No products in the cart.
Description
Pharmacodynamics
Trastuzumab is a recombinant DNA-derived humanized monoclonal antibody that selectively interacts with the extracellular domain of human epidermal growth factor receptor type 2 (HER2). These antibodies are IgG1 antibodies consisting of human regions (constant heavy chain sites) and determinant complementary murine p185 HER2 antibody sites to HER2.
The proto-oncogene HER2 or c-erB2 encodes a transmembrane receptor-like protein with a molecular weight of 185 kDa that is structurally similar to other members of the epidermal growth factor receptor family. Hyperexpression of HER2 is detected in the tissue of primary breast cancer (BC) in 25-30% of patients and in the tissue of advanced gastric cancer in 6.8-42.6% of patients. Amplification of the HER2 gene leads to overexpression of the HER2 protein on the membrane of tumor cells, which in turn causes continuous activation of the HER2 receptor.
Studies show that breast cancer patients with amplification or overexpression of HER2 in tumor tissue have a lower survival rate without evidence of disease compared to patients without amplification or overexpression of HER2 in tumor tissue.
Trastuzumab blocks the proliferation of human tumor cells with HER2 hyperexpression in vivo and in vitro. In vitro antibody-dependent cellular cytotoxicity of trastuzumab predominantly targets tumor cells with HER2 hyperexpression.
Immunogenicity
An antibody to trastuzumab was detected in one of 903 women with breast cancer who received the drug as monotherapy or in combination with chemotherapy, and she was not allergic to Herceptin®.
There are no data on immunogenicity in the use of Herceptin® for the treatment of gastric cancer.
Pharmacokinetics
The pharmacokinetics of trastuzumab have been studied in patients with metastatic and early-stage cancer and in patients with advanced gastric cancer. No special studies on the study of interdrug interactions have been conducted.
Breast cancer
The pharmacokinetics were nonlinear when the drug was administered as short IV infusions at doses of 10, 50, 100, 250 and 500 mg once a week. The clearance of the drug decreased with increasing dose.
The elimination half-life (T1/2)
T1/2 is 28-38 days, hence the elimination period after drug withdrawal is up to 27 weeks (190 days or 5 half-lives).
The pharmacokinetics of trastuzumab on equilibrium.
The equilibrium state should be reached after approximately 25 weeks. Using a population-based pharmacokinetic method (two-chamber model, model-dependent analysis) to evaluate data from phase I, phase II, and phase III studies in metastatic breast cancer, the median expected AUC at equilibrium after 3 weeks was 1677 mg×day/L after administration of 3 doses (2 mg/kg) weekly and 1793 mg×day/L when administered after 3 weeks at a dose of 6 mg/kg. The calculated medians of Cmax were 104 mg/L and 189 mg/L, and Cmin were 64.9 mg/L and 47.3 mg/L, respectively. Using a model-independent or “non-compartmental” method of analysis (pop-compartmental analysis, NCA), the average Cmin in equilibrium by cycle 13 (week 37) was 63 mg/L in patients with early-stage BCM who received trastuzumab at a loading dose of 8 mg/kg, then at a maintenance dose of 6 mg/kg, after 3 weeks, and was comparable to that in patients with mRMJ who received trastuzumab weekly.
Clearance
The typical clearance of trastuzumab (for a patient with a body weight of 68 kg) was 0.241 L/day.
The volume of distribution
In all clinical studies, the central chamber (Vc) volume of distribution was 3.02 L and the peripheral chamber (Vp) was 2.68 L for a typical patient.
The circulating extracellular domain of the HER2-receptor (“sloughing” from the cell antigen)
The circulating extracellular domain of the HER2-receptor (“sloughing” from the cell antigen) was detected in the serum of some patients with breast cancer and HER2 hyperexpression. In 64% of the patients examined, the “sloughing off” antigen was detected in baseline serum samples at a concentration as high as 1880 ng/ml (median, 11 ng/ml). Patients who had high levels of the sloughing off cell antigen probably could have had a lower Cmin. However, the majority of patients with elevated sloughing off-cell antigen levels reached their target serum trastuzumab concentration by 6 weeks when the drug was administered weekly. There was no significant association between baseline cell-derived antigen levels and clinical response.
Disseminated gastric cancer
. Pharmacokinetics of trastuzumab at equilibrium state To assess the pharmacokinetics of trastuzumab at equilibrium state in patients with advanced gastric cancer after administration of trastuzumab at a loading dose of 8 mg/kg, followed by administration of 6 mg/kg every 3 weeks, a nonlinear two-chamber population pharmacokinetic method was used using data from a phase III study.
The observed levels of trastuzumab serum concentrations were lower, thus finding that the overall clearance of the drug was higher in patients with advanced gastric cancer than in breast cancer patients receiving trastuzumab at the same dose. The reason for this is unknown.
At high concentrations, total clearance is predominantly linear, and T1/2 is about 26 days.
The median estimated AUC (at equilibrium over a 3 week period) is 1213 mg×day/L, the median Cmax at equilibrium is 132 mg/L, and the median Cmin is 27.6 mg/L.
There are no data on circulating extracellular domain levels of the HER2 receptor (“sloughing off” antigen from the cell) in the serum of patients with gastric cancer.
Pharmacokinetics in special patient groups
Separate pharmacokinetic studies have not been performed in elderly patients and patients with renal or hepatic impairment. Age has no effect on the distribution of trastuzumab.
Indications
Indications
Breast cancer
Metastatic breast cancer with tumor overexpression of HER2:
as monotherapy, after one or more chemotherapy regimens;
in combination with paclitaxel or docetaxel, in the absence of previous chemotherapy (first line of therapy);
in combination with aromatase inhibitors for positive hormonal receptors (estrogen and/or progesterone) in postmenopausal women.
Early stages of breast cancer with tumor overexpression of HER2:
in the form of adjuvant therapy after surgery, completion of chemotherapy (neoadjuvant or adjuvant) and radiation therapy;
in combination with paclitaxel or docetaxel after adjuvant chemotherapy with doxorubicin and cyclophosphamide;
in combination with adjuvant chemotherapy consisting of docetaxel and carboplatin;
in combination with neoadjuvant chemotherapy followed by adjuvant monotherapy with Herceptin® for locally advanced (including inflammatory) disease or in cases where the tumor size exceeds 2 cm in diameter.
Advanced stomach cancer
Advanced adenocarcinoma of the stomach or gastroesophageal junction with tumor overexpression of HER2:
in combination with capecitabine or intravenous fluorouracil and platinum in the absence of previous antitumor therapy for metastatic disease.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Trastuzumab is a recombinant DNA-derived humanized monoclonal antibody that selectively interacts with the extracellular domain of human epidermal growth factor receptor type 2 (HER2). These antibodies are IgG1, consisting of human regions (heavy chain constant regions) and determining the complementarity of the murine p185 HER2 antibody to HER2.
The proto-oncogene HER2 or c-erB2 encodes a transmembrane receptor-like protein with a molecular weight of 185 kDa, which is structurally similar to other members of the epidermal growth factor receptor family. Overexpression of HER2 is found in the tissue of primary breast cancer (BC) in 25-30% of patients and in the tissue of advanced gastric cancer in 6.8-42.6% of patients. Amplification of the HER2 gene leads to overexpression of the HER2 protein on the tumor cell membrane, which in turn causes persistent activation of the HER2 receptor.
Studies show that breast cancer patients who have HER2 amplification or overexpression in their tumor tissue have shorter disease-free survival compared to patients without HER2 amplification or overexpression in their tumor tissue.
Trastuzumab blocks the proliferation of human tumor cells overexpressing HER2 in vivo and in vitro. In vitro, antibody-dependent cellular cytotoxicity of trastuzumab is predominantly directed toward tumor cells overexpressing HER2.
Immunogenicity
Antibodies to trastuzumab were detected in one of 903 patients with breast cancer who received the drug in monotherapy or in combination with chemotherapy, while she had no symptoms of allergy to Herceptin®.
There are no data on immunogenicity when using Herceptin® for the treatment of gastric cancer.
Pharmacokinetics
The pharmacokinetics of trastuzumab was studied in patients with metastatic breast cancer and early stages of breast cancer, as well as in patients with advanced gastric cancer. No special studies have been conducted to study drug-drug interactions.
Breast cancer
When the drug was administered in the form of short intravenous infusions at a dose of 10, 50, 100, 250 and 500 mg once a week, the pharmacokinetics were nonlinear. As the dose was increased, drug clearance decreased.
Half-life (T1/2)
T1/2 is 28-38 days, therefore, the elimination period after discontinuation of the drug is up to 27 weeks (190 days or 5 half-lives).
Pharmacokinetics of trastuzumab at steady state.
Steady state should be achieved after approximately 25 weeks. Using a population pharmacokinetic method (two-compartment model, model-dependent analysis) to evaluate data from phase I, phase II, and phase III studies in metastatic breast cancer, the median expected AUC at steady state at 3 weeks was 1677 mg x day/L after 3 doses (2 mg/kg) weekly and 1793 mg x day/L when administered after 3 weeks at a dose of 6 mg/kg. The calculated median Cmax were 104 mg/L and 189 mg/L, and Cmin were 64.9 mg/L and 47.3 mg/L, respectively. When using a model-independent or “non-compartmental analysis” method of analysis (non-compartmental analysis, NCA), the average Cmin at steady state by cycle 13 (week 37) was 63 mg/l in patients with early stages of breast cancer who received trastuzumab at a loading dose of 8 mg/kg, then at a maintenance dose of 6 mg/kg, after 3 weeks, and was comparable to that in patients with mBC treated with weekly trastuzumab.
Clearance
The typical clearance of trastuzumab (for a patient weighing 68 kg) was 0.241 L/day.
Volume of distribution
In all clinical studies, the volume of distribution in the central chamber (Vc) was 3.02 L, in the peripheral chamber (Vp) – 2.68 L for a typical patient.
Circulating extracellular domain of the HER2 receptor (antigen shed from the cell)
In the blood serum of some patients with breast cancer and HER2 overexpression, a circulating extracellular domain of the HER2 receptor (antigen “exfoliated” from the cell) was detected. In 64% of the examined patients, the initial serum samples revealed an antigen “exfoliated” from the cells in a concentration reaching 1880 ng/ml (median 11 ng/ml). Patients who had a high level of concentration of antigen “exfoliated” from the cell could probably have a lower Cmin. However, in the majority of patients with elevated levels of cell-shedding antigen, when the drug was administered weekly, the target serum trastuzumab concentration was achieved by week 6. There was no significant relationship between the initial level of antigen shed from the cell and the clinical response.
Advanced stomach cancer
Pharmacokinetics of Trastuzumab at Steady State To evaluate the pharmacokinetics of trastuzumab at steady state in patients with advanced gastric cancer after administration of trastuzumab at a loading dose of 8 mg/kg, followed by 6 mg/kg every 3 weeks, a nonlinear two-compartment population pharmacokinetic method was used using data from a phase III study.
The observed serum trastuzumab concentration levels were lower, suggesting that overall drug clearance was found to be higher in patients with advanced gastric cancer than in patients with breast cancer receiving the same dose of trastuzumab. The reason for this is unknown.
At high concentrations, total clearance is predominantly linear, and T1/2 is about 26 days.
The median estimated AUC (at steady state over a 3-week period) is 1213 mg x day/l, the median Cmax at steady state is 132 mg/l, the median Cmin is 27.6 mg/l.
There are no data on the level of the circulating extracellular domain of the HER2 receptor (cell-exfoliated antigen) in the serum of patients with gastric cancer.
Pharmacokinetics in special groups of patients
Separate pharmacokinetic studies have not been conducted in elderly patients and patients with renal or hepatic impairment. Age does not affect the distribution of trastuzumab.
Special instructions
Special instructions
Treatment with Herceptin® should only be carried out under the supervision of an oncologist. HER2 testing must be performed in a specialized laboratory that can provide quality control of the testing procedure.
Herceptin® should be used in patients with metastatic breast cancer or early stage breast cancer only in the presence of tumor overexpression of HER2, as determined by immunohistochemistry (IHC), or HER2 gene amplification, as determined by in situ hybridization (FISH or SISH). Accurate and validated determination methods should be used.
Herceptin® should be used in patients with metastatic gastric cancer only in the presence of tumor overexpression of HER2, determined by IHC as IHC2+ and confirmed by SISH or FISH, or IHC3+. Accurate and validated determination methods should be used.
There are currently no data from clinical studies on patients receiving Herceptin® repeatedly after use in adjuvant therapy.
Infusion reactions and hypersensitivity reactions
Infrequently, serious infusion-related adverse reactions occurred with Herceptin® administration: shortness of breath, hypotension, wheezing, hypertension, bronchospasm, supraventricular tachyarrhythmia, decreased hemoglobin oxygen saturation, anaphylaxis, respiratory distress syndrome, urticaria and angioedema. Most of them occurred during the infusion or within 2.5 hours from the start of the first administration. If an infusion reaction occurs, the administration should be stopped. The patient should be carefully monitored until all symptoms resolve. Effective therapy for serious reactions involves the use of oxygen inhalation, beta-agonists, and corticosteroids. If severe and life-threatening infusion reactions occur, discontinuation of further therapy with Herceptin® should be considered.
In rare cases, these reactions have been associated with a fatal outcome. The risk of fatal infusion reactions is higher in patients with shortness of breath at rest caused by pulmonary metastases or concomitant diseases, therefore such patients should not receive Herceptin® therapy.
Cases have been reported in which deterioration of the condition was observed after initial improvement, as well as cases with delayed rapid deterioration of the condition. Death occurred within hours to one week after infusion. In very rare cases, patients have developed symptoms of infusion reactions or pulmonary symptoms (more than 6 hours after starting Herceptin® administration). Patients should be warned about the possible delayed development of these symptoms and the need to immediately contact their doctor if they occur.
Lung disorders
When using the drug Herceptin® in the post-registration period, severe pulmonary events were recorded, which were sometimes accompanied by death. In addition, cases of interstitial lung disease (ILD), including pulmonary infiltrates, acute respiratory distress syndrome, pneumonia, pneumonitis, pleural effusion, acute pulmonary edema and respiratory failure, have been observed. Risk factors associated with ILD include: prior or concomitant therapy with other anti-neoplastic drugs known to be associated with ILD (taxanes, gemcitabine, vinorelbine, and radiation therapy). These phenomena can occur both during infusion (as manifestations of infusion reactions) and delayed. The risk of severe pulmonary reactions is higher in patients with metastatic lung disease, concomitant diseases, accompanied by shortness of breath at rest. Therefore, such patients should not receive Herceptin®. Caution should be exercised, especially in patients receiving concomitant taxane therapy, due to the development of pneumonitis.
Cardiotoxicity
General instructions
Heart failure (NYHA functional class II-IV) observed after therapy with Herceptin® as monotherapy or in combination with paclitaxel or docetaxel, especially after chemotherapy containing anthracyclines (doxorubicin or epirubicin), can be moderate to severe and in some cases can be fatal.
Patients who are scheduled to receive Herceptin®, especially those who have previously received anthracyclines and cyclophosphamide, should first undergo a thorough cardiac evaluation, including a history, physical examination, ECG, echocardiography, and/or radioisotope ventriculography or MRI.
Before starting treatment with Herceptin®, it is necessary to carefully weigh the possible benefits and risks of its use.
Since the T1/2 half of Herceptin® is about 28-38 days, the drug can remain in the blood for up to 27 weeks after completion of therapy. Patients receiving anthracyclines after completion of Herceptin® treatment may have an increased risk of cardiotoxicity. If possible, physicians should avoid prescribing anthracycline-based chemotherapy for 27 weeks after completion of Herceptin® therapy. When using anthracycline drugs, careful monitoring of cardiac function should be performed.
The need for a routine cardiac examination should be assessed in patients in whom cardiovascular disease is suspected during pre-treatment examination.
All patients should have cardiac function monitored during treatment (eg, every 12 weeks).
As a result of monitoring, it is possible to identify patients who have developed cardiac dysfunction.
In patients with asymptomatic cardiac dysfunction, more frequent monitoring (eg, every 6 to 8 weeks) may be beneficial. With prolonged deterioration in left ventricular function that does not manifest itself symptomatically, it is advisable to consider discontinuation of the drug if there is no clinical benefit from its use. Caution should be exercised during treatment in patients with symptomatic heart failure, hypertension, or a documented history of coronary artery disease, as well as in patients with early-stage breast cancer with a left ventricular ejection fraction ≤55%.
If LVEF falls to values below 50% and 10 points relative to the value before starting therapy, treatment should be suspended and LVEF re-evaluated no later than 3 weeks later. If LVEF does not improve or continues to decline, discontinuation of the drug should be considered if the benefit does not outweigh the risk in the patient. Such patients should be examined by a cardiologist and be under his supervision.
If symptomatic heart failure develops during Herceptin® therapy, appropriate standard drug therapy should be administered. Discontinuation of Herceptin® should be considered if clinically significant heart failure develops, unless the benefit of the drug in a particular patient outweighs the risk.
The safety of continuing or restarting Herceptin therapy in patients who develop cardiotoxicity has not been studied in prospective clinical studies. Most patients showed improvement with standard drug therapy in pivotal clinical trials. Diuretics, cardiac glycosides, beta-blockers and/or ACE inhibitors were used as standard therapy. In the presence of clinical benefit from the use of Herceptin®, the majority of patients with adverse reactions from the heart continued therapy without the manifestation of additional clinically significant reactions from the heart.
Metastatic breast cancer
It is not recommended to use Herceptin® in combination with anthracyclines for the treatment of metastatic breast cancer.
The risk of developing cardiotoxicity in patients with metastatic breast cancer is increased with prior anthracycline therapy, but it is lower compared with that with simultaneous use of anthracyclines and Herceptin®.
Early stages of breast cancer
Patients with early stages of breast cancer should have a cardiac evaluation before starting treatment, every 3 months during therapy, and every 6 months thereafter for 24 months after the last dose of the drug. Longer-term monitoring is recommended after treatment with Herceptin® in combination with anthracyclines, with examinations occurring once a year for 5 years from the date of the last dose of Herceptin®, or beyond if there is a prolonged decrease in LVEF.
Adjuvant therapy
It is not recommended to use Herceptin® in combination with anthracyclines as part of adjuvant therapy. In patients with early stage breast cancer who received Herceptin® after anthracycline-based chemotherapy, there was an increase in the incidence of symptomatic and asymptomatic adverse cardiac events compared with those who received chemotherapy with docetaxel and carboplatin (non-anthracycline-based regimens). However, the difference was greater in cases of combined use of Herceptin® and taxanes than in cases of sequential use.
Regardless of the regimen used, the majority of symptomatic cardiac events occurred in the first 18 months of treatment. In one of the 3 pivotal studies conducted (with a median follow-up of 5.5 years), there was a sustained increase in the cumulative incidence of symptomatic cardiac events or events associated with a decrease in LVEF: in 2.37% of patients receiving Herceptin® with taxanes after therapy with anthracyclines, compared with 1% of patients in the comparison groups (in the group of therapy with anthracyclines and cyclophosphamide, hereinafter taxanes, and in the group of therapy with taxanes, carboplatin and Herceptin®).
Since patients in the early stages of breast cancer with a history of established congestive heart failure, uncontrolled high-risk arrhythmias, angina pectoris requiring drug treatment, clinically significant heart defects, signs of transmural myocardial infarction according to ECG, poorly controlled arterial hypertension did not participate in the clinical trial, there is no information on the benefit/risk ratio in such patients, and therefore treatment with the drug it is not recommended for such patients.
Neoadjuvant-adjuvant therapy
For patients with early stages of breast cancer who may be eligible for neoadjuvant-adjuvant therapy, the use of Herceptin® in combination with anthracyclines is recommended only if they have not previously received chemotherapy and only when using low-dose anthracycline regimens (maximum total dose of doxorubicin 180 mg/m2 or epirubicin 360 mg/m2).
In patients receiving low doses of anthracyclines and Herceptin® as part of neoadjuvant therapy, additional cytotoxic chemotherapy after surgery is not recommended.
Since patients with heart failure of functional class II-IV according to NYHA, LVEF is 180 mm Hg. or diastolic > 100 mm Hg), clinically significant heart defects and uncontrolled high-risk arrhythmias were not included in the clinical study, treatment with Herceptin® is not recommended in such patients.
Experience with the use of trastuzumab in combination with low-dose anthracycline regimens is limited. When Herceptin® was used in conjunction with neoadjuvant chemotherapy, which included three cycles of neoadjuvant doxorubicin (total dose of doxorubicin 180 mg/m2), the incidence of symptomatic cardiac dysfunction was low (1.7%).
Neoadjuvant-adjuvant therapy with Herceptin® is not recommended for patients over the age of 65 years, since clinical experience in such patients is limited.
Additional information
When prescribing Herceptin® to a patient with hypersensitivity to benzyl alcohol, the drug must be diluted with water for injection, and only one dose can be taken from each multi-dose vial. The remaining drug should be thrown away.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
Studies have not been conducted to study the effect of the drug on the ability to drive a car and operate machinery. If symptoms of infusion reactions occur, patients should not drive or operate machinery until symptoms resolve.
Active ingredient
Active ingredient
Trastuzumab
Composition
Composition
Active ingredients:
trastuzumab 440 mg.
Excipients:
L-histidine hydrochloride – 9.9 mg,
L-histidine – 6.4 mg,
α,α-trehalose dihydrate – 400 mg,
polysorbate 20 – 1.8 mg.
Solvent (bacteriostatic water for injection – 20 ml, containing 1.1% benzyl alcohol as an antimicrobial preservative): benzyl alcohol – 229.9 mg, water for injection – 20.9 mg.
Pregnancy
Pregnancy
Women of childbearing potential must use reliable methods of contraception during treatment with Herceptin® and for at least 6 months after treatment.
If pregnancy occurs, the woman must be warned about the possibility of harmful effects on the fetus. If a pregnant woman continues to receive Herceptin® therapy, she should be closely monitored by doctors of various specialties. It is not known whether Herceptin® affects fertility in women. The results of animal experiments did not reveal signs of impaired fertility or negative effects on the fetus.
Breastfeeding is not recommended during treatment and for at least 6 months after the end of Herceptin® therapy.
Benzyl alcohol, contained as a preservative in Bacteriostatic Water for Injection supplied with each 440 mg multi-dose vial, is toxic to neonates and children under 3 years of age.
Contraindications
Contraindications
Severe shortness of breath at rest caused by pulmonary metastases or requiring oxygen maintenance;
children under 18 years of age (efficacy and safety of use in children have not been established);
pregnancy;
breastfeeding period;
hypersensitivity to trastuzumab or any other component of the drug, incl. to benzyl alcohol contained as a preservative in the bacteriostatic water for injection supplied with each 440 mg multi-dose vial.
With caution: use in case of coronary artery disease, arterial hypertension, heart failure, concomitant lung diseases or metastases to the lungs, previous therapy with cardiotoxic drugs, incl. anthracyclines/cyclophosphamide.
Side Effects
Side Effects
Currently, the most serious and/or common adverse reactions reported with the use of Herceptin® are: cardiotoxicity, infusion reactions, hematotoxicity (particularly neutropenia) and pulmonary disorders.
The following classification is used to describe the frequency of adverse reactions in this section:
very often (≥1/10);
often (≥1/100, but <1/10);
uncommon (≥1/1000, but <1/100);
rare (≥1/10,000, but <1/1000);
very rare (<1/10,000), unknown (cannot be calculated from available data).
Within each group, adverse reactions are presented according to decreasing severity.
The following are the adverse reactions reported with Herceptin®, both monotherapy and in combination with chemotherapy, in pivotal clinical trials and post-marketing use. Frequencies are based on the maximum observed in pivotal clinical studies.
Infectious and parasitic diseases: often – pneumonia1 (<1%), neutropenic sepsis, cystitis, Herpes zoster, infections, influenza, nasopharyngitis, sinusitis, skin infections, rhinitis, upper respiratory tract infections, urinary tract infections, erysipelas, phlegmon; infrequently - sepsis.
Benign, malignant and unspecified neoplasms (including cysts and polyps): unknown – progression of malignancy, progression of neoplasm.
From the blood and lymphatic system: very often – febrile neutropenia; often – anemia, neutropenia, thrombocytopenia, leukopenia; unknown – hypoprothrombinemia.
From the immune system: often – hypersensitivity reactions; unknown – anaphylactic reactions1, anaphylactic shock1.
Metabolism: often – weight loss, anorexia; unknown – hyperkalemia.
From the mental side: often – anxiety, depression, insomnia, impaired thinking.
From the nervous system: very often – tremor2, dizziness, headaches; often – peripheral neuropathy, paresthesia, muscle hypertonicity, drowsiness, dysgeusia (distortion of taste perception), ataxia; rarely – paresis; unknown – cerebral edema.
From the side of the organ of vision: very often – conjunctivitis, increased lacrimation; often – dry eyes; unknown – papilledema, retinal hemorrhage.
Hearing and labyrinthine disorders: uncommon – deafness.
From the cardiovascular system: very often – decrease and increase in blood pressure2, cardiac arrhythmia2, palpitations2, atrial or ventricular flutter2, decreased left ventricular ejection fraction3, “hot flashes”; often – heart failure (congestive)1 (2%), supraventricular tachyarrhythmia1,2, cardiomyopathy, arterial hypotension1,2, vasodilation; infrequently – pericardial effusion; unknown – cardiogenic shock, pericarditis, bradycardia, gallop rhythm.
From the respiratory system, chest and mediastinal organs: very often – wheezing1,2, shortness of breath1 (14%), cough, nosebleeds, rhinorrhea; often – bronchial asthma, impaired pulmonary function, pharyngitis; uncommon – pleural effusion1; rarely – pneumonitis; unknown – pulmonary fibrosis1, respiratory failure1, pulmonary infiltration1, acute pulmonary edema1, acute respiratory distress syndrome1, bronchospasm1, hypoxia1, decreased hemoglobin oxygen saturation1, laryngeal edema, orthopnea, pulmonary edema.
From the gastrointestinal tract: very often – diarrhea, vomiting, nausea, swelling of the lips2, abdominal pain; often – pancreatitis, dyspepsia, hemorrhoids, constipation, dry mouth.
From the liver and biliary tract: often – hepatitis, pain in the liver, hepatocellular damage; rarely – jaundice; unknown – liver failure.
From the skin and subcutaneous tissues: very often – erythema, rash, swelling of the face2; often – acne, alopecia, dry skin, ecchymosis, hyperhidrosis, maculopapular rash, abnormal nail structure, itching; unknown – angioedema, dermatitis, urticaria.
From the musculoskeletal system and connective tissue: very often – arthralgia, muscle stiffness2, myalgia; often – arthritis, back pain, ossalgia, muscle spasms, pain in the neck.
From the kidneys and urinary tract: often – kidney disease; unknown – membranous glomerulonephritis, glomerulonephropathy, renal failure.
Effect on pregnancy, postpartum and perinatal conditions: unknown – oligohydramnios, fatal pulmonary hypoplasia and renal hypoplasia in the fetus.
From the genital organs and mammary gland: often – inflammation of the mammary gland/mastitis.
General disorders and disorders at the injection site: very often – asthenia, chest pain, chills, weakness, flu-like syndrome, infusion reactions, pain, fever; often – peripheral edema, malaise, mucositis, edema.
Injuries, intoxication and complications of manipulation: often – bruise.
1 – adverse reactions that have been reported to be associated with death.
2 – adverse reactions, which were mainly reported in association with infusion reactions. The exact percentage has not been established.
3 – adverse reactions were observed during combination therapy after anthracyclines and in combination with taxanes.
The exact frequency percentages for those terms that were reported with a fatal outcome at a frequency of “often” or “very often” are presented in parentheses. The percentage refers to the total number of these events with and without fatal outcome.
The following adverse reactions were reported in the pivotal clinical studies with a frequency of ≥ 1/10 in any of the treatment groups, with no significant difference between the Herceptin®-containing treatment group and the comparison treatment group: lethargy, hypoesthesia, pain in the extremities, pain in the mouth and throat, lymphedema, weight gain, onychoclasia, musculoskeletal pain, pharyngitis, bronchitis, chest discomfort, epigastric pain, gastritis, stomatitis, vertigo, arterial hypertension, hiccups, hand-foot syndrome, breast pain, onychorrhexis, dyspnea on exertion and dysuria.
Below is information on individual adverse reactions.
Infusion reactions and hypersensitivity reactions
It is estimated that approximately 40% of patients receiving Herceptin® experience some form of infusion reaction. However, most infusion reactions are mild to moderate in severity (according to NCI-CTC) and tend to occur early in treatment, i.e. during the 1st, 2nd and 3rd infusions, with subsequent infusions they occur less frequently. Reactions include (but are not limited to) the following symptoms: chills, fever, rash, nausea and vomiting, shortness of breath and headache. Severe anaphylactic reactions requiring immediate additional medical intervention may most often occur during the first or second infusion of Herceptin® and have been associated with death.
Cardiotoxicity
NYHA functional class II-IV cardiotoxicity (heart failure) is a common adverse reaction with Herceptin® and has been associated with a fatal outcome. In 3 pivotal clinical trials of trastuzumab in combination with adjuvant chemotherapy, the incidence of grade 3/4 cardiac dysfunction (symptomatic congestive heart failure) was no different from that in patients receiving chemotherapy alone (i.e., without Herceptin®) or in patients receiving taxanes and Herceptin® sequentially (0.3-0.4%). The incidence was highest in patients receiving Herceptin® with taxanes (2%).
The safety of continuing or reinitiating Herceptin therapy in patients who have experienced cardiotoxicity has not been studied prospectively. However, the majority of patients experiencing heart failure in the pivotal studies improved with standard therapy, which included diuretics, cardiac glycosides, beta-blockers and/or ACE inhibitors.
The majority of patients with cardiac symptoms and evidence of clinical benefit from Herceptin® therapy continued therapy without the occurrence of additional clinically significant cardiac events.
Experience with the use of Herceptin® in combination with low-dose anthracycline regimens in neoadjuvant therapy is limited.
Hematological toxicity
Febrile neutropenia occurred very often. Adverse reactions that occur frequently include anemia, leukopenia, thrombocytopenia and neutropenia. The incidence of hypoprothrombinemia is unknown. The risk of neutropenia may be slightly higher when using trastuzumab in combination with docetaxel after therapy with anthracycline drugs.
Lung disorders
Severe pulmonary adverse events (including fatalities) are associated with the use of Herceptin®. These reactions include (but are not limited to): pulmonary infiltrates, acute respiratory distress syndrome, pneumonia, pneumonitis, pleural effusion, acute pulmonary edema and respiratory failure.
Interaction
Interaction
Specific drug interaction studies of Herceptin® have not been conducted in humans.
In clinical studies, no clinically significant interactions with concomitantly used drugs (including doxorubicin, paclitaxel, docetaxel, capecitabine or cisplatin) were observed.
Herceptin® is not compatible with 5% dextrose solution due to the possibility of protein aggregation.
Herceptin® should not be mixed or dissolved with other medicines.
There were no signs of incompatibility between Herceptin® solution and infusion bags made of polyvinyl chloride, polyethylene or polypropylene.
Overdose
Overdose
In clinical studies, no cases of drug overdose were observed. Administration of Herceptin® in single doses greater than 10 mg/kg has not been studied. Herceptin® in doses ≤10 mg/kg was well tolerated.
Storage conditions
Storage conditions
At 2–8 °C
Shelf life
Shelf life
4 years
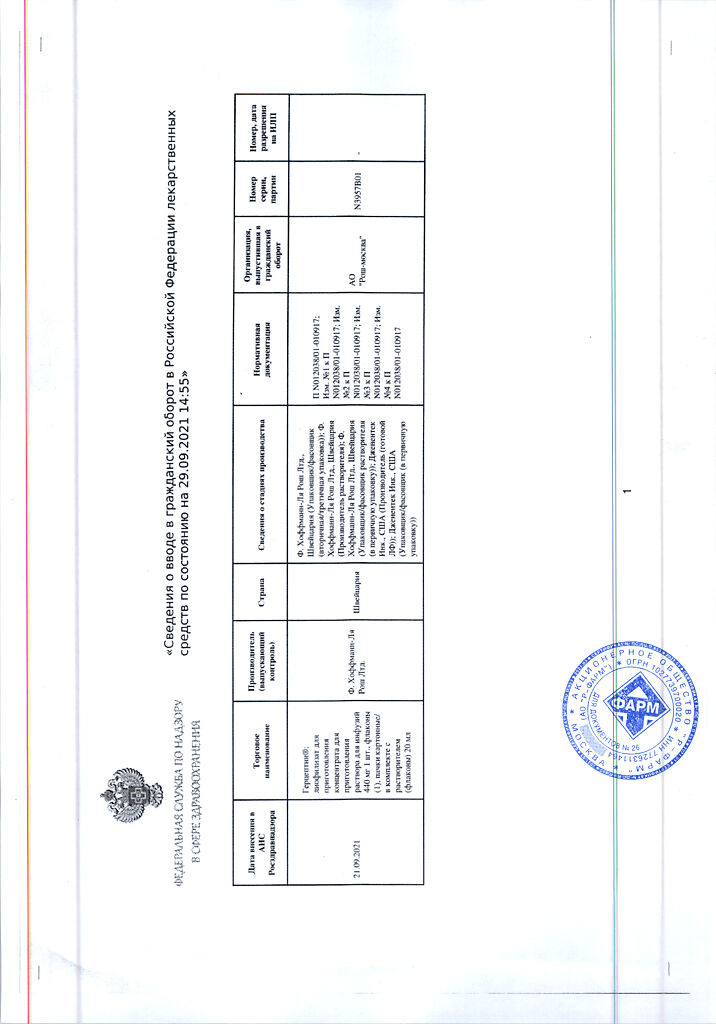
Manufacturer
Manufacturer
Genentech Inc., USA
Additional information
| Shelf life | 4 years |
|---|---|
| Conditions of storage | At 2-8 °C |
| Manufacturer | Genentech Inc. |
| Medication form | lyophilizate |
| Brand | #Н/Д |
Related products
Buy Herceptin, lyophilizate 440 mg +20 ml with delivery to USA, UK, Europe and over 120 other countries.