No products in the cart.
Glibenclamide+Metformin, 2.5mg+500 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: oral hypoglycemic agents (sulfonylurea derivative of the II generation + biguanide).
ATX code: A10BD02
Pharmacological properties
Pharmacodynamics
The drug is a fixed combination of two oral hypoglycemic agents of different pharmacological groups: metformin and glibenclamide. Metformin belongs to the biguanide group and reduces both basal and postprandial plasma glucose levels. Metformin does not stimulate insulin secretion and therefore does not cause hypoglycemia.
Has 3 mechanisms of action:
– reduces glucose production by the liver by inhibiting gluconeogenesis and glycogenolysis;
– Increases the sensitivity of peripheral receptors to insulin, glucose consumption and utilization by cells in the muscles;
– Delays glucose absorption in the gastrointestinal tract (GIT).
Metformin also has beneficial effects on blood lipid composition, reducing the concentration of total cholesterol, low-density lipoproteins (LDL) and triglycerides.
Glibenclamide belongs to the group of sulfonylurea derivatives of II generation. Glucose content when taking glibenclamide decreases as a result of stimulation of insulin secretion by pancreatic β-cells. Metformin and glibenclamide have different mechanisms of action, but mutually complement the hypoglycemic activity of each other. The combination of the two hypoglycemic agents has a synergistic effect in reducing blood glucose levels.
Pharmacokinetics
Glibenclamide
Absorption
In oral administration, absorption from the GI tract is more than 95%. The maximum concentration (Cmax) in plasma is reached in about 4 hours.
Distribution
The binding to plasma proteins is 99%. The volume of distribution is about 10 liters.
Metabolism and excretion
It is almost completely metabolized in the liver to form two inactive metabolites, which are excreted by the kidneys (40%) and through the intestine (60%). The elimination half-life (T1/2) is 4 to 11 hours.
Metformin
Absorption
After oral administration metformin is absorbed from the gastrointestinal tract quite completely, Cmax in plasma is reached within 2.5 hours. Absolute bioavailability is 50 to 60%.
Distribution
Metformin is rapidly distributed in the tissues, practically does not bind with plasma proteins.
Metabolism
It is metabolized to a very low degree and is excreted by the kidneys. About 20-30% of metformin is excreted unchanged in the intestine. T1/2 is on average 6.5 hours.
In impaired renal function, renal clearance decreases as does creatinine clearance, with an increased T1/2 that leads to increased plasma concentrations of metformin.
The combination of metformin and glibenclamide in one tablet has the same bioavailability as when tablets containing metformin or glibenclamide are taken simultaneously separately.
The bioavailability of metformin combined with glibenclamide is not affected by food intake, as is the bioavailability of glibenclamide. However, the absorption rate of glibenclamide increases with food intake.
Indications
Indications
Type 2 diabetes mellitus in adults:
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Interaction
Interaction
Contraindicated combinations
Associated with glibenclamide
Miconazole may cause hypoglycemia (up to and including coma).
Injurious to metformin use
Iodine-containing contrast agents: depending on renal function, the drug should be discontinued 48 hours before and 48 hours after intravenous administration of iodine-containing contrast agents.
Unrecommended combinations
Related to the use of sulfonylurea derivatives
Alcohol: a disulfiram-like reaction (alcohol intolerance) is very rarely observed when alcohol and glibenclamide are taken simultaneously. Alcohol intake may increase the hypoglycemic effect (by inhibiting the compensatory reactions or delaying its metabolic inactivation), which may contribute to the development of hypoglycemic coma. Alcohol and medicinal products containing ethanol should be avoided during treatment with the drug.
Phenylbutazone increases the hypoglycemic effect of sulfonylurea derivatives (by replacing sulfonylurea derivatives at the sites of binding to the protein and/or reducing their excretion). It is preferable to use other anti-inflammatory agents that find fewer interactions, or to warn the patient about the need for self-control of glycemic levels; if necessary, the dose should be adjusted when co-administering the anti-inflammatory agent and after discontinuation.
Linked with glibenclamide
Bozentan in combination with glibenclamide increases the risk of hepatotoxic effects. The hypoglycemic effect of glibenclamide may also be reduced. Concomitant use of these drugs is not recommended.
Related to the use of metformin
Alcohol: the risk of lactoacidosis is increased in acute alcohol intoxication, especially in case of starvation, malnutrition or liver failure.
Alcohol and medicinal products containing ethanol should be avoided during treatment with the drug.
Combinations requiring caution
Related to the use of all hypoglycemic agents
Chlorpromazine: in high doses (100 mg/day) causes increased glycemia (reducing insulin secretion).
Precautionary measures: the patient should be advised to monitor blood glucose levels independently; if necessary, the drug dose should be adjusted if used concomitantly with neuroleptics and after stopping their use.
Glucocorticosteroids (GCS) and tetracosactide: Increased blood glucose, sometimes accompanied by ketosis (GCS cause decreased glucose tolerance).
Precautionary measures: the patient should be warned about the need for self-monitoring of blood glucose; if necessary, the drug dose should be adjusted if used concomitantly with GCS and after stopping their use.
Danazolol has a hyperglycemic effect. If treatment with danazolol is necessary and after discontinuation of danazolol, the dose should be adjusted with glycemic control.
Beta2-adrenomimetics: by stimulating beta2-adrenoreceptors increase blood glucose concentration.
Precautionary measures: the patient should be warned about the need for self-control of blood glucose; transfer to insulin therapy is possible.
Diuretics: increase in blood glucose.
Precautionary measures: the patient should be warned about the need for self-monitoring of blood glucose; the drug dose may need to be adjusted if used concomitantly with diuretics and after stopping their use.
Angiotensin-converting enzyme (ACE) inhibitors (captopril, enalapril): use of ACE inhibitors reduces blood glucose. If necessary, the dose of the drug should be adjusted when concomitant use with ACE inhibitors and after discontinuation of their use.
Associated with the use of metformin
Diuretics: lactoacidosis occurring when taking metformin against a background of functional renal failure caused by taking diuretics, especially “loop” diuretics. Associated with the use of glibenclamide
Beta-adrenoblockers, clonidine, reserpine, guanethidine, and sympathomimetics mask some symptoms of hypoglycemia: palpitations and tachycardia; most non-selective beta-adrenoblockers increase the frequency and severity of hypoglycemia.
Patients should be advised to self-monitor blood glucose, especially at the start of treatment.
Fluconazole: increase T1/2 of glibenclamide with possible development of hypoglycemia. Patients should be cautioned about the need for self-monitoring of blood glucose; the drug dose may need to be adjusted during concomitant use with fluconazole and after discontinuation.
Other interactions: combinations to consider:
Involved with glibenclamide
Desmopressin: Glibenclamide + Metformin may decrease the antidiuretic effect of desmopressin.
Antibacterial drugs (drugs) from the group of sulfonamides, fluoroquinolones, anticoagulants (coumarin derivatives), monoamine oxidase inhibitors, chloramphenicol, pentoxifylline, hypolipidemic drugs from the group of fibrates, disopyramide – risk of hypoglycemia with glibenclamide.
Special Instructions
Special Instructions
During use of Glibenclamide + Metformin, glycemia levels should be monitored regularly on an empty stomach and after meals.
Lactoacidosis
Lactoacidosis is an extremely rare but serious (high mortality if not treated urgently) complication that can occur due to metformin cumulation. Cases of lactoacidosis in patients treated with metformin occurred mainly in diabetic patients with severe renal insufficiency.
Contraindications
Contraindications
Side effects
Side effects
Overdose
Overdose
Pregnancy use
Pregnancy use
Similarities
Similarities
Additional information
| Weight | 0.040 kg |
|---|---|
| Shelf life | 3 years. Do not use after the expiration date. |
| Conditions of storage | At a temperature not exceeding 25 ° C. Keep out of reach of children. |
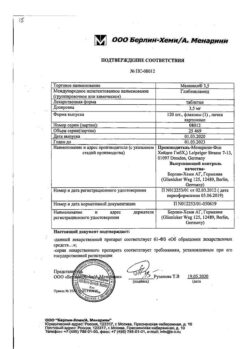
| Manufacturer | Ozon, Russia |
| Medication form | pills |
| Brand | Ozon |
Other forms…
Related products
Buy Glibenclamide+Metformin, 2.5mg+500 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.