No products in the cart.
Description
Pharmacodynamics
Antitumor drug, antimetabolite of pyrimidine analogues group. The drug exhibits cyclospecificity, acting on cells in S phase (replication phase) and G1/S phase (interval between initial growth phase and replication phase).
Hemcitabine is metabolized inside the cell under the action of nucleosidkinases to form active diphosphate and triphosphate nucleosides. Diphosphate nucleosides inhibit ribonucleotide reductase, which acts as the sole catalyst for reactions leading to the formation of deoxynucleoside triphosphates required for DNA synthesis. Triphosphate nucleosides actively compete with deoxycytidine triphosphate for incorporation into DNA and RNA molecules. Once the intracellular metabolites of gemcitabine are incorporated into the DNA strand, one additional nucleotide is added to its growing strands, resulting in complete inhibition of further DNA synthesis and programmed cell death, known as apoptosis.
Pharmacokinetics
Distribution
The binding to plasma proteins is negligible.
Elevation
The T1/2 varies from 32 to 94 minutes. Gemcitabine is rapidly excreted by the kidneys mainly as the inactive metabolite 2′-deoxy-2′,2′-difluoruridine. Less than 10% of the dose administered intravenously is found unchanged in the urine.
The systemic clearance varies from 30 to 90 l/h/m2.
Pharmacokinetics in special clinical cases
The analysis of pharmacokinetic studies with single and multiple administration of the drug shows that Vd is significantly gender dependent.
The systemic clearance, which ranges from approximately 30 L/h/m2 to 90 L/h/m2, depends on sex and age.
Indications
Indications
Locally advanced or metastatic non-small cell lung cancer – as first-line therapy in combination with cisplatin or carboplatin, as well as monotherapy in elderly patients with performance status equal to 2;
unresectable, locally recurrent or metastatic breast cancer – as part of combination therapy with paclitaxel after neoadjuvant and/or adjuvant therapy with the inclusion of anthracyclines in the absence of contraindications to their use;
locally advanced or metastatic urothelial cancer (cancer of the bladder, renal pelvis, ureter, urethra);
locally advanced or metastatic epithelial ovarian cancer as monotherapy or in combination with carboplatin in patients with disease progression after first-line platinum-based therapy;
locally advanced or metastatic pancreatic cancer;
locally advanced or metastatic cervical cancer;
biliary tract cancer.
Gemcitabine has been shown to be effective in advanced small cell lung cancer and advanced refractory testicular cancer.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Antitumor drug, antimetabolite of the group of pyrimidine analogues. The drug exhibits cyclospecificity, acting on cells in the S phase (replication phase) and G1/S (the interval between the initial growth phase and the replication phase).
Gemcitabine is metabolized intracellularly by nucleoside kinases to form active diphosphate and triphosphate nucleosides. Diphosphate nucleosides inhibit ribonucleotide reductase, which acts as the sole catalyst for the reactions leading to the formation of deoxynucleoside triphosphates necessary for DNA synthesis. Triphosphate nucleosides actively compete with deoxycytidine triphosphate for incorporation into DNA and RNA molecules. After the intracellular metabolites of gemcitabine are incorporated into the DNA strand, one additional nucleotide is added to its growing strands, resulting in complete inhibition of further DNA synthesis and programmed cell death, known as apoptosis.
Pharmacokinetics
Distribution
Plasma protein binding is negligible.
Removal
T1/2 ranges from 32 to 94 minutes. Gemcitabine is rapidly excreted from the body by the kidneys, mainly in the form of an inactive metabolite 2′-deoxy-2′,2′-difluorouridine. Less than 10% of a dose administered intravenously is found unchanged in the urine.
System clearance ranges from 30 to 90 l/h/m2.
Pharmacokinetics in special clinical situations
Analysis of pharmacokinetic studies with single and repeated administration of the drug shows that Vd is significantly dependent on gender.
Systemic clearance, which ranges from approximately 30 l/h/m2 to 90 l/h/m2, depends on gender and age.
Special instructions
Special instructions
Treatment with gemcitabine should only be carried out under the supervision of a physician experienced in the use of anticancer chemotherapy.
Before each administration of gemcitabine, it is necessary to monitor the number of platelets, leukocytes and granulocytes in the blood. If there are signs of bone marrow suppression caused by the drug, it is necessary to suspend treatment or adjust the dose.
It is necessary to regularly examine the patient and assess kidney and liver function. Administration of gemcitabine for liver metastases, a history of hepatitis and alcoholism, as well as liver cirrhosis increases the risk of developing liver failure.
Increasing the duration of infusion and frequency of administration leads to increased toxicity.
Gemcitabine may suppress bone marrow activity, resulting in leukopenia, thrombocytopenia, or anemia.
Capillary leak syndrome, with potentially serious consequences, has been observed in patients receiving gemcitabine as monotherapy or in combination with other chemotherapy drugs. If capillary leak syndrome develops during therapy, treatment with gemcitabine should be discontinued and necessary measures taken. According to some literature data, capillary leak syndrome has been associated with respiratory distress syndrome in adults.
Depending on the degree of toxicity, the dose can be reduced during each cycle or at the start of a new cycle in steps.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
There have been no studies of the effect of gemcitabine on the ability to drive vehicles or operate machinery. However, gemcitabine is known to cause mild to moderate drowsiness, especially when combined with alcohol.
Patients should be warned not to operate machinery if they feel drowsy.
Active ingredient
Active ingredient
Gemcitabine
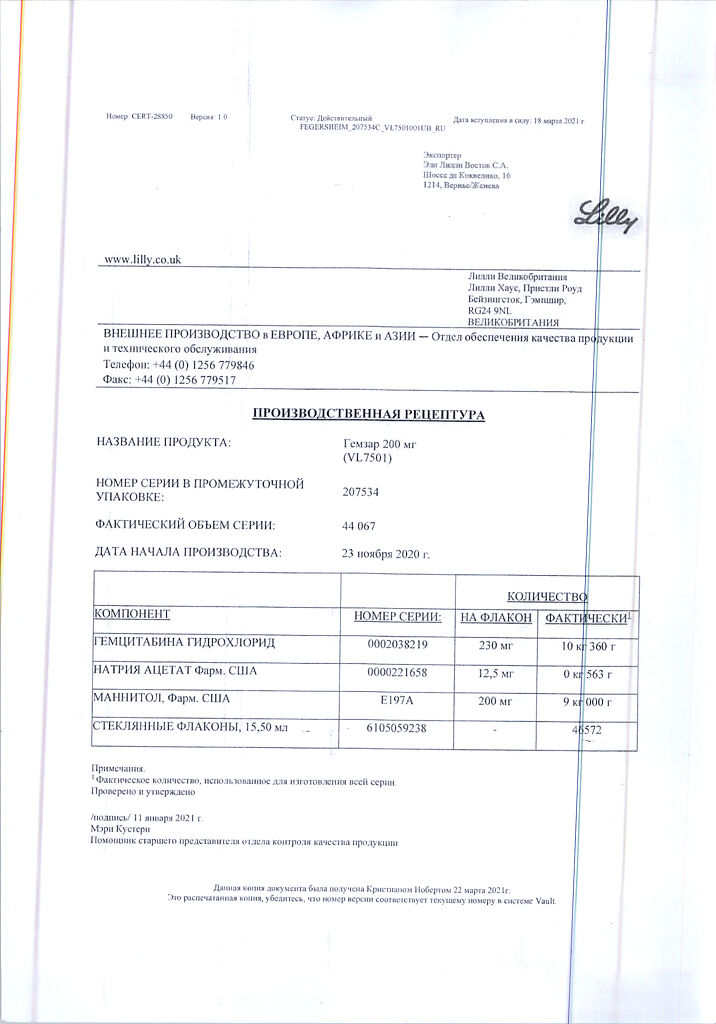
Composition
Composition
1 bottle contains:
Active substances:
gemcitabine hydrochloride 228 mg, which corresponds to the content of gemcitabine 200 mg.
Excipients:
mannitol – 200 mg,
sodium acetate – 12.5 mg.
Pregnancy
Pregnancy
The drug is contraindicated during pregnancy and lactation (breastfeeding).
Contraindications
Contraindications
Age up to 18 years;
pregnancy;
lactation period (breastfeeding);
hypersensitivity to gemcitabine or other components of the drug.
With caution: the drug is prescribed for impaired liver and/or kidney function, suppression of bone marrow hematopoiesis (including during concomitant radiation or chemotherapy), acute infectious diseases of a viral, fungal or bacterial nature.
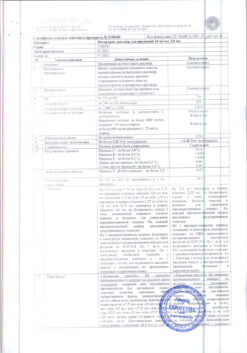
Side Effects
Side Effects
Adverse reactions that occurred more often than in isolated cases are listed according to the following gradation:
very often (≥10%);
often (≥1%, <10%);
uncommon (≥0.1%, <1%);
rare (≥0.01%, <0.1%);
very rare (<0.01%).
From the hematopoietic system: very often – anemia, leukopenia, thrombocytopenia; often – febrile neutropenia; very rarely – thrombocytosis.
Metabolic disorders: often – anorexia.
From the nervous system: often – headache, sleep disturbance, drowsiness.
From the cardiovascular system: very often – edema, peripheral edema; infrequently – heart failure, arrhythmia, mainly supraventricular; rarely – myocardial infarction, decreased blood pressure.
From the respiratory system: very often – shortness of breath; often – cough, rhinitis; infrequently – bronchospasm.
From the digestive system: very often – impaired liver function (usually mild, rarely requiring cessation of treatment), nausea, vomiting; often – diarrhea, stomatitis, constipation.
From the skin and subcutaneous tissues: very often – mild skin rashes accompanied by itching, alopecia (usually minimal hair loss); often – itching, sweating; rarely – ulcers, formation of vesicles.
From the urinary system: very often – mild proteinuria and hematuria.
From the musculoskeletal system: often – back pain, myalgia.
Allergic reactions: very rarely – anaphylactoid reactions, anaphylactic reaction.
Other: very often – flu-like syndrome (fever, headache, chills, asthenia, malaise); rarely – reactions at the injection site. Fever and asthenia are often reported as separate symptoms. Radiation toxicity has been rarely reported.
Post-marketing data
From the cardiovascular system: infrequently – heart failure, arrhythmia, mainly supraventricular; rarely – gangrene and peripheral vasculitis; very rarely – capillary hyperpermeability syndrome.
From the respiratory system: infrequently – interstitial pneumonitis; rarely – adult respiratory distress syndrome, pulmonary edema. If such effects occur, discontinuation of gemcitabine therapy should be considered. Early maintenance therapy may improve the situation.
From the digestive system: very rarely – ischemic colitis.
From the skin and subcutaneous tissues: rarely – severe skin reactions, including desquamation and bullous skin lesions.
From the urinary system: rarely – hemolytic-uremic syndrome. At the first sign of any manifestations of microangiopathic hemolytic anemia (for example, a sharp decrease in hemoglobin with concomitant thrombocytopenia, an increase in bilirubin, serum creatinine, urea or LDH), gemcitabine therapy should be discontinued immediately. Renal failure may be irreversible even after stopping therapy and dialysis may be required.
From the liver and biliary tract: very often – increased activity of liver enzymes: AST, ALT, alkaline phosphatase; often – increased bilirubin concentration; uncommon – severe hepatotoxicity, including liver failure; rarely – increased GGT activity.
Other: very rarely – Lyell’s syndrome, Stevens-Johnson syndrome; radiation reactions were recorded.
Interaction
Interaction
Radiation therapy
Concomitant use (coadministration or less than 7 days apart): Toxicity associated with this multimodal treatment depends on many different factors: dose of gemcitabine, frequency of gemcitabine administration, radiation dose, radiation treatment planning technique, type and volume of tissue treated.
Preclinical and clinical studies have shown that gemcitabine has a radiosensitizing effect. In the only study in which gemcitabine was administered at a dose of 1000 mg/m2 for 6 weeks concomitantly with therapeutic chest irradiation in patients with non-small cell lung cancer, significant toxicity was reported in the form of severe and potentially life-threatening mucosal inflammation, mainly esophagitis, as well as pneumonitis, especially in patients with large volumes of tissue irradiation (median volume of irradiation 4795 cm3).
Subsequent studies (phase II studies in non-small cell lung cancer) indicate the advisability of administering gemcitabine at lower doses with concomitant radiation therapy with predicted toxicity. Radiation therapy to the chest area (SD 66 Gy) was carried out simultaneously with chemotherapy with gemcitabine at a dose of 600 mg/m2 (4 injections) and cisplatin at a dose of 80 mg/m2 (2 injections) for 6 weeks. Several phase I and II studies have shown that in non-small cell lung cancer and pancreatic cancer, it is more appropriate to administer gemcitabine monotherapy (up to 300 mg/m2/week) in parallel with radiation therapy. The optimal regimen for safely administering gemcitabine with therapeutic doses of radiotherapy has not yet been established for all tumor types.
Sequential use (interval greater than 7 days): Other than radiation reaction when gemcitabine was administered more than 7 days before or after radiation therapy, no increase in toxicity was observed. These data suggest that gemcitabine can be administered one week after radiotherapy or after the acute effects of radiotherapy have resolved. Radiation damage to irradiated tissues (eg, esophagitis, colitis, and pneumonitis) has been reported with both concurrent and sequential use of gemcitabine with radiation therapy.
Other
Concomitant use with live yellow fever vaccines and other live vaccines is not recommended due to the risk of systemic disease, which may be fatal, especially in immunosuppressed patients.
Overdose
Overdose
Treatment: no antidote is known.
Clinically acceptable toxicity was observed with single doses of up to 5.7 g/m2 IV over 30 minutes every 2 weeks.
In case of suspected overdose, the patient should be under constant medical supervision, including counting the blood count.
If necessary, carry out symptomatic treatment.
Storage conditions
Storage conditions
At 15–30 °C
Shelf life
Shelf life
3 years
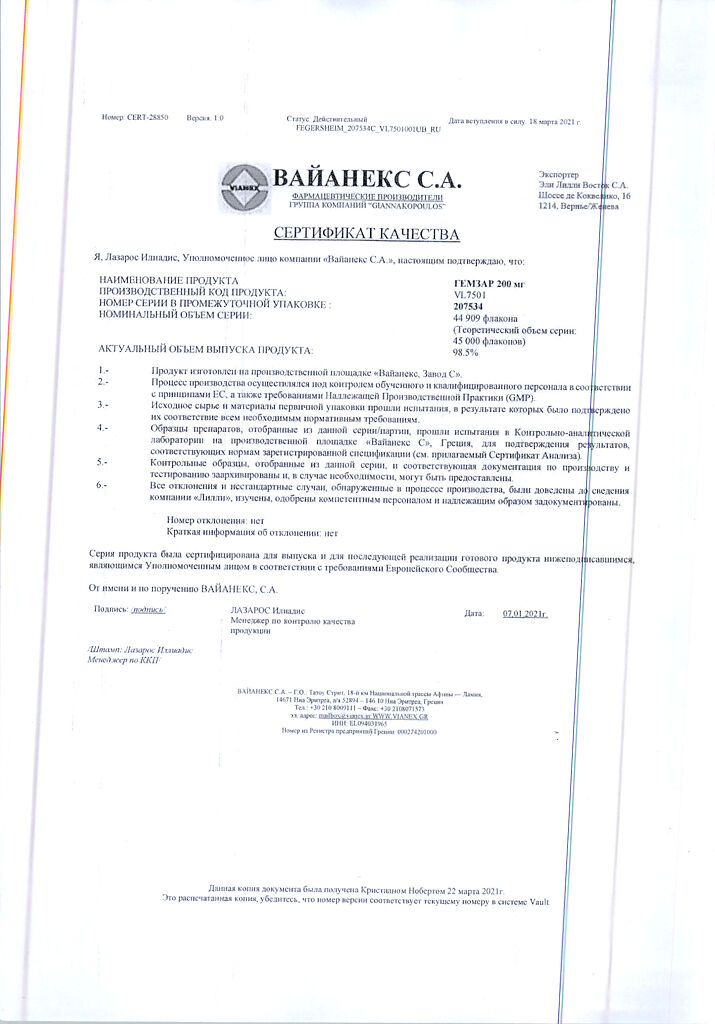
Manufacturer
Manufacturer
Vaynex S.A., Greece
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At 15-30 °C |
| Manufacturer | Weinex S.A., Greece |
| Medication form | lyophilizate |
| Brand | Weinex S.A. |
Other forms…
Related products
Buy Gemzar, lyophilizate 200 mg with delivery to USA, UK, Europe and over 120 other countries.