No products in the cart.
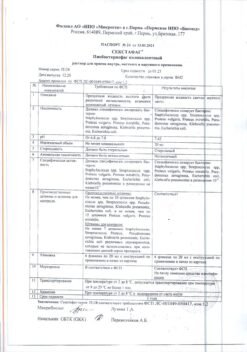
Hilaris, lyophilizate 150 mg
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: Immunodepressant – monoclonal antibodies to interleukin-1β.
ATX code: L04AC08.
Pharmacological properties
Mechanism of action
Kanakinumab is a human monoclonal IgGl/kappa isotype antibody to interleukin-1β (IL-1β). Canakinumab binds with high affinity to human IL-1β, thus neutralizing its biological effect by blocking the interaction of IL-1β with its receptors, IL-1β-induced gene activation and production of inflammatory mediators such as IL-6 and cyclooxygenase-2. Thus, canakinumab is suitable for the correction of diseases and conditions characterized by hyperproduction of IL-1β at the local or systemic level.
Pharmacodynamics
The overproduction of IL-1β in inflammatory diseases can lead to local or systemic inflammation, excessive production of C-reactive protein (CRP) or serum amyloid A (SAA) and fever.
Cryopyrin-associated periodic syndrome (CAPS)Patients with various CAPS phenotypes, including familial cold
Familial Cold Autoinflammatory Syndrome/ Familial Cold Urticaria (FCAS/FCU), Muckle-Wells Syndrome, MWS) and Neonatal onset multisystemic inflammatory disease/Chronic infantile neurological cutaneous and articular syndrome, NOMID/C1NCA), with excessive uncontrolled IL-1β production (manifested by fever, increased fatigue, skin rash, arthritis, pronounced leukocytosis, high platelet count, and increased CRP concentration), a rapid response to canakinumab therapy was observed. On treatment with the drug, phenomena such as elevated concentration of CRP, CAA, leukocytosis and increased platelet count quickly returned to normal levels.
Still disease in adults and juvenile arthritis with systemic onset (systemic juvenile idiopathic arthritis, sJIA, ILAR classification, International League of Rheumatology Associations)Adult Still disease and sJIA are severe autoinflammatory diseases that are caused by innate immunity through proinflammatory cytokines, a key one being IL-1β.
The common manifestations of adult Still’s disease and SSIA include fever, skin rash, hepatosplenomegaly, lymphadenopathy, polyserositis and arthritis. Treatment with the drug in most of these patients resulted in rapid and sustained improvement in the joint and systemic manifestations of SJIA with a significant reduction in the number of inflamed joints, rapid resolution of fever, and a decrease in the concentration of acute phase reactants.
Gouty arthritis
The exacerbation of gouty arthritis is due to activation of tissue macrophages and simultaneous hyperproduction of IL-1β, which leads to an acute inflammatory response with a pronounced pain syndrome. The production of IL-1β is provoked by the deposition of crystals of uric acid salts (monosodium urate monohydrate) in the joints and surrounding tissues, which leads to the activation of “NALP3-inflamosome” complexes. Innate immune activators such as endogenous toll-like receptor agonists may also contribute to the activation of IL-1β gene transcription, initiating gouty arthritis exacerbation. After canakinumab therapy, within a short time there is a decrease in the concentration of laboratory markers of inflammation (CRP, CAA), and signs of inflammation of the affected joint (pain, swelling, redness) disappear.
Pharmacokinetics
Intake
In adult patients with different CAPS phenotypes, after a single subcutaneous (p/k) injection of 150 mg of canakinumab, the time to reach maximum concentration (Cmax) is about 7 days. The average final elimination half-life is 26 days. When canakinumab is administered b/c the absolute bioavailability is 66% (population pharmacokinetic analysis in patients with CAPS, including children aged 2 years and older). Pharmacokinetic parameters (area under the concentration-time curve (AUC) and Cmax) increase in proportion to dose in the dose range from 0.30 to 10.0 mg/kg by intravenous (w/v) infusion or by p/q administration (at a dose of 150 to 600 mg).
Distribution
Canakinumab binds to serum IL-1β. The volume of distribution (Vss) varies with body weight.
In patients with CAPS, Vss is 6.2 L at a body weight of 70 kg, 5.0 L in patients with periodic fever syndrome (TRAPS, H1DS/MKD, FMF) with a body weight of 55 kg, in patients with SSIA, 3.2 L at a body weight of 33 kg and in patients with gouty arthritis, 7.9 L at a body weight of 93 kg. When administered by mouth for 6 months at a dose of 150 mg every 8 weeks, at a dose of 4 mg/kg every 4 weeks, and 150 mg every 12 weeks, canakinumab has a cumulation factor of 1.3, 1.6 and 1.1, respectively.
Elevation
The clearance (C1) varies with body weight. For patients with CAPS, this figure is 0.17 L/d at a body weight of 70 kg, 0.14 L/d in patients with periodic fever syndrome (TRAPS, HIDS/MKD, FMF) at a body weight of 55 kg, 0.11 L/d in patients with SSIA at a body weight of 33 kg, and 0.23 L/d in patients with gouty arthritis at a body weight of 93 kg. After accounting for weight differences, no significant difference in pharmacokinetic properties of canakinumab was found in patients with gouty arthritis, different CAPS, TRAPS, HIDS/MKD, FMF and cSIA phenotypes. No increase in C1 or changes in any other time-dependent pharmacokinetic parameters of canakinumab were observed with repeated administration of the drug. No age- or sex-dependent changes in pharmacokinetic parameters were observed after dose adjustment by body weight.
Pharmacokinetics in Special Clinical Cases
Patients less than 18 years of age
In patients 4 years of age and older, after a single p/c administration of the drug at a dose of 150 mg or 2 mg/kg once, the time to reach Cmax of canakinumab is 2-7 days.
The terminal elimination half-life of canakinumab in these patients is similar to that in adults: 22.9 to 25.7 days.
The pharmacokinetic parameters of canakinumab in children with CAPS aged 2 to 4 years are similar to those in patients 4 years and older, according to a population-based pharmacokinetic modeling analysis. Additional pharmacokinetic analysis showed that the pharmacokinetic parameters of cancanakinumab in 6 children with CAPS younger than 2 years of age were similar to those in children older than 2 years of age. Pharmacokinetic characteristics were similar in patients with CAPS, TRAPS, HIDS/MKD, FMF, and cSIA. When canakinumab was administered by mouth at a dose of 4 mg/kg every 4 weeks, AUC and Cmax values were similar in patients with SSIA in the 2 to 20 year age group.
According to population pharmacokinetic modeling analysis, the pharmacokinetic parameters of canakinumab in patients with SLEA aged 16 to 20 years and those younger than 16 years were similar. In patients with SSIA over and under 20 years of age, the calculated exposure of canakinumab at equilibrium at a dose value of 4 mg/kg (300 mg maximum) was comparable.
In patients with periodic fever syndrome (TRAPS, HIDS/MKD, FMF), exposure at minimal plasma concentrations of canakinumab at a 2 mg/kg p/kg dose every 4 weeks was comparable in age groups in patients aged 2 to 20 years.
Patients over 65 years of age
There was no difference in pharmacokinetic parameters based on C1 and Vss in patients in the older age group and patients less than 65 years of age.
Indications
Indications
Outoinflammatory periodic fever syndromes:
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
In patients with autoinflammatory periodic fever syndromes (CAPS, TRAPS, HIDS/MKD, FMF), and Still’s disease, including cSIA, therapy with Hilaris® may be initiated and administered only under the supervision of a physician experienced in the diagnosis and treatment of the respective diseases. After training in solution preparation techniques, selection of syringes and needles suitable for injection, and injection technique, patients with the above diseases or their caregivers may selfadminister the drug under proper supervision (if deemed necessary by the physician).
In patients with gouty arthritis, therapy with Hilaris® may only be initiated and performed under the supervision of a physician experienced in the use of biologic drugs; only a healthcare professional should administer the drug.
The drug is administered by injection, selecting areas of the body with pronounced subcutaneous tissue, such as the anterior surface of the abdomen, the anterior surface of the upper thigh, the outer surface of the upper arm or the buttocks (see section “Directions for Use”). To avoid painful sensations, the injection site should be changed for each subsequent injection. Avoid injecting in areas where there is damage to the skin, bruising or a rash. Injection into scar tissue should be avoided because of possible reduction of canakinumab exposure.
Each vial of Hilaris® is designed to be used as a single dose for a single patient.
Cryopyrin-associated periodic syndrome (CAPS)
The recommended starting doses of Ilaris® for patients with cryopyrin-associated periodic syndrome are listed in Table 1. 1
Table 1 Recommended starting doses of Ilaris® for patients with cryopyrin-associated periodic syndrome
The drug is administered by injection, 1 injection at 8-week intervals.
If the starting dose of 150 mg or 2 mg/kg does not give satisfactory clinical response, i.e. if the process of rash and other inflammatory symptoms resolution is not observed within 7 days after the first injection of Ilaris® , the second injection of the drug in dose of 150 mg (if body weight >40 kg) or 2 mg/kg (if body weight â¥15 kg and â¤40 kg) can be given. In case of further complete clinical response it is recommended to give maintenance therapy with Ilaris® preparation in dose 300 mg 1 injection with 8 weeks interval (if body weight >40 kg) or 4 mg/kg 1 injection with 8 weeks interval (if body weight â¥15 kg and â¤40 kg).
If satisfactory clinical effect is not observed within 7 days after increasing the dose, a third injection of Ilaris® may be given at a dose of 300 mg (at body weight >40 kg) or 4 mg/kg (at body weight â¥15 kg and â¤40 kg).
In case these patients achieve complete clinical response in further treatment it is recommended to provide maintenance therapy with Ilaris® in dose of 600 mg 1 injection with 8 weeks interval (for body weight >40 kg) or 8 mg/kg (for body weight â¥15 kg and â¤40 kg) 1 injection with 8 weeks interval on the basis of individual clinical evaluation.
If at the starting dose of 4 mg/kg satisfactory clinical effect is not observed within 7 days after the first injection, the second injection of Ilaris® at the dose of 4 mg/kg is possible. If full clinical response is subsequently achieved in these patients, maintenance therapy at a dose of 8 mg/kg 1 injection at 8-week intervals should be considered based on individual clinical evaluation.
The dose selection algorithm for adults and children over 4 years of age with a body weight â¥15 kg is shown in Figure 1, and for children 2 to 4 years of age with a body weight â¥7.5 kg <15 kg is shown in Figure 2.
Clinical experience with the drug at dosing intervals less than 4 weeks or at doses greater than 600 mg or 8 mg/kg is limited.
Tumor necrosis factor receptor associated syndrome (TRAPS), hyper-IgD syndrome/mevalonate kinase deficiency syndrome (HIDS/MKD), familial Mediterranean fever (FMF)
The recommended starting dose of the drug in adults and children 2 years and older is:
– 150 mg in patients with a body weight of >40 kg;
– 2 mg/kg in patients with a body weight of â¥7.5 kg and â¤40 kg.
The drug is administered as a pelvic injection every 4 weeks.
If there is no satisfactory clinical response within 7 days after the first injection of Ilaris® the second injection of the drug at a dose of 150 mg (for body mass of >40 kg) or 2 mg/kg (for body weight â¥7.5 kg and â¤40 kg) may be given. In case of further complete clinical response it is recommended to give maintenance therapy with Ilaris® in dose of 300 mg or 4 mg/kg every 4 weeks as a p/u injection.
The continuation of therapy with the drug in patients without clinical improvement should be reconsidered by the treating physician.
Still disease (Still’s disease in adults and SSIA in patients older than 2 years)
The recommended dose in patients with a body weight â¥7.5 kg is 4 mg/kg (maximum up to 300 mg) every 4 weeks as a p/week injection. Continuation of therapy with the drug in patients without clinical improvement should be reconsidered by the attending physician.
Gouty arthritis
The control and optimization of hyperuricemia should be done with appropriate antipodagric agents.
The drug Hilaris® should be used for therapy of exacerbations of gouty arthritis as needed.
The recommended dose of the drug in adults is 150 mg, the drug is given once daily by injection during an attack of gouty arthritis. For maximum effectiveness, the drug should be administered as soon as possible after the onset of an attack of gouty arthritis.
Patients with no therapeutic response to the first injection should not receive the drug again. In patients with a positive response to therapy with the drug, if continuation of treatment is necessary, reintroduction of the drug is possible no earlier than 12 weeks after the previous injection.
Patient Use in Special Patient Groups
Patients over 65 years of age
There is no need to adjust the dose of the drug in patients over 65 years of age.
Patients less than 18 years of age
There are no data on the use of Hilaris® for the treatment of gouty arthritis in children and adolescents less than 18 years of age.
Experience with canakinumab in children younger than 2 years of age is limited in the indications cryopyrin-associated periodic syndrome (CAPS), tumor necrosis factor receptor-associated periodic syndrome (TRAPS), hyper-IgD syndrome/mevalonate kinase deficiency syndrome (HIDS/MKD), familial Mediterranean fever (FMF), available data are listed under “Pharmacological properties” and “Side effects,” but no dosing recommendations are available. There are no data on the efficacy and safety of canakinumab in patients with SSRIs younger than 2 years of age.
Patients with impaired renal function
There is no need to adjust the dose of the drug in patients with impaired renal function (experience with clinical use in these patients is limited).
Patients with impaired liver function
The efficacy and safety of the drug have not been studied in patients with impaired liver function. Because canakinumab is human IgG, impaired liver function is not expected to affect its pharmacokinetics.
Interaction
Interaction
Special Instructions
Special Instructions
Experience with Hilaris® in patients with CAPS without an established mutation in the NLRP3 gene is limited.
Neutropenia and leukopenia
The development of neutropenia (absolute neutrophil count below 1.5Ã109/l) and leukopenia has been reported during therapy with IL-1 inhibitors, including Ilaris®. Do not start treatment with the drug in patients with neutropenia or leukopenia. Before initiation of therapy with the drug, white blood cell count including neutrophils should be determined and these values should be assessed again in 1-2 months. In case of prolonged or repeated therapy, these values should be periodically monitored during treatment. If absolute neutrophil and leukocyte counts decrease during therapy with the drug, proper control of the patient’s condition should be ensured and, if necessary, discontinuation of treatment with the drug should be considered.
Malignant neoplasms
There have been reports of malignancies in patients treated with Hilaris®, but the risk of malignancy with antibody binding IL-1 therapy is unknown.
Infectious diseases
Ilaris® use may be accompanied by increased incidence of serious infections, therefore a patient should be closely monitored for symptoms of infection during and after therapy with the drug. Caution should be exercised when using the drug in patients with infections, recurrent infectious diseases in the anamnesis or concomitant diseases predisposing to the development of infections. In CAPS, TRAPS, HIDS/MKB, FMF and Still’s disease, treatment with Hilaris® should not be started or continued in patients with an active infection requiring medical intervention. In patients with gouty arthritis, therapy with the drug should not be started during the active period of infection. The drug should not be used concomitantly with TNF inhibitors, since this may increase the risk of serious infections.
When using the drug Hilaris® there have been isolated cases of opportunistic infections (including aspergillosis, atypical infectious diseases of mycobacterial etiology, shingles). A causal relationship between these events and the use of the drug cannot be excluded.
About 12% of patients with different CAPS phenotypes had positive tuberculin test results without any evidence of tuberculosis infection (latent or active) when using the drug. There are no data on increased risk of reactivation of TB infection with treatment with monoclonal antibodies to IL-1 (e.g., Hilaris®).
Before initiating treatment with Ilaris® all patients should be evaluated to detect active or latent tuberculosis infection (including history taking and appropriate screening tests such as tuberculin test, IGRA (Interferon-Gamma-Release-Assay) or chest radiologic examination. During and after treatment with the drug, the patient’s condition should be closely monitored in order to detect tuberculosis infection. The patient should be informed about the necessity to consult a physician in case of the following symptoms during and after treatment with Ilaris® – prolonged cough, weight loss, subfebrile fever. In case of conversion of tuberculin test from negative to positive, especially in high-risk patients, alternative screening tests should be performed. In case of detection of tuberculosis infection the treatment by Ilaris® should not be started or continued.
Macrophage activation syndrome in adult patients with Still’s disease and cSIA
Macrophage activation syndrome is a known life-threatening condition that can develop in patients with rheumatic diseases, particularly patients with Still’s disease, and requires intensive therapy. The physician should be alert to symptoms of infection or worsening of the course of the disease, known to be a trigger for macrophage activation syndrome. Clinical trial data indicate that Hilaris® likely does not increase the risk of macrophage activation syndrome in patients with SJIA, but no definitive conclusions can be drawn.
Hypersensitivity reactions
Hypersensitivity reactions have been reported with Ilaris®. In most cases these reactions were expressed in a mild degree. No anaphylactoid or anaphylactic reactions were observed during the use of the drug. However, when using the drug Hilaris® one cannot exclude the risk of severe hypersensitivity reactions, which may occur when injecting drugs of protein origin.
Hepatic disorders
In clinical trials transient increase of liver transaminases activity or bilirubin concentration was noted.
Patients who have vertigo while taking the drug Ilaris® should abstain from driving vehicles or operating machinery until the undesired phenomenon has completely disappeared.
Contraindications
Contraindications
The drug should be used with caution in elderly patients; in patients with recurrent infections or any history of conditions predisposing to the development of infections.
Side effects
Side effects
Infectious and parasitic diseases: very common – infections, in particular, nasopharyngitis, sinusitis (viral), upper respiratory tract infections, bronchitis, influenza, urinary tract infections, gastroenteritis, panniculitis, pneumonia, pharyngitis, ear infections.
Nervous system disorders: often – dizziness/vertigo.
Muscular system disorders: often – back pain.
Hematopoietic system: frequently – thrombocytopenia, leukopenia; infrequently – neutropenia.
Metabolism: common – dyslipidemia; transient increase of uric acid concentration is possible.
Hearing organ and labyrinth disorders: often – dizziness.
The digestive system: frequently – vomiting; infrequently – gastroesophageal reflux disease; in some cases during the drug therapy in patients with CAPS a slight asymptomatic increase of bilirubin in serum without increasing liver transaminase activity has been noted.
Hepatic and biliary tract disorders: often – increased bilirubin level, increased ACT activity.
Allergic reactions: the development of anaphylactoid or anaphylactic reactions has not been observed; however, the risk of severe hypersensitivity reactions which may be observed when injecting the drugs of protein origin cannot be excluded.
Immunological reactions: 1%, antibodies to canakinumab were detected in patients receiving canakinumab for gouty arthritis; these antibodies were not detected in patients with CAPS.
General reactions: infrequent – general weakness.
Local reactions: frequent – reaction at the injection site.
Overdose
Overdose
Pregnancy use
Pregnancy use
Additional information
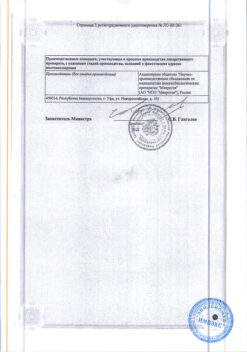
| Shelf life | 3 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | Store in the dark place at the temperature from 2 to 8 °С. Do not freeze. Store in the original carton package. The drug should be kept out of reach of children. |
| Manufacturer | Novartis Pharma Stein AG, Switzerland |
| Medication form | lyophilizate |
| Brand | Novartis Pharma Stein AG |
Related products
Buy Hilaris, lyophilizate 150 mg with delivery to USA, UK, Europe and over 120 other countries.