No products in the cart.
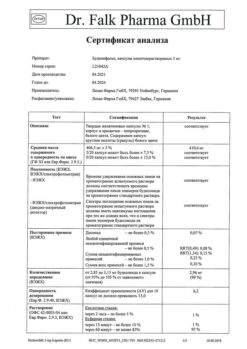
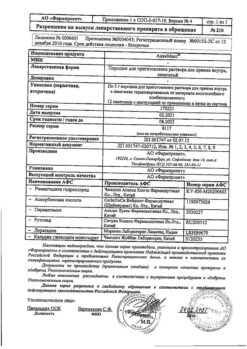
Ipraterol-aeronativ, aerosol 20 mcg/dose+50 mcg/dose 200 doses
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: combined bronchodilator (beta2-adrenomimetic selective + m-cholinoblocker).
ATX code: R03AL01
Pharmacological properties
Pharmacodynamics
The drug Ipraterol-aeronativ contains two components with bronchodilator activity: ipratropium bromide, a m-cholinoblocker, and fenoterol, a β2-adrenomimetic.
The bronchodilation by inhaled administration of ipratropium bromide is due primarily to local rather than systemic anticholinergic action.
Ipratropium bromide is a quaternary ammonium derivative with anticholinergic (parasympatholytic) properties. Ipratropium bromide inhibits vagus nerve reflexes. Anticholinergic agents prevent increased intracellular concentration of calcium ions, which occurs due to interaction of acetylcholine with muscarinic receptors of bronchial smooth muscles. The release of calcium ions is mediated by a system of secondary mediators, which include inositol triphosphate (ITP) and diacylglycerol (DAG).
In patients with bronchospasm associated with chronic obstructive pulmonary disease (chronic bronchitis and pulmonary emphysema), significant improvement in pulmonary function (increased forced expiratory volume per 1 second (PEF1) and peak expiratory velocity (PEF) by 15% or more) are observed within 15 minutes, the maximum effect is achieved in 1-2 hours and lasts in most patients up to 6 hours after administration.
Ipratropium bromide has no adverse effect on airway mucus secretion, mucociliary clearance and gas exchange.
Phenoterol selectively stimulates β2 adrenoreceptors at the therapeutic dose. Stimulation of β1-adrenoreceptors activates adenylate cyclase through stimulation of GS-protein. Stimulation of β1-adrenoreceptors occurs at high doses. Fenoterol relaxes the smooth muscles of the bronchi and vessels and counteracts the development of bronchospastic reactions due to the effects of histamine, methacholine, cold air and allergens (immediate-type hypersensitivity reactions). Immediately after use, fenoterol blocks the release of inflammatory mediators and bronchoobstruction from mast cells. In addition, when using fenoterol in doses of 0.6 mg, increased mucociliary clearance is noted.
The β2-adrenergic (stimulating β-adrenoreceptors) effects of the drug on cardiac activity, such as increased heart rate and force, are due to the vascular action of fenoterol, the stimulation of β2 adrenoreceptors of the heart and, when doses higher than therapeutic doses are used, by stimulation of β1-adrenoreceptors. As with other β-adrenergic drugs, prolongation of the QT intervalc when using high doses is noted. When using fenoterol with metered-dose aerosol inhalers (MDIs), this effect was inconsistent and was noted when doses higher than recommended were used. However, after using fenoterol with nebulizers (standard-dose inhalation solution in vials), the systemic effect may be higher than when using the drug with DAIs at the recommended doses. The clinical significance of these observations has not been established.
The most commonly observed effect of β-adrenoreceptor agonists is tremor. In contrast to the effects on bronchial smooth muscles, tolerance may develop to the systemic effects of β-adrenoreceptor agonists; the clinical significance of this phenomenon is unclear. Tremor is the most frequent undesirable effect of β-adrenoreceptor agonists. When these two active agents are used together, the bronchodilator effect is achieved by affecting different pharmacological targets. These substances complement each other, resulting in an increased antispasmodic effect on the bronchial muscles and a greater breadth of therapeutic action in bronchopulmonary diseases accompanied by airway constriction. The complementary effect is such that a lower dose of the β-adrenergic component is required to achieve the desired effect, which allows an individual selection of the effective dose with virtually no side effects.
In acute bronchoconstriction, the effect of the drug develops quickly, allowing it to be used in acute attacks of bronchospasm.
Pharmacokinetics
There is no evidence that the pharmacokinetics of the combination drug containing ipratropium bromide and fenoterol differ from that of each of the individual components.
Absorption
In the inhaled route of administration, ipratropium bromide is characterized by extremely low absorption from the respiratory mucosa. The plasma concentration of ipratropium bromide is at the lower limit of determination, and it can be measured only when high doses of the active substance are used. After inhalation, 10-30% of the administered dose of ipratropium bromide usually enters the lungs (depending on the dosage form and inhalation method). Most of the dose is swallowed and reaches the gastrointestinal tract.
The portion of the drug dose that enters the lungs quickly reaches the systemic bloodstream (within minutes). The total systemic bioavailability of ipratropium bromide administered by inhalation is 2% and 7-28%, respectively.
Depending on the method of inhalation and the inhalation system used, about 10-30% of the active substance reaches the lower airways, and the rest is deposited in the upper airways and swallowed. As a result, some amount of inhaled fenoterol enters the gastrointestinal tract. Absorption is biphasic – 30% of fenoterol is rapidly absorbed with a half-life (T1/2) of 11 minutes, and 70% is slowly absorbed with a T1/2 of 120 minutes. There is no correlation between the plasma concentrations of fenoterol achieved after inhalation and the pharmacodynamic time-effect curve. Long (3-5 hours) bronchodilator effect after inhalation, comparable with the corresponding effect achieved after intravenous administration, is not supported by high concentrations of the active substance in the systemic bloodstream. After oral administration, about 60% of fenoterol is absorbed. Time of reaching maximum concentration in blood plasma is 2 hours.
Distribution
Ipratropium bromide, which is a quaternary amine, is poorly soluble in fat and poorly penetrates through biological membranes. It does not cumulate. Ipratropium bromide binds to plasma proteins to a minimal extent (less than 20%). There are no data on the possibility of penetration of ipratropium bromide through the placental barrier and into the breast milk.
Phenoterol is intensively distributed throughout the organs and tissues. Binding with blood plasma proteins is 40-55%. Fenoterol unchanged passes through the placental barrier and is excreted with breast milk.
Metabolism
Ipratropium bromide is metabolized by oxidation mainly in the liver. Up to 8 metabolites of ipratropium bromide are known, which bind weakly to muscarinic receptors and are considered inactive.
Phenoterol is metabolized in the liver. After 24 hours, 60% of the intravenous dose and 35% of the oral dose are excreted in the urine. This fraction of fenoterol undergoes biotransformation due to the “primary passage” effect through the liver, as a result of which the bioavailability of the drug after oral administration drops to approximately 1.5%. This explains the fact that the swallowed amount of the drug has almost no effect on the plasma concentration of the active substance achieved after inhalation. Biotransformation of fenoterol in humans occurs mainly by conjugation with sulfates in the intestinal wall.
Elimation
Ipratropium bromide is excreted mainly through the intestine and also through the kidneys. About 25% is excreted unchanged, the rest is excreted as metabolites.
Phenoterol is excreted by the kidneys and with bile as inactive sulfate conjugates. When parenteral administration, phenoterol is excreted according to a three-phase model with half-lives of 0.42 minutes, 14.3 minutes and 3.2 hours.
Pharmacokinetics in selected patient groups
The pharmacokinetics of the combination drug containing ipratropium bromide and fenoterol have not been studied in patients with diabetes mellitus, elderly patients, children, or patients with hepatic or renal dysfunction.
.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
Active ingredients:
Ipratropium bromide monohydrate
0.021 mg
(in terms of ipratropium bromide
/p>
0.020 mg)
Phenoterol hydrobromide
0.050 mg
Excipients:
Ethanol absolute
15.300 mg
Limonic acid monohydrate
0.005 mg
/p>
Triethyl citrate
0.150 mg
Propellant R 134a
(1, 1, 1,2-tetrafluoroethane)
44.470 mg
How to take, the dosage
How to take, the dosage
The dose should be adjusted on an individual basis.
Unless otherwise advised by a physician, the following doses are recommended:
Adults and children over 6 years of age
Treatment of attacks
In most cases, two inhaled doses of aerosol are sufficient to relieve symptoms. If there is no relief of breathing within 5 minutes, an additional 2 inhalation doses may be used.
If there is no relief after 4 inhalation doses and additional inhalation doses are needed, seek medical attention immediately.
Intermittent and prolonged therapy
Ingest 1-2 inhalations per dose, up to 8 inhalations per day (average of 1-2 inhalations 3 times a day). In bronchial asthma the drug should be used only as needed. The drug Ipraterol-aeronativ in children should be used only by prescription and under adult supervision (see section “Special indications”).
Inhalation instructions
Patients should be instructed on the proper use of the metered dose aerosol.
Ipraterol Aeronativ is for inhaled use only.
Before using the inhaler for the first time or if the inhaler has not been used for a week or longer, check its operation. Remove the protective cap from the tip of the inhaler, shake the inhaler well and press the balloon down with one squirt of product in the air.
Step 1: Remove the protective cap from the tip of the inhaler as shown in Figure 1.
Phase 2: Shake the inhaler vigorously.
Step 3: Take a slow, full breath.
Step 4: Holding the balloon as shown in Figure 2, cup your lips tightly around the mouthpiece.
The balloon should be pointing one way up (figure 2).
Step 5: Take the deepest breath possible while quickly pressing on the bottom of the balloon until one inhalation dose is released.
Step 6: Hold your breath for a few seconds, then take the mouthpiece out of your mouth and slowly exhale.
Please put the protective cap on the tip of the inhaler.
Repeat steps 2-6 for the second inhalation dose, if necessary.
Clean the inhaler
Rinse the tip of the inhaler regularly (once a week) as shown in Figure 3.
Please remove the metal can from its plastic case and rinse
the case and the cap with warm water. Do not use hot water.
Dry thoroughly, but do not use a heating device. Put the can back in its case and replace the cap. Do not submerge a metal can in water.
The bottle has a capacity of 200 inhalations. You need to replace it after this.
The product should be supervised in children.
It is recommended that the child’s nostrils be clamped during inhalation to prevent nasal inhalation.
WARNING: The plastic mouthpiece is designed specifically for Ipraterol Aeronativ and is used for precise dosing of the product. The mouthpiece must not be used with other metered dose aerosols. You must also not use Ipraterol-aeronativ with any adapter other than the mouthpiece supplied with the product.
The contents of the cylinder are under pressure.
The cylinder must not be opened or heated above 50°C!
Interaction
Interaction
Long-term concomitant use of Ipraterol Aeronativ with other anticholinergic drugs is not recommended due to lack of data.
The concomitant use of other β-adrenomimetic and anticholinergic drugs, including systemic ones, and xanthine derivatives (e.g., theophylline) may increase the bronchodilator effect of ipraterol-aeronativ and lead to increased adverse reactions.
The bronchodilator effect of ipraterol-aeronativ may be significantly impaired if β-adrenoblockers are prescribed at the same time.
The hypokalemia associated with the use of β-adrenomimetics may be increased by concomitant administration of xanthine derivatives, glucocorticosteroids and diuretics. This fact should be paid special attention when treating patients with severe forms of obstructive airways diseases. Hypokalemia may lead to an increased risk of arrhythmias in patients receiving digoxin. In addition, hypoxia may increase the negative effect of hypokalemia on cardiac rhythm. In such cases, monitoring of plasma potassium concentration is recommended.
The β2-adrenergic drugs should be used with caution in patients who have received monoamine oxidase inhibitors and tricyclic antidepressants, because these drugs can increase the effect of β-adrenergic drugs.
Inhalation of general anesthetic agents such as halogenated hydrocarbon anesthetics (halothane, trichloroethylene, enflurane) may increase the adverse effects of β-adrenergic agents on the cardiovascular system.
The co-administration of the drug with cromoglycic acid and/or glucocorticosteroids increases the effectiveness of therapy.
Special Instructions
Special Instructions
In case of sudden rapid increase of dyspnea (difficulty in breathing), consult a physician immediately.
In children, the drug Ipraterol-aeronativ should be used only by prescription and under adult supervision. Use in children under 6 years of age is contraindicated due to the lack of experience of use.
Hypersensitivity
After application of Ipraterol-aeronativ immediate hypersensitivity reactions may occur, the signs of which in rare cases may include: urticaria, angioedema, rash, bronchospasm, oropharyngeal edema, anaphylactic shock.
Paradoxical bronchospasm
Ipraterol-aeronativ, like other inhaled medicines, may cause paradoxical bronchospasm that may be life-threatening. If paradoxical bronchospasm occurs, Ipraterol-aeronativ should be discontinued immediately and alternative therapy should be used.
Long-term use
In patients with bronchial asthma, Ipraterol-aeronativ should be used only as needed; in patients with mild COPD, symptomatic treatment may be preferable to regular use;
In patients with bronchial asthma, be aware of the need for anti-inflammatory therapy to control airway inflammation and the course of the disease.
The regular use of increasing doses of drugs containing β2-adrenomimetics, such as Ipraterol Aeronativ, to relieve bronchial obstruction may cause uncontrolled worsening of the disease course. If bronchial obstruction worsens, increasing the dose of β2-adrenomimetics, including Ipraterol-aeronativ, beyond that recommended for a long time is not only unreasonable, but also dangerous. To prevent a life-threatening worsening of the course of the disease, a review of the patient’s treatment plan and adequate anti-inflammatory therapy with inhaled glucocorticosteroids should be considered.
Other sympathomimetic bronchodilators should be administered concomitantly with Ipraterol Aeronativ under medical supervision only.
Gastrointestinal disorders
In patients with a history of cystic fibrosis, gastrointestinal motility disorders are possible.
Visual disorders
Ipraterol-aeronativ should be used with caution in patients predisposed to closed-angle glaucoma. There have been isolated reports of ocular complications (e.g., increased intraocular pressure, mydriasis, closed-angle glaucoma, eye pain) developing when inhaled ipratropium bromide (or ipratropium bromide combined with β2-adrenomimetics) enters the eye. Symptoms of acute closed angle glaucoma may include eye pain or discomfort, blurred vision, haloing around objects, and colored spots in front of the eyes, combined with corneal edema and eye redness due to conjunctival hyperemia. If any combination of these symptoms develops, the use of eye drops to reduce intraocular pressure and immediate consultation with a specialist is indicated. Patients should be instructed on the proper use of Ipraterol Aeronativ inhaled. It is recommended that the solution used with the nebulizer be inhaled through the mouthpiece to prevent eye contact. If a mouthpiece is not available, a mask that fits snugly over the face should be used. Patients with a predisposition to glaucoma should be especially careful to protect their eyes.
Systemic effects
. In conditions such as recent myocardial infarction, diabetes mellitus with inadequate glycemic control, severe organic heart and vascular disease, hyperthyroidism, pheochromocytoma, or urinary tract obstruction (such as in prostatic hyperplasia or bladder neck obstruction), Ipraterol Aeronativ should only be used after careful risk/benefit assessment, especially when using doses higher than recommended.
Impact on the cardiovascular system
Rare cases of myocardial ischemia have been reported when taking β2-adrenomimetics. Patients with concomitant serious heart disease (e.g., coronary heart disease, arrhythmias, or severe heart failure) who receive ipraterol aeronativ should be warned to seek medical attention if heart pain or other symptoms suggestive of worsening heart disease occur. Symptoms such as shortness of breath and chest pain should be noted, as they may be of cardiac or pulmonary etiology.
Hypokalemia
Hypokalemia may occur with the use of β2-adrenomimetics (see section on Overdose).
In athletes, the use of Ipraterol Aeronativ may lead to positive doping tests due to its presence in phenoterol.
Impact on the ability to drive and operate vehicles
There have been no studies of the effect of the combined preparation containing ipratropium bromide and fenoterol on the ability to drive vehicles and operate mechanisms. Since by using the drug development of such adverse reactions as dizziness, nervousness, tremor, eye accommodation disorder, mydriasis, and blurred vision is possible, caution should be exercised while driving vehicles and operating machinery as well as while performing other potentially dangerous activities requiring increased concentration and rapid psychomotor reactions.
Contraindications
Contraindications
– Hypersensitivity to fenoterol, ipratropium bromide (and other atropine-like drugs) and excipients included in the drug.
– Hypertrophic obstructive cardiomyopathy.
– Tachyarrhythmia.
– First trimester of pregnancy.
– Childhood under 6 years of age.
With caution
Ipraterol Aeronativ should be used with caution in patients with conditions such as closed-angle glaucoma, arterial hypertension, diabetes mellitus, recent myocardial infarction (within the last 3 months), heart and vascular disease such as chronic heart failure ischemic heart disease, arrhythmias, aortic stenosis, severe lesions of cerebral and peripheral arteries, hyperthyroidism, pheochromocytoma, prostatic hyperplasia, bladder cervical obstruction, cystic fibrosis, II and III trimesters of pregnancy, breast-feeding period. Ipraterol Aeronativ should be used with caution in children and adolescents aged 6 to 18 years.
Side effects
Side effects
Many of the undesired effects listed above may be due to the anticholinergic and β-adrenergic properties of Ipraterol Aeronativ. Use of Ipraterol-aeronativ, as with any inhalation therapy, may cause local irritation.
Frequency definition: very frequently ( > 1/10), frequently (1/100 to 1/10), infrequently (1/1000 to 1/100), rarely (1/10000 to 1/1000), very rarely ( < 1/10000), (including individual reports).
Immune system disorders: rare – hypersensitivity reactions, anaphylactic reactions (Quincke’s edema).
Metabolic and nutrition disorders: rare – hypokalemia.
Mental disorders: infrequent – nervousness; rare – anxiety, mental disorders (mental disorders).
Nervous system disorders: infrequent – headache, dizziness, tremor.
Visual system disorders: rare – glaucoma, increased intraocular pressure, accommodation disorders, mydriasis, blurred vision, eye pain, corneal edema, conjunctival hyperemia, appearance of a halo around objects and colored spots before eyes.
Chronic disorders: infrequent tachycardia, palpitations; rare arrhythmia, atrial fibrillation, supraventricular tachycardia, myocardial ischemia.
Respiratory system, chest and mediastinum disorders: frequently – cough; infrequently – pharyngitis, dysphonia; rarely – bronchospasm, pharyngeal irritation, pharyngeal edema, laryngospasm, paradoxical bronchospasm, dry throat.
Gastrointestinal tract disorders: infrequent – vomiting, dry mouth, nausea; rare – stomatitis, glossitis, gastrointestinal motility disorders, diarrhea, constipation, swelling of the mouth.
Skin and subcutaneous tissue disorders: rarely – hives, skin rash, itching, sweating.
Muscular and connective tissue disorders: rare – muscle weakness, myalgia (muscle pain), muscle spasm.
River and urinary tract disorders: rarely – urinary retention.
Laboratory and instrumental data: infrequent – increase of systolic blood pressure; rare – increase and decrease of diastolic blood pressure.
If any of the side effects listed in the instructions worsen, or if you notice any other side effects not listed in the instructions, tell your doctor.
Overdose
Overdose
Symptoms
The symptoms of overdose are usually associated with the action of fenoterol. Symptoms due to overstimulation of β-adrenoreceptors may occur. Tachycardia, palpitations, tremors, arterial hypertension or arterial hypotension, increased difference between systolic and diastolic blood pressure, increased pulse pressure, increased angina pains, arrhythmias and feeling of blood “rush” to the face, metabolic acidosis, hypokalemia, feeling of heaviness behind the chest, increased bronchoobstruction are most likely. Possible symptoms of ipratropium bromide overdose (such as dry mouth, impaired eye accommodation), given the wide therapeutic effect of the drug and local mode of administration, are usually mild and transient.
Treatment
Ipraterol Aeronativ should be stopped. Blood acid-base balance monitoring data should be taken into account. The prescription of sedative drugs, anxiolytic drugs (tranquilizers) is recommended, in severe cases – intensive therapy. As a specific antidote, β-adrenoblockers, preferably selective β1-adrenoblockers may be used. However, one should keep in mind the possible increase in bronchial obstruction under the influence of β-adrenoblockers and carefully select the dose for patients with bronchial asthma or chronic obstructive pulmonary disease due to the risk of severe bronchospasm, which may lead to death.
Pregnancy use
Pregnancy use
The data of preclinical studies and existing clinical experience with the combination of fenoterol and ipratropium bromide showed that the active substances included in the combined drug do not have a negative effect in pregnancy. The possibility of the inhibitory effect of fenoterol on uterine contractile activity should be taken into account. The drug Ipraterol-aeronativ is contraindicated in the first trimester of pregnancy (possible weakening of labor activity). Caution should be exercised when using ipraterol-aeronativ in the second and third trimesters of pregnancy.
Phenoterol penetrates into breast milk. No data confirming that ipratropium bromide penetrates into breast milk have been obtained. The safety of using the drug during breast-feeding has not been established. In this regard, the use of the drug Ipraterol-aeronativ during breast-feeding is possible only if the potential benefit to the mother exceeds the potential risk to the baby.
Similarities
Similarities
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In a light-protected place at a temperature not exceeding 25 °C, away from heating appliances. Do not freeze. Keep out of reach of children. |
| Manufacturer | Pharmstandard-Leksredstva, Russia |
| Medication form | metered aerosol for inhalation |
| Brand | Pharmstandard-Leksredstva |
Related products
Buy Ipraterol-aeronativ, aerosol 20 mcg/dose+50 mcg/dose 200 doses with delivery to USA, UK, Europe and over 120 other countries.