No products in the cart.
Hydroxychloroquine, 200 mg 30 pcs
€35.50 €29.59
Out of stock
(E-mail when Stock is available)
Description
Hydroxychloroquine has antimalarial properties and also has anti-inflammatory and immunosuppressive effects in chronic discoid or systemic lupus erythematosus (SLE), acute and chronic rheumatoid arthritis (RA). Its mechanism of action in malaria, lupus erythematosus and rheumatoid arthritis is not fully known.
Hydroxychloroquine has the properties of a moderate immunosuppressor, inhibiting the synthesis of rheumatoid factor and acute phase reaction components. It also accumulates in leukocytes, stabilizing lysosomal membranes, and inhibits the activity of many enzymes, including collagenase and proteases, which cause cartilage breakdown.
The efficacy in SLE and RA is associated with the following anti-inflammatory and immunomodulatory effects of hydroxychloroquine: increasing intracellular pH leads to slower antigenic response and reduces binding of peptides of the main histocompatibility complex (HCG) receptors. Fewer antigen-HCG receptors reach the cell surface, resulting in a reduced autoimmune response; decreased activity of phospholipase A2 at high concentrations, lysosomal enzymes; reduced concentrations of cytokines IL-1 and IL-6, leading to reduced clinical and laboratory parameters of autoimmune response. Since there is no disruption of interferon gamma synthesis, these effects may be associated with a selective effect on cytokines; inhibition of pre- and/or post-transcriptional DNA and RNA.
Hydroxychloroquine actively suppresses asexual erythrocytic forms as well as gametes of P. vivax and P. malariae, which disappear from the blood almost simultaneously with the asexual forms. Hydroxychloroquine has no effect on R. falciparum gametes. Hydroxychloroquine is ineffective against chloroquine-resistant strains of P. falciparum, and inactive against extra-erythrocytic forms of P. vivax, P. malariae and P. ovale, and therefore cannot prevent infection with these microorganisms when administered for prophylactic purposes, and cannot prevent relapse of the disease caused by these pathogens.
Pharmacokinetics
Hydroxychloroquine is rapidly and almost completely absorbed after oral administration. The binding to plasma proteins is 45%. Mean T1/2 from plasma varies with time since hydroxychloroquine administration as follows: 5.9 h (from reaching Cmax to 10 h), 26.1 h (10 to 48 h), and 299 h (48 to 504 h). In the liver, hydroxychloroquine is partially converted to active ethylated metabolites. Unchanged hydroxychloroquine and its metabolites are well distributed in the body. The volume of distribution is 5-10 l/kg. Hydroxychloroquine accumulates in tissues with high levels of metabolism (in the liver, kidneys, lungs, spleen – in these organs the concentration exceeds the plasma concentration by 200-700 times; CNS, red blood cells, leukocytes), as well as in the retina and melanin-rich tissues. Hydroxychloroquine and its metabolites are excreted mainly in the urine and to a lesser extent in the bile. Excretion of hydroxychloroquine is slow, the terminal T1/2 is about 50 days (from whole blood) and 32 days (from plasma). In 24 hours 3% of the administered dose of hydroxychloroquine is excreted in the urine. Hydroxychloroquine penetrates the placental barrier and is detected in small amounts in breast milk.
Indications
Indications
malaria (except for chloroquine-resistant strains of P. falciparum): prevention and relief of acute attacks of malaria caused by Plasmodium vivax, P. ovale and P. malariae, as well as sensitive strains of P. falciparum;
radical treatment of malaria caused by susceptible strains of P. falciparum;
rheumatoid arthritis;
juvenile rheumatoid arthritis;
lupus erythematosus (systemic and discoid);
photodermatitis.
Pharmacological effect
Pharmacological effect
Hydroxychloroquine has antimalarial properties, and also has anti-inflammatory and immunosuppressive effects in chronic discoid or systemic lupus erythematosus (SLE), acute and chronic rheumatoid arthritis (RA). The mechanism of its action in malaria, lupus erythematosus and rheumatoid arthritis is not completely known.
Hydroxychloroquine has the properties of a moderate immunosuppressant, inhibiting the synthesis of rheumatoid factor and components of the acute phase reaction. It also accumulates in leukocytes, stabilizing lysosomal membranes, and inhibits the activity of many enzymes, incl. collagenases and proteases, which cause cartilage breakdown.
Efficacy in SLE and RA is associated with the following anti-inflammatory and immunomodulatory effects of hydroxychloroquine: an increase in intracellular pH leads to a slowdown of the antigenic response and reduces the binding of peptides to the major histocompatibility complex (MHC) receptors. Fewer MHC antigen receptors reach the cell surface, resulting in a decreased autoimmune response; decreased activity of phospholipase A2 at high concentrations of lysosomal enzymes; a decrease in the concentrations of IL-1 and IL-6 cytokines, leading to a decrease in clinical and laboratory parameters of the autoimmune response. Since there is no disruption of interferon gamma synthesis, these effects may be due to selective effects on cytokines; inhibition of pre- and/or post-transcription of DNA and RNA.
Hydroxychloroquine actively suppresses asexual erythrocyte forms, as well as gametes of P. vivax and P. malariae, which disappear from the blood almost simultaneously with the asexual forms. Hydroxychloroquine has no effect on P. falciparum gametes. Hydroxychloroquine is ineffective against chloroquine-resistant strains of P. falciparum, and is also inactive against extra-erythrocytic forms of P. vivax, P. malariae and P. ovale, and therefore cannot prevent infection by these microorganisms when prescribed for prophylactic purposes, and also cannot prevent relapse of the disease caused by these pathogens.
Pharmacokinetics
After oral administration, hydroxychloroquine is rapidly and almost completely absorbed. Communication with plasma proteins – 45%. The mean plasma T1/2 value varies depending on the time elapsed after administration of hydroxychloroquine as follows: 5.9 hours (from Cmax to 10 hours), 26.1 hours (from 10 to 48 hours) and 299 hours (from 48 to 504 hours). In the liver, hydroxychloroquine is partially converted into active ethylated metabolites. Unchanged hydroxychloroquine and its metabolites are well distributed in the body. The volume of distribution is 5-10 l/kg. Hydroxychloroquine accumulates in tissues with a high level of metabolism (in the liver, kidneys, lungs, spleen – in these organs the concentration exceeds the plasma concentration by 200-700 times; central nervous system, erythrocytes, leukocytes), as well as in the retina and tissues rich in melanin. Hydroxychloroquine and its metabolites are excreted primarily in the urine and to a lesser extent in the bile. The elimination of hydroxychloroquine is slow, with a terminal T1/2 of about 50 days (from whole blood) and 32 days (from plasma). Within 24 hours, 3% of the administered dose of hydroxychloroquine is excreted in the urine. Hydroxychloroquine crosses the placental barrier and is found in small quantities in breast milk.
Special instructions
Special instructions
The retinal toxicity of hydroxychloroquine is largely dose dependent. The incidence of retinopathy when using doses up to 6.5 mg/kg of “ideal” body weight is small. Exceeding the recommended daily dose sharply increases the risk of developing retinopathy.
Before starting a long course of treatment with hydroxychloroquine, both eyes should be thoroughly examined. The examination should include determination of visual acuity, examination of the fundus, assessment of color vision and visual fields. During therapy, such examination should be carried out at least once every 6 months.
The examination should be carried out more frequently in the following situations: with a daily dose exceeding 6.5 mg/kg of “ideal” body weight (in patients with increased body weight, using absolute body weight to calculate the dose may lead to overdose); with renal failure; with a total dose of over 200 g; in elderly people; if the patient has a decrease in visual acuity of any severity before starting treatment.
If any visual disturbances occur (decreased visual acuity, changes in color vision), hydroxychloroquine should be discontinued immediately and the patient’s vision should be carefully monitored, since retinal changes (and visual disturbances) may progress even after discontinuation of hydroxychloroquine.
Cases of cardiomyopathy leading to heart failure have been reported in patients taking hydroxychloroquine. It has been shown that hydroxychloroquine can cause severe hypoglycemia (including loss of consciousness), which can be life-threatening in patients both taking and not taking hypoglycemic drugs. Patients taking hydroxychloroquine should be warned of the risk of hypoglycemia and associated clinical signs and symptoms. In patients who develop clinical symptoms suggestive of hypoglycemia during treatment with hydroxychloroquine, blood glucose concentrations should be determined and therapy reconsidered if necessary.
Caution is recommended when using hydroxychloroquine in patients with liver or kidney disease, who may require dose reductions, or in patients taking medications that may cause adverse effects on these organs.
In patients taking hydroxychloroquine for a long time, a complete blood count should be performed periodically (if hematological abnormalities occur, hydroxychloroquine should be discontinued).
Children are particularly sensitive to the toxic effects of 4-aminoquinolines, so care should be taken to keep hydroxychloroquine out of the reach of children.
All patients taking hydroxychloroquine for a long time should be periodically examined by a neurologist regarding skeletal muscle function and the severity of tendon reflexes. If muscle weakness occurs, hydroxychloroquine should be discontinued.
In very rare cases, suicidal behavior has been reported in patients taking hydroxychloroquine. When using hydroxychloroquine, extrapyramidal disorders may develop.
Hydroxychloroquine is not effective against chloroquine-resistant strains of P. falciparum, nor is it active against extraerythrocytic forms of P. vivax, P. malariae, and P. ovale, and therefore it cannot prevent infection by these microorganisms when used prophylactically, nor can it prevent relapse of the disease caused by these pathogens.
Impact on the ability to drive vehicles and machinery
During treatment with hydroxychloroquine, caution should be exercised when performing potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Hydroxychloroquine
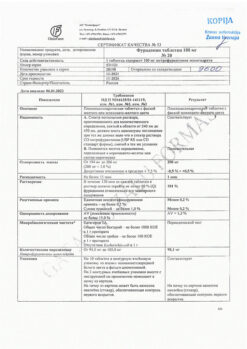
Composition
Composition
1 film-coated tablet contains:
active substance:
hydroxychloroquine sulfate – 200 mg;
excipients:
croscarmellose sodium – 3.0 mg,
magnesium stearate – 4.0 mg,
colloidal silicon dioxide – 0.5 mg,
microcrystalline cellulose (PH 102) – 92.5 mg;
film shell: hyprolose (hydroxypropylcellulose), LF – 2.4 mg, hypromelose 2910 (hydroxypropylmethylcellulose) – 0.6 mg, macrogol (polyethylene glycol) 8000 – 1.8 mg, titanium dioxide (E 171) – 2.4 mg.
Pregnancy
Pregnancy
Contraindicated for use during pregnancy.
If it is necessary to use it during breastfeeding, the ratio of the expected benefit of therapy for the mother and the potential risk for the infant should be carefully assessed, taking into account the indications for use and the duration of therapy.
Contraindications
Contraindications
Hypersensitivity to hydroxychloroquine and 4-aminoquinoline derivatives; retinopathy (including a history of maculopathy); children’s age when long-term therapy is necessary (children have an increased risk of developing toxic effects); children under 6 years of age (200 mg tablets are not intended for children with an “ideal” body weight of less than 31 kg); pregnancy.
With caution: in case of visual disorders (decreased visual acuity, impaired color vision, narrowing of visual fields), while taking drugs that can cause adverse ophthalmological reactions (danger of progression of retinopathy and visual disorders). For hematological diseases (including a history).
For neurological diseases, psychoses (including history).
For porphyria cutanea tarda (risk of exacerbation), psoriasis (risk of increased skin manifestations of the disease), while taking medications that can cause skin reactions.
In case of renal and/or liver failure, hepatitis, while taking drugs that can adversely affect liver and/or kidney function (in case of severe impairment of renal or liver function, the dose should be selected under the control of plasma concentrations of hydroxychloroquine). With deficiency of glucose-6-phosphate dehydrogenase.
For gastrointestinal diseases. In case of hypersensitivity to quinine (possibility of cross-allergic reactions).
In case of cardiac conduction disturbances (bundle branch block/AV block) and in case of hypertrophy of both ventricles. For cardiomyopathy.
With congenital or acquired prolongation of the QT interval and (or) a history of the following risk factors for prolongation of the QT interval: heart disease (for example, heart failure, myocardial infarction); proarrhythmic conditions (for example, bradycardia with a heart rate less than 50 beats/min); ventricular arrhythmias; uncorrected hypokalemia and (or) hypomagnesemia; simultaneous use of drugs that prolong the QT interval (increased risk of developing ventricular arrhythmias.
Due to the risk of hypoglycemia, hydroxychloroquine should be prescribed with caution to patients both taking and not taking hypoglycemic drugs.
Side Effects
Side Effects
From the hematopoietic system: frequency unknown – suppression of bone marrow hematopoiesis, anemia, aplastic anemia, agranulocytosis, leukopenia, thrombocytopenia.
From the immune system: frequency unknown – urticaria, angioedema, bronchospasm.
Metabolism: often – anorexia; frequency unknown – hypoglycemia, possible exacerbation of porphyria.
From the mental side: often – affective lability; infrequently – nervousness; frequency unknown – psychosis, suicidal behavior.
From the nervous system: often – headache; infrequently – dizziness; frequency unknown – seizures, extrapyramidal disorders such as muscular dystonia, dyskinesia and tremor.
On the part of the organ of vision: often – blurred vision associated with impaired accommodation, which is dose-dependent and reversible; uncommon – retinopathy with pigmentation changes and visual field defects. If hydrochloroquine is discontinued in a timely manner, these phenomena are reversible. If the condition remains undiagnosed and retinal lesions continue to develop, then there is a possible risk of their progression even after hydrochloroquine is discontinued. Retinal changes may initially be asymptomatic or manifest as paracentral or pericentral scotomas, transient scotomas, and color vision disturbances. Corneal changes may occur, including swelling and clouding. They may be asymptomatic or cause visual disturbances such as halos, blurred vision, or photophobia. These changes may be temporary or reversible. Frequency unknown – maculopathy and macular degeneration, which may be irreversible.
From the organ of hearing and labyrinthine disorders: infrequently – vertigo, tinnitus; frequency unknown – hearing loss.
From the cardiovascular system: frequency unknown – prolongation of the QT interval in patients with risk factors, which can lead to the development of heart rhythm disturbances (ventricular arrhythmia of the “pirouette” type, ventricular tachycardia), cardiomyopathy, which can lead to heart failure and, in some cases, death. Detection of cardiac conduction abnormalities (such as bundle branch blocks/AV conduction defects) and biventricular hypertrophy may indicate chronic cardiac toxicity. When hydrochloroquine is discontinued, these changes may reverse.
From the digestive system: very often – abdominal pain, nausea; often – diarrhea, vomiting. These symptoms usually resolve immediately after reducing the dose or stopping hydrochloroquine.
From the liver and biliary tract: infrequently – deviations from the norm in liver function tests; frequency unknown – fulminant liver failure.
From the skin of subcutaneous tissues: often – skin rash, itching; uncommon – changes in pigmentation of the skin and mucous membranes, hair bleaching and alopecia (these changes usually disappear quickly after cessation of treatment); frequency unknown – bullous rash including erythema multiforme; Stevens-Johnson syndrome; toxic epidermal necrolysis; photosensitivity; exfoliative dermatitis; drug skin reaction accompanied by eosinophilia and systemic manifestations (DRESS syndrome); acute generalized exanthematous pustulosis (AGEP). OHEP must be distinguished from psoriasis, although hydroxychloroquine may exacerbate psoriasis. OHEP may be accompanied by fever and hyperleukocytosis. After discontinuation of hydrochloroquine, the outcome is usually favorable.
From the musculoskeletal system: infrequently – sensory-motor disorders; frequency unknown – skeletal muscle myopathy or neuromyopathy leading to progressive weakness and atrophy of proximal muscle groups (myopathy may be reversible after discontinuation of hydrochloroquine, but full recovery may take several months), suppression of tendon reflexes and decreased nerve conduction.
Interaction
Interaction
Caution should be exercised when prescribing hydroxychloroquine to patients receiving drugs known to prolong the QT interval (eg, Class IA and III antiarrhythmics, tricyclic antidepressants, antipsychotics, certain antimicrobials [eg, moxifloxacin]) due to an increased risk of developing ventricular arrhythmias.
There are reports that hydroxychloroquine is able to increase plasma concentrations of digoxin, therefore, in order to avoid the development of glycoside intoxication during their simultaneous use, it is necessary to reduce the dose of digoxin – under the control of its concentration in plasma.
Hydroxychloroquine may potentiate the effects of insulin and oral hypoglycemic agents; dosages of these drugs may need to be reduced when initiating hydroxychloroquine.
Antacids may reduce the absorption of hydroxychloroquine. Therefore, when using antacids and hydroxychloroquine simultaneously, the interval between their doses should be at least 4 hours.
Hydroxychloroquine also has the following interactions with other drugs that have been described for chloroquine but have not yet been observed with hydroxychloroquine.
With aminoglycosides – potentiation of the direct blocking effect of aminoglycosides on neuromuscular transmission.
With cimetidine – cimetidine inhibits the metabolism of antimalarial drugs, which can lead to an increase in their plasma concentrations and increase the risk of developing their side effects, especially toxic ones.
With neostigmine and pyridostigmine – antagonism of action.
With any intradermal human diploid cell rabies vaccine – a decrease in the formation of antibodies in response to primary immunization with this vaccine.
With arrhythmogenic drugs – there is an increased risk of developing ventricular arrhythmia when chloroquine is used concomitantly with other arrhythmogenic drugs (such as amiodarone and moxifloxacin).
Halofantrine prolongs the QT interval and, in combination with chloroquine, may cause arrhythmias (this combination is not recommended).
With other antimalarial drugs that lower the seizure threshold, the use of chloroquine may lead to a decrease in the seizure threshold. Concomitant use of chloroquine with other known antimalarials that lower the seizure threshold (eg, mefloquine) may increase the risk of seizures.
With cyclosporine – there are reports of an increase in the concentration of cyclosporine in the blood plasma when cyclosporine and chloroquine are used together.
With antiepileptic drugs – when chloroquine is used together, the effectiveness of antiepileptic drugs may be insufficient.
With praziquantel – In an interaction study between chloroquine and praziquantel, a decrease in the bioavailability of praziquantel was reported. Due to the similarities in structure and pharmacokinetic parameters between hydroxychloroquine and chloroquine, a similar effect can be expected when hydroxychloroquine and praziquantel are coadministered.
With agalsidase – There is a theoretical risk of inhibition of intracellular α-galactosidase when hydroxychloroquine is coadministered with agalsidase.
Manufacturer
Manufacturer
Nanolek/Merck, Russia
Additional information
| Manufacturer | Nanolek/Merk, Russia |
|---|---|
| Medication form | pills |
| Brand | Nanolek/Merk |
Other forms…
Related products
Buy Hydroxychloroquine, 200 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.