No products in the cart.
Fortedetrim, capsules 4000 me 30 pcs
€25.81 €21.51
Description
Calcium-phosphorus metabolism regulator.
Pharmacokinetics
Intake
Calciferol (vitamin D3) when taken orally is almost completely absorbed (80%) in the small intestine. Maximum concentration in tissues is reached after 4-5 hours, after which the concentration decreases slightly, remaining constant for a long time. After a single oral administration of colecalciferol the maximum concentration in serum of the basic form is reached after about 7 days.
Distribution
Calciferol accumulates in the liver, bones, skeletal muscles, kidneys, adrenal glands, myocardium, adipose tissue. Maximum concentration in the tissue is reached after 4-5 hours, after which the concentration decreases slightly, remaining constant for a long time.
It is subjected to intestinal-hepatic recirculation. Serum concentrations of the inactive metabolite 25-hydroxycalciferol (25(OH)D3, calcidiol) may be increased for several months after high doses of colocalciferol. Hypercalcemia caused by overdose may persist for several weeks.
Metabolism
Calciferol binds to plasma alpha-2-globulins and partially to albumin and is transported to the liver, where microsomal hydroxylation occurs to form the inactive metabolite 25-hydroxycalciferol (25(OH)D3, calcidiol).
The concentration of calcidiol circulating in the blood is an indicator of vitamin D levels in the body. Calcidiol undergoes re-hydroxylation in the kidneys to form the dominant active metabolite 1,25 hydroxycalciferol (1,25(OH)2D3, calcitriol).
Elimination
25(OH)D3 is slowly excreted with a half-life of about 50 days. The main way of excretion of colecalciferol, as well as its metabolites is bile (feces), and at least 2% of these substances are excreted by the kidneys. Colecalciferol penetrates the placental barrier and passes into breast milk.
Pharmacodynamics
Vitamin D3 is the natural form of vitamin D, which is formed in humans in the skin by the action of sunlight. Compared with vitamin D2, it is characterized by 25% higher activity.
Vitamin D binds to a specific vitamin D receptor (VDR) that regulates the expression of many genes, including the TRPV6 ion channel genes (provides calcium absorption in the intestine), CALB1 (calbindin; provides calcium transport into the bloodstream), BGLAP (osteocalcin; provides bone mineralization and calcium homeostasis), SPP1 (osteopontin; regulates osteoclast migration), REN (renin; provides blood pressure regulation, being a key element of renin-angiotensin-aldosterone regulation system), IGFBP (insulin-like growth factor binding protein; enhances the action of insulin-like growth factor), FGF23 and FGFR23 (fibroblast growth factor 23; regulates calcium levels, phosphate anion, fibroblast cell division processes), TGFB1 (transforming growth factor beta-1; regulates cell division and differentiation processes of osteocytes, chondrocytes, fibroblasts and keratinocytes), LRP2 (LDL-receptor-related protein 2; mediates endocytosis of low-density lipoproteins), INSR (insulin receptor; provides insulin effects on all cell types).
Vitamin D3 is an active anti-rachitis factor. The most important function of vitamin D3 is to regulate calcium and phosphate metabolism, which promotes proper mineralization and skeletal growth.
Calciferol plays an essential role in the absorption of calcium and phosphate in the intestine, in the transport of mineral salts and in the calcification of bones, and also regulates the excretion of calcium and phosphate by the kidneys.
The concentration of calcium ions in blood determines the muscle tone of skeletal muscles, myocardial function, contributes to nerve stimulation and regulates the process of blood clotting.
Deficiency of vitamin D in food, disorders of its absorption, calcium deficiency, as well as lack of exposure to the sun during rapid growth of children leads to rickets, osteomalacia in adults, pregnant women may show symptoms of tetany, disruption of bone calcification in newborns.
The increased need for vitamin D occurs in women during menopause, as they often develop osteoporosis due to hormonal disorders. Vitamin D has a number of so called extracellular effects.
Vitamin D is involved in the functioning of the immune system by modulating cytokine levels and regulates the division of T-helper lymphocytes and the differentiation of B-lymphocytes. A number of studies have shown a decrease in the incidence of respiratory tract infections with vitamin D supplementation.
It is shown that vitamin D is an important link in homeostasis of the immune system: it prevents autoimmune diseases (diabetes mellitus type 1, multiple sclerosis, rheumatoid arthritis, inflammatory bowel diseases, etc.).
Vitamin D has antiproliferative and pro-differentiating effects, which determine the oncoprotective effect of vitamin D. It is noted that the incidence of some tumors (breast cancer, colon cancer) is increased with low levels of vitamin D in the blood.
Vitamin D is involved in the regulation of carbohydrate and fat metabolism by affecting the synthesis of IRS1 (insulin receptor substrate 1; involved in intracellular pathways of insulin receptor signaling), IGF (insulin-like growth factor; regulates the balance of adipose and muscle tissue), PPAR-δ (activated peroxisome proliferator-activated receptor type δ; promotes recycling of excess cholesterol).
According to epidemiological studies, vitamin D deficiency is associated with the risk of metabolic disorders (metabolic syndrome and type 2 diabetes). Vitamin D receptors and metabolizing enzymes are expressed in arterial vessels, the heart and virtually all cells and tissues relevant to the pathogenesis of cardiovascular disease.
In animal models antiatherosclerotic effects, suppression of renin and prevention of myocardial damage, etc., have been shown. Low levels of vitamin D in humans are associated with adverse cardiovascular risk factors such as diabetes, dyslipidemia, arterial hypertension, and are associated with the risk of cardiovascular accidents, including strokes.
In studies in experimental models of Alzheimer’s disease, vitamin D3 has been shown to reduce amyloid accumulation in the brain and improve cognitive function.
In non-interventional studies in humans, the incidence of dementia and Alzheimer’s disease has been shown to increase with low vitamin D levels and low dietary intake of vitamin D. There has been a worsening of cognitive function and the incidence of Alzheimer’s disease at low levels of vitamin D.
Indications
Indications
Composition
Composition
Capsules – 1 capsule.
How to take, the dosage
How to take, the dosage
Capsules should be taken orally swallowed whole with water, preferably with a main meal.
The treatment of vitamin D deficiency (25(OH)D level ⤠20 ng/mL) in adults is 8000 IU (4 capsules of 2000 IU or 2 capsules of 4000 IU) daily for 8 weeks.
Treatment of vitamin D insufficiency (25(OH)D level is 20-29 ng/mL) in adults is 8000 IU (4 capsules of 2000 IU or 2 capsules of 4000 IU) daily for 4 weeks.
Maintaining normal vitamin D levels (25(OH)D levels â¥30 ng/mL) in adults – 2000 IU (1 capsule) daily.
In long-term treatment, calcium concentrations in blood and urine should be determined regularly, and renal function should be determined by measuring serum creatinine concentration. If necessary, the dose should be adjusted taking into account the serum calcium concentration.
Hepatic diseases
Dose adjustment is not required.
Renal dysfunction
The drug should not be prescribed in patients with severe renal insufficiency.
Interaction
Interaction
Concomitant use of anticonvulsant drugs (such as phenytoin) or barbiturates (and possibly other drugs that induce liver enzymes) may decrease the effectiveness of colocalciferol by increasing the rate of biotransformation of colocalciferol into inactive metabolites.
The concomitant therapy with drugs of glucocorticosteroids may decrease the effectiveness of colocalciferol.
The oral administration of colecalciferol may increase the therapeutic effect and toxic potential of foxglove and other cardiac glycosides (risk of arrhythmia) by developing hypercalcemia. Close medical observation, monitoring of ECG values and plasma and urinary calcium levels, and, if necessary, adjustment of the dose of cardiac glycosides is required.
In case of concomitant therapy with thiazide diuretics, which decrease urinary calcium excretion, monitoring of serum and urinary calcium levels is recommended.
Concomitant treatment with ion exchange resins (such as colestyramine), orlistat preparations, or laxatives (such as paraffin oil) may decrease absorption of colocalciferol in the digestive tract.
The concomitant use of rifampicin and isoniazid may decrease the effectiveness of the drug due to an increased rate of biotransformation of colocalciferol.
The concomitant use of antacids containing magnesium and colecalciferol may increase the concentration of magnesium in the blood.
The concomitant administration of antacids containing aluminum and colecalciferol may increase the concentration of aluminum in the blood, which increases the risk of aluminum toxicity.
Special Instructions
Special Instructions
If other drugs containing colocalciferol are prescribed simultaneously, the dose of colocalciferol contained in Fortedetrim should be taken into account. Additional use of colecalciferol or calcium should only be made under medical supervision.
In this case it is necessary to monitor the calcium concentration in serum and urine. In patients with renal insufficiency treated with Fortedetrim, calcium and phosphate metabolism parameters should be monitored. The drug should not be used in patients with predisposition to calcium nephrolithiasis.
The drug should be used with caution in patients with impaired urinary calcium and phosphate excretion, during treatment with benzothiazidine derivatives and in immobilized patients (risk of hypercalcemia and hypercalciuria). In these patients the plasma and urinary calcium concentrations should be monitored.
The drug should not be used in pseudohypoparathyroidism because during the phase of normal sensitivity to colocalciferol the need for colocalciferol may decrease, which leads to the risk of delayed overdose. In these cases, it is better to use active vitamin D metabolites that allow more precise dosage adjustment.
In long-term treatment with Fortedetrim, plasma and urinary calcium concentrations should be monitored and renal function should be assessed by measuring serum creatinine concentration. This is especially important in elderly patients and in concomitant treatment with cardiac glycosides or diuretics.
If hypercalcemia occurs with Fortedetrim (blood calcium greater than 7.5 mmol/24 h (300 mg/24 h) or if there is evidence of renal dysfunction, the dose should be reduced or discontinued.
Impact on driving and operating machinery
There have been no studies on the effect on driving and operating machinery.
Contraindications
Contraindications
Overdose
Overdose
Symptoms
The threshold of intoxication for colocalciferol varies between 40,000 and 100,000 IU per day for 1-2 months in adults with normal parathyroid gland function. Newborns and young children may be sensitive to much lower concentrations.
Acute and chronic overdose can lead to increased serum and urine phosphorus levels and hypercalcemia, which can be persistent and potentially life-threatening.
Typical changes in biochemical parameters include hypercalcemia, hypercalciuria, and increased serum levels of 25-hydroxycalciferol (25 (OH) D3, calcidiol). Chronic overdose of colecalciferol can lead to calcium deposition in tissues and parenchymatous organs, primarily in the kidneys (urolithiasis, nephrocalcinosis) and blood vessels.
The symptoms are general in nature and appear in the form of nausea, vomiting, also initially as diarrhea, later as constipation, loss of appetite, weakness, headache, muscle and joint pain, muscle weakness, azotemia, constant sleepiness, polydipsia and polyuria and, at the final stage, as dehydration. Colocalciferol overdose may cause ECG changes, heart rhythm disturbances, pancreatitis, and renal failure.
The treatment of overdose
The first thing to do is to stop taking colocalciferol. It takes several weeks to eliminate the hypercalcemia caused by a colocalciferol overdose. Depending on the degree of hypercalcemia, treatment measures include a low- or no-calcium diet, increased fluid intake, forced diuresis with furosemide, and glucocorticosteroids and calcitonin.
When renal function is preserved, calcium concentration can be significantly reduced by infusion of isotonic sodium chloride solution (3-6 liters over 24 hours) with furosemide and, in some cases, also sodium edetate at a dose of 15 mg/kg/h, while monitoring calcium levels and ECG data.
Phosphate infusion should not be used to reduce hypercalcemia caused by colecalciferol overdose because of the risk of metastatic calcification. Hemodialysis (dialysate without calcium) should be performed in oligoanuria.
There is no specific antidote.
Patients are advised to pay attention to the symptoms of possible overdose when taking high doses of the drug for a long time (nausea, vomiting, initially diarrhea, later constipation, loss of appetite, weakness, headache, muscle and joint pain, muscle weakness, persistent somnolence, polydipsia and polyuria).
Pregnancy use
Pregnancy use
Additional information
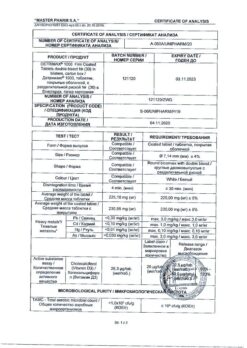
| Manufacturer | Polpharma S.A., Poland |
|---|---|
| Medication form | capsules |
| Brand | Polpharma S.A. |
Related products
Buy Fortedetrim, capsules 4000 me 30 pcs with delivery to USA, UK, Europe and over 120 other countries.