No products in the cart.
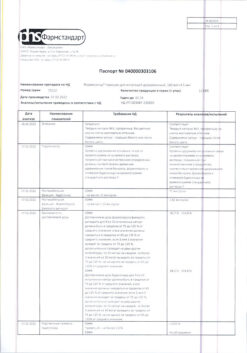
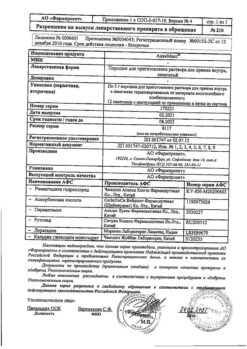
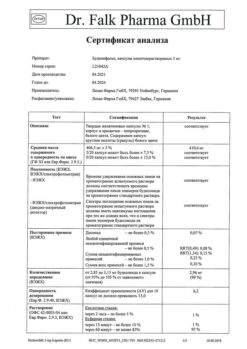
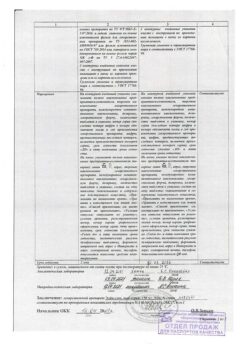
Formisonide, 160 µg+4, 5 µg/dose 60 pcs
€29.27 €24.39
Description
Pharmacotherapeutic group: Bronchodilator combined (p2-adrenomimetic selective + topical glucocorticosteroid)
ATX code: R03AK07
Pharmacodynamics
Formisonide® contains budesonide and formoterol, which have different mechanisms of action and have an additive effect in reducing the frequency of bronchial asthma exacerbations. Special properties of budesonide and formoterol enable to use their combination for relieving attacks/symptoms with anti-inflammatory effect, or as maintenance therapy of bronchial asthma.
Budesonide. Budesonide is a glucocorticosteroid that has a rapid (within hours) and dose-dependent anti-inflammatory effect on the airways after inhalation, reducing the severity of symptoms and the frequency of exacerbations of bronchial asthma. When prescribing inhaled budesonide, there is a lower incidence of serious adverse effects than when using systemic glucocorticosteroids. It reduces the severity of bronchial mucosal edema, mucus production, sputum formation and airway hyperresponsiveness. The exact mechanism of anti-inflammatory action of glucocorticosteroids is unknown.
Formoterol. Formoterol is a selective β2-adrenoreceptor agonist, after inhalation of which there is rapid and prolonged relaxation of bronchial smooth muscle in patients with reversible airway obstruction. The dose-dependent bronchodilator effect occurs within 1-3 minutes after inhalation and persists for at least 12 hours after a single dose.
Clinical efficacy of budesonide + formoterol combination as maintenance therapy
Adding formoterol to budesonide reduces the severity of bronchial asthma symptoms, improves lung function and reduces the frequency of exacerbations of the disease.
The effect of the combined preparation budesonide + formoterol on lung function corresponds to the effect of the combination of budesonide and formoterol monodrugs and exceeds the effect of budesonide alone. In all cases, short-acting beta2-adrenostimulator was used for seizure control. No decrease of antiasthmatic effect with time was noted. The combination drug has good tolerability.
Combination of budesonide and formoterol as maintenance therapy in combination with short-acting β2-adrenoceptor. No decrease of antiasthmatic effect with time has been noted. The drug has good tolerability.
Combined preparation budesonide+formoterol as maintenance therapy in combination with short-acting β2-adrenoceptor for seizure control was administered to patients aged 6 to 11 years for 12 weeks (two inhalations of 80/4.5 mcg/inhalation twice a day). Improvement of pulmonary function and good tolerability of therapy compared to the corresponding dose of budesonide were noted.
Clinical efficacy of budesonide and formoterol combination as maintenance therapy and for seizure/symptom control
In an observational study of 4,447 patients treated with budesonide and formoterol combination therapy as maintenance therapy and for attack/symptom management with anti-inflammatory effects for 6 to 12 months, there was a statistically and clinically significant reduction in the number of severe exacerbations, an increase in the time to first exacerbation compared with the combination of budesonide combined with formoterol or budesonide as maintenance therapy and a beta2-adrenergic stimulant for seizure control. There was also effective control of disease symptoms, pulmonary function, and a reduction in the frequency of prescribing inhalation for seizure control. The development of tolerance to the prescribed therapy was not detected.
In patients who sought medical attention due to the development of an acute attack of bronchial asthma, after inhalation of the combination of budesonide and formoterol the relief of symptoms (bronchospasm) came as quickly and effectively as after prescription of salbutamol and formoterol.
Chronic Obstructive Pulmonary Disease (COPD)
In two studies lasting 12 months in patients with moderate to severe COPD (baseline: prebronchodilatation first-second forced expiratory volume (FEF1) < 50% of proper; median postbronchodilatation PEF1 = 42% of proper) a significant reduction in exacerbation rate was observed with the budesonide/formoterol combination compared with patients treated with formoterol or placebo alone (mean exacerbation rate 1.4 compared with 1.8-1.9 in the placebo/formoterol group). No differences were observed between budesonide combined with formoterol and formoterol on ROB1.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Selection of the dose of active substances included in the drug Formisonide is carried out individually and depending on the severity of the disease. This has to be taken into account not only when starting treatment with combination drugs, but also when changing the dose of the drug.
Bronchial asthma
Formisonide is not indicated for the initial treatment of intermittent and mild persistent bronchial asthma.
If individual patients require a different active ingredient dose combination than Formisonide, p2-adrenomimetics and/or GCS in separate inhalers should be prescribed separately.
Patients should see their physician regularly to monitor the optimal dose of Formisonide. The dose should be reduced to the lowest dose that maintains optimal control of bronchial asthma symptoms. After achieving bronchial asthma control with twice-daily dosing, it is recommended to titrate the dose to the lowest effective dose, up to taking 1 inhalation per day, in those cases where the physician believes the patient requires maintenance therapy in combination with a long-acting bronchodilator. In the next step, if full control is achieved, monotherapy with inhaled glucocorticosteroids may be tried.
There are two approaches to prescribing therapy for bronchial asthma with Formisonide:
A. As maintenance therapy: Formisonide is prescribed for ongoing maintenance therapy in combination with a single short-acting p2-adrenomimetic to control attacks;
B. As maintenance therapy and for seizure control: Formisonide is prescribed both for ongoing maintenance therapy and on demand when symptoms appear.
As maintenance therapy: prescribed in combination with a separate short-acting p2-adrenomimetic for seizure control. Patients must have a separate short-acting P2-adrenomimetic inhaler with them at all times to control attacks.
The increased frequency of use of short-acting P2-adrenomimetics is an indication that overall control of the disease is worsening, and requires reassessment of asthma therapy.
As maintenance therapy and for seizure control, the drug is especially indicated for patients with insufficient asthma control and a need for frequent use of medications for seizure control; if there is a history of bronchial asthma exacerbations that required medical intervention. The patient must have Formisonide on hand at all times to control attacks.
The occurrence of dose-dependent side effects in patients using large amounts of inhalation for seizure management must be monitored closely.
The recommended dose is 2 inhalations per day: 1 inhalation in the morning and evening, or 2 inhalations once a day in the morning only or in the evening only. Some patients may be prescribed a maintenance dose of Formisonide 160 mcg + 4.5 mcg 2 inhalations 2 times a day. If symptoms of bronchial asthma occur, 1 additional inhalation should be prescribed. If symptoms increase further within a few minutes, 1 additional inhalation is prescribed, but not more than 6 inhalations to stop 1 attack.
It is not usually necessary to prescribe more than 8 inhalations per day, but the number of inhalations may be increased to 12 per day for short periods of time. In patients who use more than 8 inhalations per day, a review of therapy is recommended.
Chronic obstructive pulmonary disease: Recommended dose: 2 inhalations 2 times a day.
Particular patient groups:
There are no data on the use of Formisonide in patients with hepatic impairment. Because budesonide and formoterol are eliminated primarily by the kidneys through hepatic metabolism, a slower rate of elimination can be expected in patients with severe hepatic cirrhosis.
There is no need for special selection of the drug dose for elderly patients.
Interaction
Interaction
Special Instructions
Special Instructions
It is recommended that the dose of the drug be gradually reduced before discontinuing treatment, and abrupt withdrawal of treatment is not recommended.
Formisonide is not indicated for initial therapy in the initial stages of treatment of bronchial asthma and COPD.
If therapy is not effective enough or the maximum recommended doses of Formisonide are exceeded, the treatment regimen should be reconsidered.
An increase in the frequency with which bronchodilators are taken as emergency medications indicates a worsening of the course of the underlying disease and is reason to reconsider the treatment tactics for bronchial asthma. An unexpected and progressive worsening of bronchial asthma or COPD symptom control is a potentially life-threatening condition and requires urgent medical intervention. In this situation, consideration should be given to increasing the dose of GCS, i.e., prescribing a course of oral GCS or antibiotic treatment if infection has set in. Patients should always have emergency medications on hand: Formisonide (for patients with bronchial asthma using Formisonide for maintenance therapy and for control of attacks) or p2-adrenomimetic short-acting agents (for patients using Formisonide only for maintenance therapy).
The need for regular maintenance doses of Formisonide should be explained to the patient according to the therapy chosen, even when there are no symptoms of the disease. Inhalation of Formisonide to control attacks should only be given when symptoms occur, but it is not indicated for regular prophylactic use, i.e. before exercise. In such cases, the use of a separate short-acting p2-adrenomimetic is indicated. If the symptoms of bronchial asthma can be controlled, the dose of Formisonide can be gradually reduced, and it is important to constantly monitor the condition of patients. The lowest effective dose should be prescribed (see section “Dosage and administration”).
The treatment with Formisonide should not be started during exacerbation of bronchial asthma.
As with the use of any other inhaled drug, paradoxical bronchospasm may occur with immediate increase in rales after a dose of Formisonide. In this case, treatment with Formisonide should be discontinued, the therapy should be reconsidered and alternative therapy should be prescribed, if necessary.
Any inhaled GCS, particularly if high doses are taken over a prolonged period of time, may cause systemic effects. Systemic effects are less likely to occur with inhaled therapy than with oral GCS. Possible systemic effects include adrenal suppression, decreased bone mineral density, cataracts and glaucoma.
Because of the potential effect of inhaled GCS on bone mineral density special attention should be given to patients taking high doses over a long period of time with risk factors for osteoporosis. Studies of long-term use of inhaled budesonide in adults at a daily dose of 800 micrograms (measured dose) showed no significant effect on bone mineral density. There are no data regarding the effect of higher doses of the drug on bone mineral density.
If there is reason to believe that adrenal function has been impaired on prior systemic GCS therapy, precautions should be taken when transferring patients to Formisonide.
Inhaled budesonide therapy generally minimizes the need for oral GCS, but patients who discontinue oral GCS therapy may have long-term adrenal insufficiency. Patients who in the past required urgent high-dose GCS or received long-term treatment with high-dose inhaled GCS may also be at this risk. It should be remembered about the possibility of residual adrenal dysfunction in such patients in extreme cases and any situations that may cause stress (including surgical interventions). Adequate GCS treatment should be provided in such situations. Depending on the degree of adrenal dysfunction, a specialist may need to be consulted prior to the recommended procedures.
The development of candidal infection of the oral cavity is possible. To reduce the risk, patients are advised to rinse their mouth thoroughly with water after each inhalation of the drug. If oral candidiasis infection develops, local antifungal therapy may be given without discontinuing treatment with Formisonide. Special precautions should be observed in patients with unstable bronchial asthma who use short-acting P2-adrenomimetics to relieve attacks during exacerbation of severe bronchial asthma, because the risk of hypokalemia increases against hypoxia and in other conditions, when the possibility of hypokalemic symptoms increases. In such cases it is recommended to control potassium content in blood serum.
The blood glucose concentration in diabetic patients should be monitored during treatment.
The use of formoterol in a dose greater than 54 mcg/day (over 12 inhalations of Formisonide in doses of 80+4.5 mcg or 160+4.5 mcg or over 6 inhalations of 320+9 mcg) may lead to positive doping tests.
Particulars of action of the drug when withdrawing
Because of the risk of exacerbations, abrupt withdrawal of Formisonide should be avoided, the dose of the drug should be reduced gradually under medical supervision.
Impact on ability to drive or operate moving machinery
In case of adverse reactions such as tremors or muscle cramps, when using Formisonide, patients should refrain from driving or operating machinery as well as from other potentially dangerous activities requiring increased concentration and quick psychomotor reactions.
Contraindications
Contraindications
Side effects
Side effects
There has been no increase in the incidence of adverse reactions when budesonide and formoterol have been coadministered.
The undesirable reactions are distributed according to the frequency of occurrence. The following criteria were used to assess frequency: very common (>1/10), common (1/100 to 1/10), infrequent (1/1000 to 1/100), rare (1/10000 to 1/1000), very rare (<1/10000), (including individual reports).
Infectious and parasitic diseases:
often – rhinopharyngitis, nasal congestion, sinusitis, upper respiratory tract infections, bronchitis, oropharyngeal candidiasis (candidiasis of the oral mucosa and larynx).
Immune system disorders:
rarely – anaphylactic reactions, including angioedema (Quincke’s edema); bronchospasm, including paradoxical.
Endocrine system disorders:
rarely – hypokalemia;
very rarely – hyperglycemia, symptoms of systemic glucocorticosteroid effects (including hypocorticism, hypercorticism).
Psychiatric disorders:
infrequent – psychomotor agitation, restlessness, anxiety, dizziness, sleep disorders,
very rare – depression, behavior disorders, aggressive behavior, nervousness, taste disorders.
Disorders of the central nervous system:
often – headache.
Visual organ disorders:
very rarely – cataracts, glaucoma (with prolonged use of high doses), increased intraocular pressure.
Cardiac disorders:
often – palpitations;
infrequently – tachycardia;
rarely – arrhythmias, including atrial fibrillation, supraventricular tachycardia, extrasystole;
very rarely – angina pectoris, atrial and ventricular tachyarrhythmias.
Vascular disorders:
very rarely – changes of blood pressure (arterial hypotension, arterial hypertension).
Respiratory system, thoracic and mediastinal disorders:
often – irritation in the throat, cough, hoarseness of the voice;
rarely – dysphonia, (disappearing after discontinuing therapy or reducing the dose of the drug).
Gastrointestinal disorders:
often – discomfort in the stomach,
rarely – vomiting,
very rarely – nausea, dysphagia (swallowing disorders).
Skin and subcutaneous tissue disorders:
infrequent – bruising,
rare – hives, itching, dermatitis, rash,
very rare – redness of the skin.
Muscular and connective tissue disorders:
often – tremor,
infrequently – muscle cramps,
rarely – osteoporosis (decreased bone mineral density), back pain.
The systemic effects of inhaled GKS may be observed when taking the drug in high doses for a long time.
The use of p2-adrenomimetics may increase blood levels of insulin, free fatty acids, glycerol, and ketone derivatives.
If any of the side effects listed in the instructions worsen, or if you notice any other manifestations not listed in the instructions, tell your doctor.
Overdose
Overdose
Pregnancy use
Pregnancy use
Similarities
Similarities
Additional information
| Shelf life | 2 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 ° C. Keep out of reach of children. |
| Manufacturer | Pharmstandard-Leksredstva, Russia |
| Medication form | metered inhalation powder |
| Brand | Pharmstandard-Leksredstva |
Other forms…
Related products
Buy Formisonide, 160 µg+4, 5 µg/dose 60 pcs with delivery to USA, UK, Europe and over 120 other countries.