No products in the cart.
Description
Irinotecan is a semi-synthetic derivative of camptothecin, a specific inhibitor of the cellular enzyme topoisomerase I. In tissues, the drug is metabolized to form the active metabolite SN-38, which is superior to irinotecan in its activity. Irinotecan and SN-38 stabilize the complex of topoisomerase I with DNA, which prevents the replication of the latter.
Pharmacokinetics
The pharmacokinetic profile of irinotecan is not dose dependent. Maximum plasma concentrations of irinotecan and SN-38 were reached by the end of the IV infusion at the recommended dose of 350 mg/m2. Binding to plasma proteins for irinotecan is approximately 65%, for its active metabolite SN-38 – 95%.
The distribution of the drug in plasma is biphasic or triphasic. It is metabolized mainly in liver under the action of carboxylesterase enzyme to the active metabolite – SN-38. Average T1/2 of the drug in the first phase is 12 min, in the second phase – 2.5 h and in the last phase – 14.2 h.
The drug is excreted in the urine within 24 hours as unchanged drug (20%) and as SN-38 (0.25%). About 30% of the drug is excreted with the bile, both as unchanged and as SN-38 glucuronide. 5-fluorouracil and calcium folinate do not affect the pharmacokinetics of irinotecan.
Indications
Indications
Locally advanced or metastatic cancer of the colon and rectum: as monotherapy in patients with disease progression after conventional treatment; in combination with 5-fluorouracil and calcium folinate in patients who have not previously received chemotherapy.
Pharmacological effect
Pharmacological effect
Irinotecan is a semisynthetic derivative of camptothecin and is a specific inhibitor of the cellular enzyme topoisomerase I. In tissues, the drug is metabolized to form the active metabolite SN-38, which is superior in activity to irinotecan. Irinotecan and SN-38 stabilize the topoisomerase I complex with DNA, which prevents DNA replication.
Pharmacokinetics
The pharmacokinetic profile of irinotecan is independent of dose. The maximum plasma concentration of irinotecan and SN-38 was achieved at the end of the IV infusion at the recommended dose of 350 mg/m2. Plasma protein binding for irinotecan is approximately 65%, for its active metabolite – SN-38 – 95%.
The distribution of the drug in plasma is two- or three-phase. Metabolized mainly in the liver under the action of the enzyme carboxylesterase to the active metabolite – SN-38. The average T1/2 of the drug in the first phase is 12 minutes, in the second – 2.5 hours and in the last – 14.2 hours.
It is excreted in the urine within 24 hours as unchanged drug (20%) and as SN-38 (0.25%). About 30% of the drug is excreted with bile, both unchanged and in the form of glucuronide SN-38. 5-fluorouracil and calcium folinate do not affect the pharmacokinetics of irinotecan.
Special instructions
Special instructions
Treatment with Iriten should be carried out in specialized chemotherapy departments under the supervision of a physician experienced in working with anticancer drugs. In patients receiving Iriten, it is necessary to do a detailed clinical blood test weekly and monitor liver function.
Diarrhea that occurs as a consequence of the cytotoxic effect of the drug (delayed diarrhea) is usually observed no earlier than 24 hours after administration of Iriten (in most patients, on average, after 5 days). When the first episode of loose stool occurs, it is necessary to prescribe plenty of fluids containing electrolytes and immediately carry out antidiarrheal therapy, including taking high doses of loperamide (4 mg at the first dose and then 2 mg every 2 hours).
This therapy is continued for at least 12 hours after the last episode of loose stool, but not more than 48 hours due to the possibility of developing paresis of the small intestine. If diarrhea is assessed as severe (more than 6 episodes of loose stools per day or severe tenesmus), and if it is accompanied by vomiting or fever, the patient should be urgently hospitalized for comprehensive treatment, including the administration of broad-spectrum antibiotics.
For moderate or mild diarrhea (less than 6 episodes of loose stools per day and moderate tenesmus), which does not stop within the first 48 hours, it is necessary to start taking broad-spectrum antibiotics orally, and it is recommended to hospitalize the patient. If diarrhea and severe neutropenia (white blood cell count less than 500/μl) occur simultaneously, broad-spectrum antibiotics are prescribed orally in addition to antidiarrheal therapy for prophylactic purposes.
Loperamide should not be prescribed prophylactically, incl. patients who have had diarrhea during previous administrations of Iriten. The patient must be warned in advance about the possibility of developing delayed diarrhea. Patients should immediately inform their doctor if diarrhea occurs and begin appropriate treatment immediately. With inadequate treatment of diarrhea, a life-threatening condition may develop, especially if diarrhea develops against the background of neutropenia. Patients with febrile neutropenia (body temperature >38°C and neutrophil count less than 1000/μl) should be promptly started on broad-spectrum antibiotics in a hospital setting.
With the development of acute cholinergic syndrome, in the absence of contraindications, the administration of 0.25 mg of atropine sulfate subcutaneously is indicated. Caution should be exercised when using the drug in patients with bronchial asthma. In patients with a history of indications for the development of acute cholinergic syndrome, incl. and in severe form, prophylactic administration of antiemetic drugs is recommended before prescribing Iriten.
Since the dosage form of the drug contains D-sorbitol as an excipient, Iriten cannot be used in patients with hereditary fructose intolerance. When preparing Iriten solution and handling the drug, care should be taken. It is necessary to use gloves, a mask and goggles.
If Iriten solution or infusion solution gets on the skin or mucous membranes, the skin should be immediately washed with soap and water, and the mucous membranes with just water.
Impact on the ability to drive vehicles and operate machinery
Patients should be warned about the possibility of dizziness and visual disturbances that develop within 24 hours after administration of the drug during treatment with Iriten. If these symptoms occur, patients are advised to refrain from driving or using other machinery.
Active ingredient
Active ingredient
Irinotecan
Composition
Composition
Active ingredient:
irinotecan hydrochloride trihydrate;
Excipients:
D-sorbitol,
lactic acid,
sodium hydroxide,
water d/i.
Pregnancy
Pregnancy
The drug is contraindicated for use during pregnancy and lactation (breastfeeding). During treatment with Iriten and for at least 3 months after discontinuation of therapy, reliable contraceptive measures should be used.
Contraindications
Contraindications
— chronic inflammatory bowel diseases and/or intestinal patency disorders;
– pronounced inhibition of bone marrow hematopoiesis;
– serum bilirubin level exceeding ULN by more than 1.5 times;
— general condition of patients, assessed according to the WHO scale>2;
– pregnancy;
– lactation period (breastfeeding);
– hypersensitivity to irinotecan or other components of the drug.
The drug should be prescribed with caution during radiation therapy (in history) to the abdominal or pelvic area, leukocytosis, and in female patients (the risk of developing diarrhea increases).
Side Effects
Side Effects
From the hematopoietic organs: neutropenia is observed on average in 80% of patients, incl. half of them have a decrease in neutrophils to
From the digestive system: late diarrhea, occurring more than 24 hours (on average 5 days) after drug administration, is a dose-limiting toxicity and is observed in approximately 87% of patients, of which 38% are severe. Nausea and vomiting usually occur on the first day of administration or after 24 hours in 85% of patients.
Dehydration has been reported due to vomiting and diarrhea, very rarely with the development of renal failure, hypotension and heart failure. Possible abdominal pain, anorexia, mucositis, constipation.
Acute cholinergic syndrome is observed in 9% of patients during the first 24 hours after administration of Iriten and is manifested by diarrhea, abdominal pain, increased sweating, miosis, visual disturbances, lacrimation, salivation, decreased blood pressure, dizziness, chills and general malaise.
From the central nervous system: involuntary muscle twitching or cramps, paresthesia, asthenia.
Allergic reactions: rarely – skin rash and very rarely – the development of anaphylactic shock. Other: shortness of breath, alopecia, increased body temperature, local reactions.
Interaction
Interaction
Since Iriten has anticholinesterase activity, there may be an increase in the duration of neuromuscular blockade when combined with suxamethonium and an antagonistic interaction with respect to neuromuscular blockade when combined with non-depolarizing muscle relaxants.
Pharmaceutical interactions Iriten should not be mixed with other drugs in the same bottle.
Overdose
Overdose
Since Iriten has anticholinesterase activity, there may be an increase in the duration of neuromuscular blockade when combined with suxamethonium and an antagonistic interaction with respect to neuromuscular blockade when combined with non-depolarizing muscle relaxants.
Pharmaceutical interactions Iriten should not be mixed with other drugs in the same bottle.
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 25 °C.
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
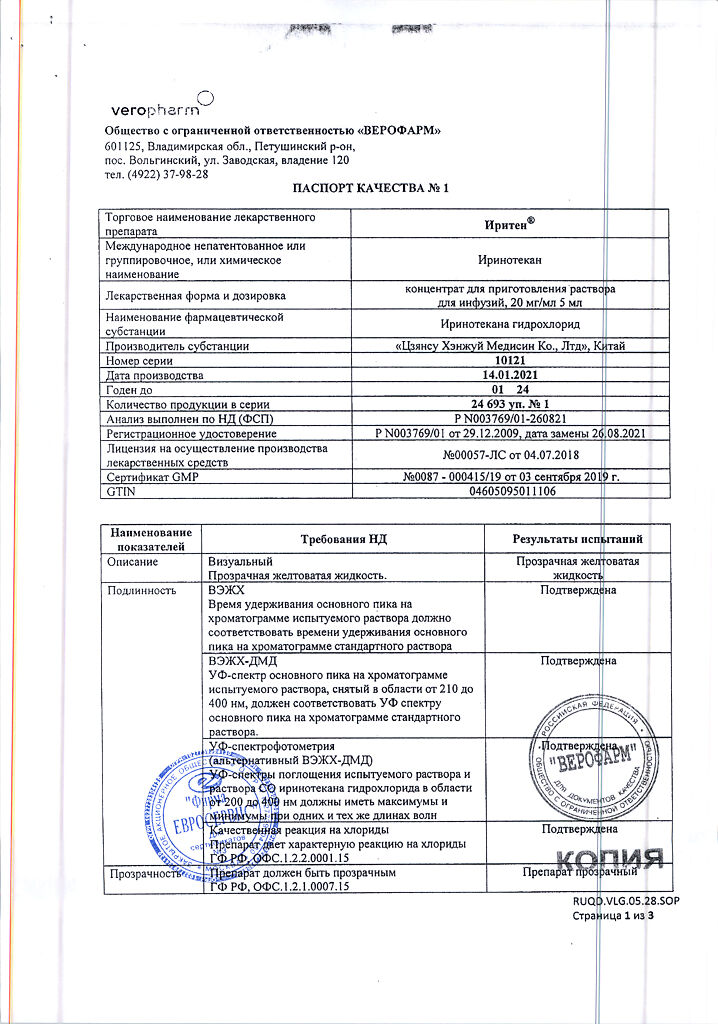
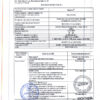
Veropharm LLC, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a light-protected place at a temperature not exceeding 25 °C. |
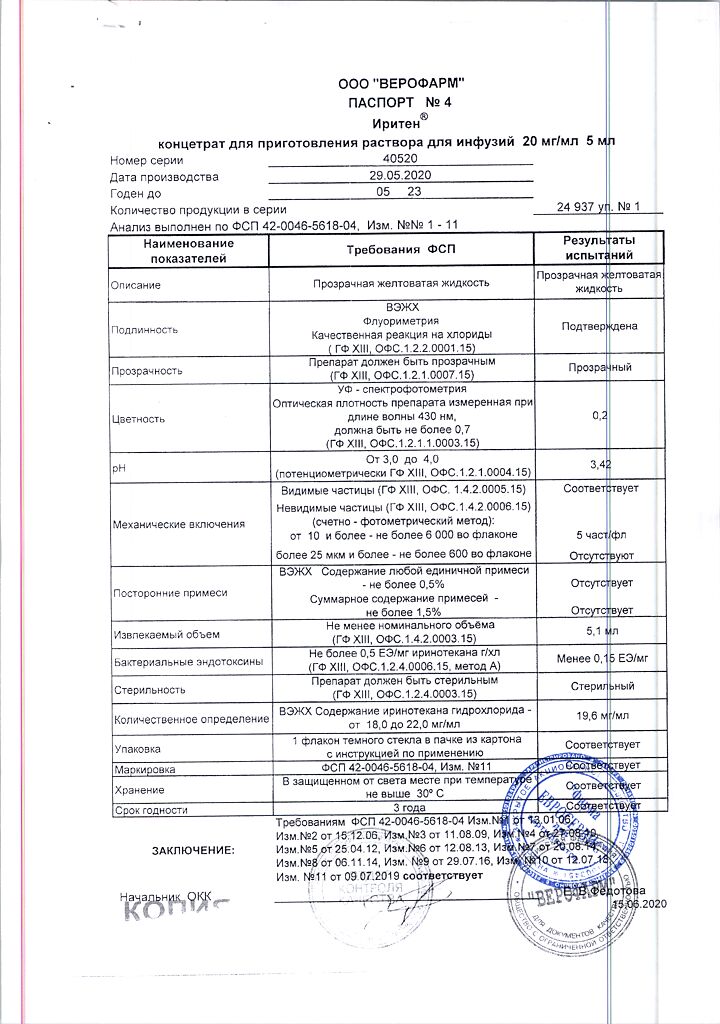
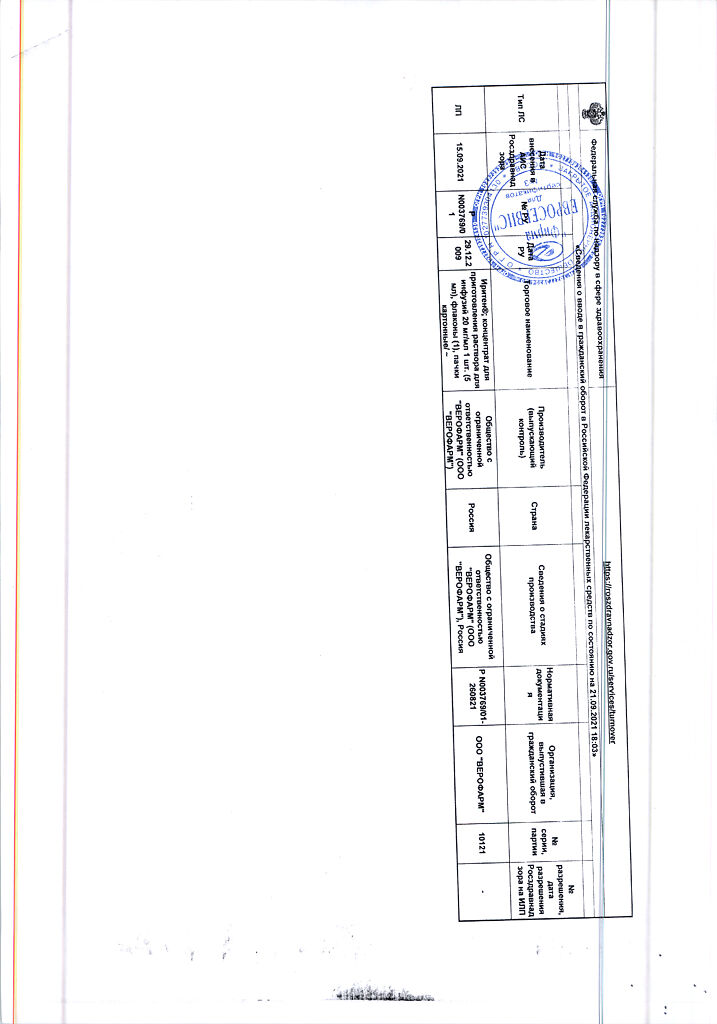
| Manufacturer | Veropharm AO, Russia |
| Medication form | concentrate for preparation of infusion solution |
| Brand | Veropharm AO |
Related products
Buy Iriten, 20 mg/ml 5 ml with delivery to USA, UK, Europe and over 120 other countries.