No products in the cart.
Glucovance, 5 mg+500 mg 30 pcs
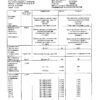
€12.33 €10.79
Description
Glucovans® is a fixed combination of two oral hypoglycemic agents of different pharmacological groups: metformin and glibenclamide.
Metformin belongs to the biguanide group and reduces both basal and postprandial plasma glucose levels. Metformin does not stimulate insulin secretion and therefore does not cause hypoglycemia. It has 3 mechanisms of action:
- reduces glucose production by the liver by inhibiting gluconeogenesis and glycogenolysis;
- increases peripheral receptor sensitivity to insulin, glucose consumption and utilization by muscle cells;
- delays glucose absorption in the gastrointestinal tract.
The drug also has beneficial effects on blood lipid composition, reducing the level of total cholesterol, LDL and triglycerides.
Glibenclamide belongs to the group of sulfonylurea derivatives of the II generation. Glucose content when taking glibenclamide decreases as a result of stimulation of insulin secretion by pancreatic β-cells.
Metformin and glibenclamide have different mechanisms of action, but mutually complement each other’s hypoglycemic activity. The combination of the two hypoglycemic agents has a synergistic effect in reducing glucose.
Pharmacokinetics
Glibenclamide. When administered orally, absorption from the gastrointestinal tract is more than 95%. Glibenclamide contained in Glucovans® is micronized. Cmax in plasma is reached in about 4 h, Vd – about 10 l. Binding to plasma proteins is 99%. It is almost completely metabolized in the liver to form two inactive metabolites, which are excreted by the kidneys (40%) and with the bile (60%). T1/2 is from 4 to 11 hours.
Metformin. After oral administration is absorbed from the gastrointestinal tract quite completely, Cmax in plasma is reached within 2.5 hours. About 20-30% of metformin is excreted unchanged through the gastrointestinal tract. Absolute bioavailability is 50 to 60%. Metformin is rapidly distributed in tissues, almost does not bind with plasma proteins. It is very poorly metabolized and excreted by the kidneys. T1/2 is on average 6.5 hours. With impaired renal function, renal clearance is decreased, as well as creatinine clearance, while the T1/2 is increased, which leads to increased plasma concentrations of metformin.
The combination of metformin and glibenclamide in the same dosage form has the same bioavailability as tablets containing metformin or glibenclamide alone. The bioavailability of metformin combined with glibenclamide is not affected by food intake, as is the bioavailability of glibenclamide. However, the absorption rate of glibenclamide increases with food intake.
Indications
Indications
Type 2 diabetes mellitus in adults:
if diet therapy, physical exercise and previous therapy with metformin or sulfonylurea derivatives are ineffective;
to replace previous therapy with two drugs (metformin and a sulfonylurea derivative) in patients with stable and well-controlled glycemic levels.
Pharmacological effect
Pharmacological effect
Glucovance® is a fixed combination of two oral hypoglycemic agents of different pharmacological groups: metformin and glibenclamide.
Metformin belongs to the group of biguanides and reduces the content of both basal and postprandial glucose in the blood plasma. Metformin does not stimulate insulin secretion and therefore does not cause hypoglycemia. Has 3 mechanisms of action:
reduces liver glucose production by inhibiting gluconeogenesis and glycogenolysis;
increases the sensitivity of peripheral receptors to insulin, the consumption and utilization of glucose by cells in the muscles;
delays the absorption of glucose in the gastrointestinal tract.
The drug also has a beneficial effect on blood lipids, reducing the level of total cholesterol, LDL and triglycerides.
Glibenclamide belongs to the group of sulfonylurea derivatives of the second generation. Glucose content when taking glibenclamide decreases as a result of stimulation of insulin secretion by pancreatic β-cells.
Metformin and glibenclamide have different mechanisms of action, but complement each other’s hypoglycemic activity. The combination of two hypoglycemic agents has a synergistic effect in reducing glucose levels.
Pharmacokinetics
Glibenclamide. When taken orally, absorption from the gastrointestinal tract is more than 95%. Glibenclamide, which is part of the drug Glucovance®, is micronized. Cmax in plasma is achieved in approximately 4 hours, Vd – about 10 l. Communication with plasma proteins is 99%. Almost completely metabolized in the liver with the formation of two inactive metabolites, which are excreted by the kidneys (40%) and bile (60%). T1/2 – from 4 to 11 hours.
Metformin. After oral administration, it is absorbed from the gastrointestinal tract quite completely, Cmax in plasma is reached within 2.5 hours. Approximately 20–30% of metformin is excreted through the gastrointestinal tract unchanged. Absolute bioavailability ranges from 50 to 60%. Metformin is quickly distributed in tissues and practically does not bind to plasma proteins. It is metabolized to a very weak extent and is excreted by the kidneys. T1/2 averages 6.5 hours. If renal function is impaired, renal clearance decreases, as does creatinine clearance, while T1/2 increases, which leads to an increase in the concentration of metformin in the blood plasma.
The combination of metformin and glibenclamide in one dosage form has the same bioavailability as when taking tablets containing metformin or glibenclamide alone. The bioavailability of metformin in combination with glibenclamide is not affected by food intake, nor is the bioavailability of glibenclamide. However, the rate of absorption of glibenclamide increases with food intake.
Special instructions
Special instructions
During treatment with Glucovance®, it is necessary to regularly monitor the level of glycemia on an empty stomach and after meals.
Lactic acidosis
Lactic acidosis is an extremely rare but serious (high mortality rate unless promptly treated) complication that can occur due to accumulation of metformin. Cases of lactic acidosis in patients receiving metformin occurred mainly in diabetic patients with severe renal failure.
Other associated risk factors should be considered, such as poorly controlled diabetes, ketosis, prolonged fasting, excessive alcohol consumption, liver failure and any condition associated with severe hypoxia.
The risk of developing lactic acidosis should be taken into account when nonspecific signs appear, such as muscle cramps accompanied by dyspeptic disorders, abdominal pain and severe malaise. In severe cases, acidotic dyspnea, hypoxia, hypothermia and coma may occur.
Diagnostic laboratory parameters are: low blood pH, plasma lactate concentration above 5 mmol/L, increased anion gap and lactate/pyruvate ratio.
Hypoglycemia
Since Glucovance® contains glibenclamide, taking the drug is accompanied by a risk of hypoglycemia in the patient. Gradual dose titration after initiation of treatment may prevent the occurrence of hypoglycemia. This treatment can only be prescribed to a patient who adheres to a regular diet (including breakfast). It is important that carbohydrate intake is regular, as the risk of hypoglycemia increases with late meals, insufficient or unbalanced carbohydrate intake. The development of hypoglycemia is most likely during a hypocaloric diet, after intense or prolonged physical activity, when drinking alcohol or taking a combination of hypoglycemic agents.
Due to compensatory reactions caused by hypoglycemia, sweating, fear, tachycardia, hypertension, palpitations, angina pectoris and arrhythmia may occur. The latter symptoms may be absent if hypoglycemia develops slowly, in the case of autonomic neuropathy, or while taking beta-blockers, clonidine, reserpine, guanethidine or sympathomimetics.
Other symptoms of hypoglycemia in patients with diabetes mellitus may include headache, hunger, nausea, vomiting, severe fatigue, sleep disturbance, restlessness, aggression, impaired concentration and psychomotor reactions, depression, confusion, speech impairment, visual impairment, trembling, paralysis and paresthesia, dizziness, delirium, convulsions, somnolence, unconsciousness, shallow breathing and bradycardia.
Careful prescribing, dose selection, and appropriate patient instructions are important to reduce the risk of hypoglycemia. If the patient has recurrent episodes of hypoglycemia that are either severe or due to unawareness of symptoms, treatment with other hypoglycemic agents should be considered.
Factors contributing to the development of hypoglycemia:
simultaneous use of alcohol, especially during fasting;
refusal or (especially for older patients) inability of the patient to interact with the doctor and follow the recommendations set out in the instructions for use;
poor nutrition, irregular eating, fasting, or changes in diet;
imbalance between physical activity and carbohydrate intake;
renal failure;
severe liver failure;
overdose of the drug Glucovance®;
certain endocrine disorders: insufficiency of the thyroid gland, pituitary gland and adrenal glands;
simultaneous use of individual medications.
Kidney and liver failure
Pharmacokinetics and/or pharmacodynamics may vary in patients with hepatic impairment or severe renal impairment. The hypoglycemia that occurs in such patients can be prolonged, in which case appropriate treatment should be started.
Instability of blood glucose levels
In the case of surgery or other cause of decompensation of diabetes, it is recommended to consider a temporary transition to insulin therapy. Symptoms of hyperglycemia include frequent urination, severe thirst, and dry skin.
48 hours before planned surgery or intravenous administration of an iodinated radiocontrast agent, Glucovance® should be discontinued. Treatment is recommended to be resumed after 48 hours and only after renal function has been assessed and found to be normal.
Kidney function
Since metformin is excreted by the kidneys, before starting treatment and regularly thereafter, it is necessary to determine creatinine Cl and/or serum creatinine levels: at least once a year in patients with normal renal function, and 2–4 times a year in elderly patients, as well as in patients with creatinine Cl at ULN.
Particular caution is recommended in cases where renal function may be impaired, such as in elderly patients or when starting antihypertensive therapy, diuretics or NSAIDs.
Other Precautions
The patient should inform the doctor about the occurrence of a bronchopulmonary infection or infectious disease of the genitourinary organs.
Impact on the ability to drive a car and operate machinery. Patients should be informed about the risk of hypoglycemia and take precautions when driving a car and operating machinery that requires increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Glibenclamide, Metformin
Composition
Composition
Active ingredients:
glibenclamide;
metformin hydrochloride;
Excipients:
croscarmellose sodium;
povidone K30;
MCC;
magnesium stearate
Contraindications
Contraindications
hypersensitivity to metformin, glibenclamide or other sulfonylurea derivatives, as well as to excipients;
diabetes mellitus type I;
diabetic ketoacidosis, diabetic precoma, diabetic coma;
renal failure or impaired renal function (Cl creatinine
acute conditions that can lead to changes in kidney function: dehydration, severe infection, shock, intravascular administration of iodine-containing contrast agents (see “Special Instructions”);
acute or chronic diseases that are accompanied by tissue hypoxia: cardiac or respiratory failure, recent myocardial infarction, shock;
liver failure;
porphyria;
pregnancy;
breastfeeding period;
simultaneous use of miconazole;
extensive surgical operations;
chronic alcoholism, acute alcohol intoxication;
lactic acidosis (including history);
following a hypocaloric diet (
It is not recommended to use the drug in people over 60 years of age who perform heavy physical work, which is associated with an increased risk of developing lactic acidosis.
Glucovance® contains lactose, therefore its use is not recommended for patients with rare hereditary diseases associated with galactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome.
With caution: febrile syndrome, adrenal insufficiency, hypofunction of the anterior pituitary gland, diseases of the thyroid gland with uncompensated impairment of its function.
Side Effects
Side Effects
Metabolic disorders: hypoglycemia (see “Overdose”, “Special instructions”). Rarely – attacks of hepatic porphyria and cutaneous porphyria; very rarely – lactic acidosis (see “Special Instructions”). Decreased absorption of vitamin B12, accompanied by a decrease in its concentration in the blood serum with long-term use of metformin. When megaloblastic anemia is detected, the possibility of such an etiology must be taken into account. Disulfiram-like reaction when drinking alcohol.
Laboratory indicators: infrequently – an increase in serum urea and creatinine concentrations from moderate to moderate; very rarely – hyponatremia.
From the circulatory and lymphatic systems: these adverse effects disappear after discontinuation of the drug. Rarely – leukopenia and thrombocytopenia; very rarely – agranulocytosis, hemolytic anemia, bone marrow aplasia and pancytopenia.
From the nervous system: often – taste disturbance (metallic taste in the mouth).
On the part of the visual organs: at the beginning of treatment, temporary visual impairment may occur due to a decrease in blood glucose.
From the gastrointestinal tract: very often – nausea, vomiting, diarrhea, abdominal pain and lack of appetite. These symptoms are more common at the beginning of treatment and in most cases go away on their own. To prevent the development of these symptoms, it is recommended to take the drug in 2 or 3 doses; Slowly increasing the dose of the drug also improves its tolerability.
From the skin and subcutaneous tissue: rarely – skin reactions such as itching, urticaria, maculopapular rash; very rarely – cutaneous or visceral allergic vasculitis, polymorphic erythema, exfoliative dermatitis, photosensitivity.
Immunological reactions: very rarely – anaphylactic shock. Cross-hypersensitivity reactions to sulfonamides and their derivatives may occur.
Hepatobiliary disorders: very rarely – abnormal liver function tests or hepatitis requiring discontinuation of treatment.
Interaction
Interaction
Contraindicated combinations
Associated with the use of glibenclamide
Miconazole: may provoke the development of hypoglycemia (up to the development of coma).
Associated with metformin use
Iodinated contrast media: Depending on renal function, the drug should be discontinued 48 hours before or after intravenous administration of iodinated contrast media.
Combinations not recommended
Related to the use of sulfonylurea derivatives
Alcohol: Antabuse reaction (alcohol intolerance) is very rarely observed when taking alcohol and glibenclamide simultaneously. Alcohol intake may increase the hypoglycemic effect (by inhibiting compensatory reactions or delaying its metabolic inactivation), which may contribute to the development of hypoglycemic coma. During treatment with Glucovance®, you should avoid drinking alcohol and drugs containing alcohol.
Phenylbutazone increases the hypoglycemic effect of sulfonylurea derivatives (by replacing sulfonylurea derivatives at protein binding sites and/or reducing their elimination). It is preferable to use other anti-inflammatory drugs that exhibit fewer interactions, or to warn the patient about the need to self-monitor glycemic levels; If necessary, the dose should be adjusted when using an anti-inflammatory drug together and after its discontinuation.
Associated with the use of glibenclamide
Bosentan: in combination with glibenclamide increases the risk of hepatotoxicity. It is recommended to avoid taking these drugs together. The hypoglycemic effect of glibenclamide may also be reduced.
Associated with metformin use
Alcohol: The risk of developing lactic acidosis increases with acute alcohol intoxication, especially in cases of fasting or poor nutrition, or liver failure. During treatment with Glucovance®, you should avoid drinking alcohol and drugs containing alcohol.
Combinations requiring caution
Associated with the use of all hypoglycemic agents
Chlorpromazine: in high doses (100 mg/day) causes an increase in glycemic levels (reducing insulin release). Precautions: the patient should be warned about the need to independently monitor blood glucose levels and, if necessary, adjust the dose of the hypoglycemic agent during simultaneous use of the antipsychotic and after discontinuation of its use.
GCS and tetracosactide: an increase in blood glucose levels, sometimes accompanied by ketosis (GCS cause a decrease in glucose tolerance). Precautions: the patient should be warned about the need to independently monitor blood glucose levels and, if necessary, adjust the dose of the hypoglycemic agent during the simultaneous use of GCS and after discontinuation of their use.
Danazol: has a hyperglycemic effect. If treatment with danazol is necessary and when taking the latter, a dose adjustment of the drug Glucovance is required under the control of glycemic levels.
β2-adrenergic agonists: by stimulating β2-adrenergic receptors, they increase the concentration of glucose in the blood. Precautions: it is necessary to warn the patient and establish control of blood glucose levels; transfer to insulin therapy is possible.
Diuretics: increase blood glucose levels. Precautions: the patient should be warned about the need to independently monitor blood glucose levels; It may be necessary to adjust the dose of the hypoglycemic agent during simultaneous use with diuretics and after discontinuation of their use.
ACE inhibitors (captopril, enalapril): the use of ACE inhibitors helps reduce blood glucose levels. If necessary, the dose of Glucovance should be adjusted during simultaneous use with ACE inhibitors and after discontinuation of their use.
Associated with metformin use
Diuretics: lactic acidosis that occurs when taking metformin against the background of functional renal failure caused by taking diuretics, especially loop diuretics.
Associated with the use of glibenclamide
β-blockers, clonidine, reserpine, guanethidine and sympathomimetics mask some symptoms of hypoglycemia: palpitations and tachycardia; Most non-selective beta-blockers increase the incidence and severity of hypoglycemia. The patient should be warned about the need to independently monitor blood glucose levels, especially at the beginning of treatment.
Fluconazole: an increase in T1/2 of glibenclamide with the possible occurrence of manifestations of hypoglycemia. The patient should be warned about the need to self-monitor blood glucose levels; It may be necessary to adjust the dose of hypoglycemic drugs during concomitant treatment with fluconazole and after discontinuation of its use.
Other Interactions: Combinations to Consider
Associated with the use of glibenclamide
Desmopressin: Glucovance® may reduce the antidiuretic effect of desmopressin.
Antibacterial drugs from the group of sulfonamides, fluoroquinolones, anticoagulants (coumarin derivatives), MAO inhibitors, chloramphenicol, pentoxifylline, lipid-lowering drugs from the group of fibrates, disopyramide: the risk of developing hypoglycemia during the use of glibenclamide.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C.
Shelf life
Shelf life
3 years
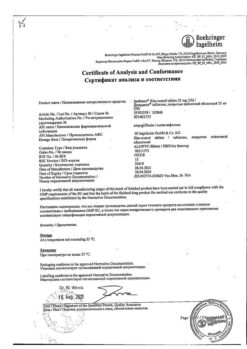
Manufacturer
Manufacturer
Merck Santé S.a.S., France
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C. |
| Manufacturer | Merck Santé S.a.s., France |
| Medication form | pills |
| Brand | Merck Santé S.a.s. |
Other forms…
Related products
Buy Glucovance, 5 mg+500 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.