules 14 pcs with delivery to USA, UK, Europe and over 120 other countries.