No products in the cart.
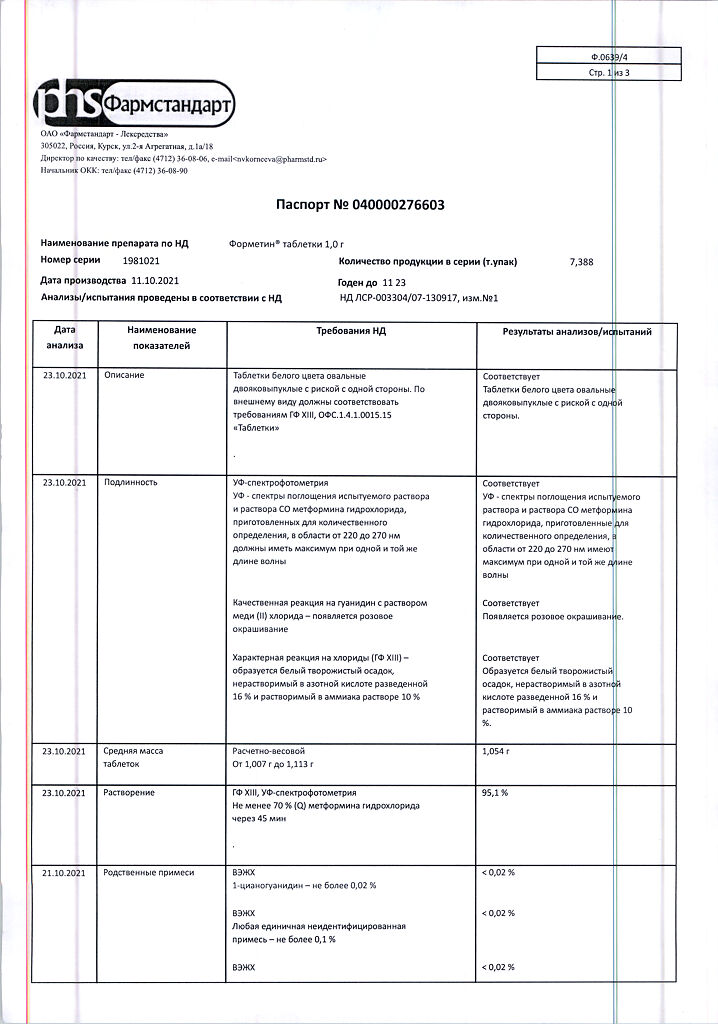
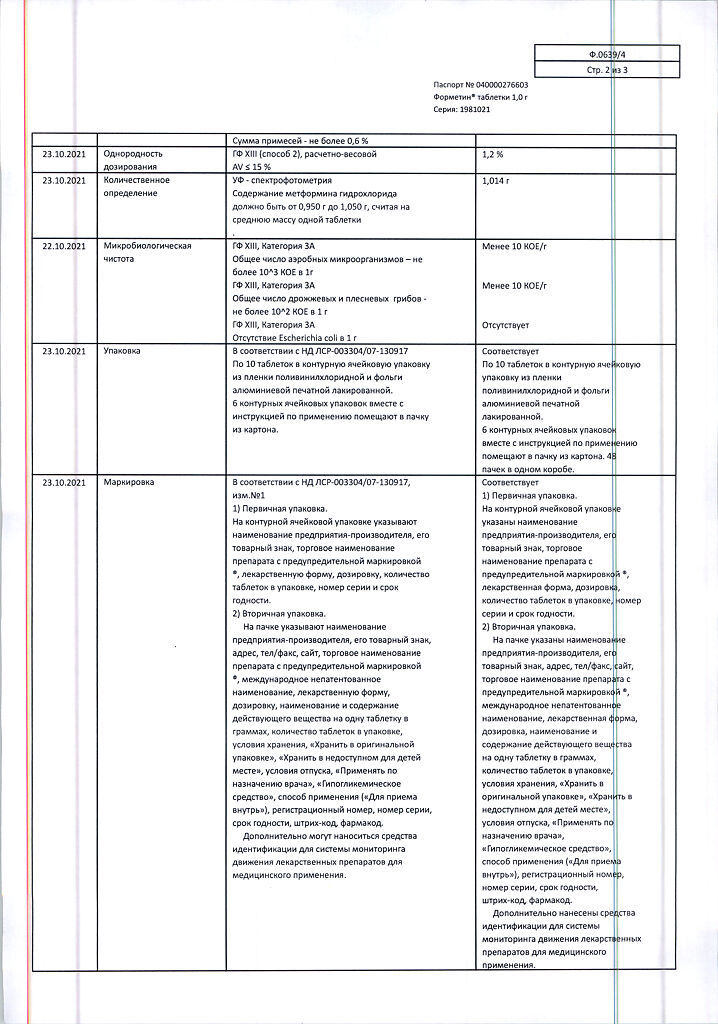
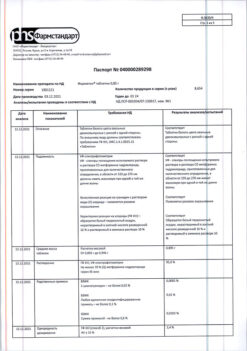
Formetin, 1 g tablets 60 pcs
€5.89 €5.24
Description
Formethine has hypoglycemic effect.
Pharmacodynamics
Metformin inhibits gluconeogenesis in the liver, reduces glucose absorption from the intestine, increases peripheral glucose utilization, and increases tissue sensitivity to insulin.
With this it has no effect on insulin secretion by beta cells of the pancreas, does not cause hypoglycemic reactions. Reduces the level of triglycerides and low-density lipoproteins in the blood. Stabilizes or reduces body weight. Has a fibrinolytic effect due to inhibition of tissue-type plasminogen activator inhibitor.
Pharmacokinetics
After oral administration, metformin is slowly absorbed from the gastrointestinal tract. Bioavailability after a standard dose is 50-60%. Maximum plasma concentration is reached 2.5 hours after oral administration. It practically does not bind with plasma proteins.
It is accumulated in salivary glands, muscles, liver and kidneys. It is excreted unchanged by kidneys. Period of semiejection is 1.5-4.5 hours. Cumulation of the drug is possible in patients with impaired renal function.
Indications
Indications
Type 2 diabetes mellitus, especially in obese patients, with ineffective diet therapy and exercise:
– in adults as monotherapy or in combination with other oral hypoglycemic agents, or with insulin;
– in children over 10 years of age as monotherapy or in combination with insulin.
Prevention of type 2 diabetes mellitus in patients with prediabetes with additional risk factors for developing type 2 diabetes mellitus in whom lifestyle changes have prevented them from achieving adequate glycemic control.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Hypoglycemic agent for oral administration of the biguanide group
ATX code: A10BA02
Pharmacological properties
Pharmacodynamics
Metformin reduces hyperglycemia without leading to the development of hypoglycemia. Unlike sulfonylurea derivatives, it does not stimulate insulin secretion and does not have a hypoglycemic effect in healthy individuals. Increases the sensitivity of peripheral receptors to insulin and the utilization of glucose by cells. Reduces liver glucose production by inhibiting gluconeogenesis and glycogenolysis. Delays the absorption of glucose in the intestines.
Metformin stimulates glycogen synthesis by acting on glycogen synthase. Increases the transport capacity of all types of membrane glucose transporters.
In addition, it has a beneficial effect on lipid metabolism: it reduces the content of total cholesterol, low-density lipoproteins and triglycerides.
While taking metformin, the patient’s body weight either remains stable or decreases moderately.
Clinical studies have also shown the effectiveness of metformin for the prevention of diabetes mellitus in patients with prediabetes with additional risk factors for the development of overt type 2 diabetes mellitus in whom lifestyle changes have not achieved adequate glycemic control.
Pharmacokinetics
Absorption
After oral administration, metformin is absorbed from the gastrointestinal tract quite completely. The proportion of unabsorbed metformin found in feces is 20-30%. The absorption process of metformin is characterized by saturation. It is assumed that the pharmacokinetics of its absorption is not linear. The maximum concentration (Cmax) (approximately 2 µg/ml or 15 µmol) in the blood plasma is achieved after 2.5 hours. When used in recommended doses, the equilibrium concentration of metformin in the blood plasma is achieved within 24-48 hours and, as a rule, does not exceed 1 µg/ml. Absolute bioavailability is 50-60%. With simultaneous food intake, the absorption of metformin is reduced and delayed.
Distribution
Metformin is quickly distributed into tissues and practically does not bind to plasma proteins. Cmax in the blood is lower than Cmax in the blood plasma and is achieved in approximately the same time. Metformin penetrates into red blood cells. It is likely that erythrocytes represent a secondary distribution compartment for metformin. The average volume of distribution is 63-276 l.
Metabolism and excretion
It is metabolized to a very weak extent; no metabolites were found in the body. It is excreted mainly by the kidneys unchanged. Metformin clearance in healthy volunteers is more than 400 ml/min (4 times more than creatinine clearance), indicating the presence of active tubular secretion. The half-life is approximately 6.5 hours.
Renal dysfunction
If renal function is impaired, the clearance of metformin decreases in proportion to the clearance of creatinine; accordingly, the half-life increases, the concentration of metformin in the blood plasma increases, and the risk of its accumulation increases.
Children
With a single dose of more than 500 mg in children, the pharmacokinetic parameters of metformin were similar to those in healthy adults. When repeated doses of 500 mg twice daily were administered for 7 days in children, the Cmax and area under the concentration-time curve (AUC0-1) of metformin were reduced by approximately 33% and 40%, respectively, compared with adult patients with diabetes mellitus who received metformin at a dose of 500 mg twice daily for 14 days. Because the dose of metformin is individualized based on glycemic control, the findings are of limited clinical relevance.
Special instructions
Special instructions
Lactic acidosis
Lactic acidosis is a rare but serious (high mortality unless promptly treated) complication that may occur due to accumulation of metformin. Cases of lactic acidosis when taking metformin occurred mainly in patients with diabetes mellitus with severe renal failure.
Other associated risk factors should be taken into account, such as decompensated diabetes mellitus, ketosis, prolonged fasting, alcoholism, liver failure and any condition associated with severe hypoxia. This may help reduce the incidence of lactic acidosis. The risk of developing lactic acidosis should be taken into account when nonspecific signs appear, such as muscle cramps accompanied by dyspeptic disorders, abdominal pain and severe asthenia.
Lactic acidosis is characterized by acidotic shortness of breath, abdominal pain and hypothermia followed by coma. Diagnostic laboratory parameters are a decrease in blood pH (less than 7.25), lactate content in the blood plasma over 5 mmol/l, increased anion gap and lactate/pyruvate ratio. If metabolic acidosis is suspected, stop taking the drug and consult a doctor immediately.
Surgical operations
The use of metformin should be discontinued 48 hours before elective surgery and can be continued no earlier than 48 hours after, provided that renal function has been found to be normal during the examination.
Kidney function
Since metformin is excreted by the kidneys, before starting treatment and regularly thereafter, it is necessary to determine creatinine clearance:
– at least once a year in patients with normal renal function;
– at least 2-4 times a year in elderly patients, as well as in patients with creatinine clearance at the lower limit of normal.
In case of creatinine clearance less than 45 ml/min, the use of the drug is contraindicated.
Particular caution should be exercised in case of possible impairment of renal function in elderly patients, with simultaneous use of hypotensive drugs, diuretics or non-steroidal anti-inflammatory drugs.
Heart failure
Patients with heart failure have a higher risk of developing hypoxia and renal failure.
Patients with chronic heart failure should have cardiac and renal function monitored regularly while taking metformin.
Taking metformin in heart failure with unstable hemodynamic parameters is contraindicated.
Children and teenagers
The diagnosis of type 2 diabetes mellitus must be confirmed before starting treatment with metformin.
In clinical studies lasting 1 year, metformin was shown to have no effect on growth and puberty. However, due to the lack of long-term data, careful monitoring of the subsequent effects of metformin on these parameters in children, especially during puberty, is recommended.
Clinical experience with metformin in children aged 10 to 12 years is limited, so the most careful monitoring is necessary in children in this age group.
Other Precautions
Patients are advised to continue to follow a diet with even carbohydrate intake throughout the day. Overweight patients are advised to continue to follow a hypocaloric diet (but not less than 1000 kcal/day).
It is recommended that routine laboratory tests be performed regularly to monitor diabetes mellitus.
Metformin in monotherapy does not cause hypoelicemia, however, it is recommended to exercise caution when using it in combination with insulin or other hypoglycemic agents (for example, sulfonylurea derivatives, repaglinide, etc.).
The use of the drug in patients with prediabetes is recommended in the presence of additional risk factors for the development of type 2 diabetes, which include:
– age less than 60 years;
– body mass index (BMI) >35 kg/m2;
– history of gestational diabetes mellitus;
– family history of diabetes mellitus in first-degree relatives;
– increased concentration of triglycerides;
– reduced concentration of HDL cholesterol;
– arterial hypertension.
Metformin did not affect fertility in male or female rats when administered at doses three times the maximum recommended daily dose for humans.
Impact on the ability to drive vehicles and machinery
Monotherapy with Formetin® does not cause hypoglycemia, and therefore does not affect the ability to drive vehicles and machines. However, patients should be warned about the risk of hypoglycemia when using metformin in combination with other hypoglycemic drugs (sulfonylureas, insulin, repaglinide, etc.).
Active ingredient
Active ingredient
Metformin
Composition
Composition
Composition per tablet:
active ingredient: metformin hydrochloride – 0.500 g; 0.850 g; 1,000 g;
excipients: povidone (medium molecular weight polyvinylpyrrolidone, povidone K-30) – 0.017 g; 0.029 g; 0.034 g; croscarmellose sodium (primellose) – 0.008 g; 0.0136 g; 0.016 g; magnesium stearate – 0.005 g; 0.0084 g; 0.010 g
Pregnancy
Pregnancy
Decompensated diabetes mellitus during pregnancy is associated with an increased risk of birth defects and perinatal mortality. Limited evidence suggests that taking metformin in pregnant women does not increase the risk of birth defects in their children.
When planning pregnancy, as well as in the event of pregnancy while taking metformin for prediabetes and type 2 diabetes mellitus, the drug should be discontinued, and insulin therapy should be prescribed in case of type 2 diabetes mellitus. It is necessary to maintain the blood glucose level at a level closest to normal to reduce the risk of fetal malformations.
Metformin passes into breast milk. No side effects were observed in breastfeeding newborns while taking metformin. However, due to limited data, the use of the drug during breastfeeding is not recommended. The decision to stop breastfeeding should be made taking into account the benefits of breastfeeding and the potential risk of side effects for the baby.
Contraindications
Contraindications
– Hypersensitivity to metformin or to any excipient.
– Diabetic ketoacidosis, diabetic precoma, coma.
– Renal failure or impaired renal function (creatinine clearance less than 45 ml/min),
– Acute conditions that occur with a risk of developing renal dysfunction: -dehydration (with diarrhea, vomiting), severe infectious diseases, shock.
– Clinically pronounced manifestations of acute or chronic diseases that can lead to the development of tissue hypoxia (including acute heart failure, chronic heart failure with unstable hemodynamic parameters, respiratory failure, acute myocardial infarction).
– Major surgical operations and injuries, when insulin therapy is indicated (see section “Special instructions”).
– Liver failure, liver dysfunction.
– Chronic alcoholism, acute alcohol poisoning.
– Pregnancy (see section “Use during pregnancy and breastfeeding”).
– Lactic acidosis (including history).
– Use for less than 48 hours before and within 48 hours after radioisotope or x-ray studies with the introduction of iodine-containing contrast agent (see section “Interaction with other drugs”).
– Following a hypocaloric diet (less than 1000 kcal/day).
With caution
Use the drug:
– in children from 10 to 12 years old;
– in persons over 60 years of age who perform heavy physical work, which is associated with an increased risk of developing lactic acidosis;
– in patients with renal failure (creatinine clearance 45-59 ml/min);
– during breastfeeding.
Side Effects
Side Effects
The frequency of side effects of the drug is assessed as follows: very common: > 1/10;
frequent: > 1/100, < 1/10;
uncommon: > 1/1000, < 1/100;
rare: > 1/10,000, < 1/1000;
very rare: < 1/10,000.
Side effects are presented in order of decreasing importance.
Metabolic and nutritional disorders
Very rare: lactic acidosis (see “Special Instructions”).
With long-term use of metformin, a decrease in the absorption of vitamin B12 may be observed. When megaloblastic anemia is detected, the possibility of such an etiology must be taken into account.
Nervous system disorders
Common: taste disturbance.
Gastrointestinal disorders
Very common: nausea, vomiting, diarrhea, abdominal pain and lack of appetite.
Most often they occur during the initial period of treatment and in most cases resolve spontaneously. To prevent symptoms, it is recommended to take metformin 2 or 3 times a day with or after meals. Slowly increasing the dose may improve gastrointestinal tolerability.
Skin and subcutaneous tissue disorders
Very rare: skin reactions such as erythema, itching, rash.
Disorders of the liver and biliary tract
Very rare: abnormal liver function tests and hepatitis; after discontinuation of metformin, these adverse effects completely disappear.
Published data, post-marketing data, and controlled clinical studies in limited pediatric populations aged 10-16 years indicate that side effects in children are similar in nature and severity to those in adult patients.
Interaction
Interaction
Contraindicated combinations
Iodine-containing radiocontrast agents: against the background of functional renal failure in patients with diabetes mellitus, radiological examination with the use of iodine-containing radiocontrast agents can cause the development of lactic acidosis. Treatment with Formetin® should be discontinued depending on renal function 48 hours before or during an X-ray examination using iodine-containing radiocontrast agents and not resumed earlier than 48 hours after, provided that during the examination renal function was found to be normal.
Combinations not recommended
Alcohol: with acute alcohol intoxication, the risk of developing lactic acidosis increases, especially in the case of:
– insufficient nutrition, adherence to a low-calorie diet;
– liver failure.
While taking the drug, you should avoid drinking alcohol and medications containing ethanol.
Combinations requiring caution
Danazol: simultaneous use of danazol is not recommended to avoid the hyperglycemic effect of the latter. If treatment with danazol is necessary and after stopping the latter, a dose adjustment of Formetin® is required under the control of blood glucose concentrations.
Chlorpromazine: When taken in large doses (100 mg per day), it increases blood glucose concentrations, reducing insulin release. When treated with antipsychotics and after stopping the latter, dose adjustment of the drug is required under the control of blood glucose concentrations.
Glucocorticosteroids (GCS) of systemic and local action reduce glucose tolerance, increase the concentration of glucose in the blood, sometimes causing ketosis. When treating GCS and after stopping the latter, dose adjustment of the drug Formtein® is required under the control of blood glucose concentrations.
Diuretics: Concomitant use of loop diuretics may lead to the development of lactic acidosis due to possible functional renal failure. Formetin® should not be prescribed if creatinine clearance is below 60 ml/min.
Prescribed by injection, beta2-adrenergic agonists: increase the concentration of glucose in the blood due to stimulation of beta2-adrenergic receptors. In this case, monitoring of blood glucose concentration is necessary. If necessary, insulin administration is recommended.
When using the above drugs simultaneously, more frequent monitoring of blood glucose may be required, especially at the beginning of treatment. If necessary, the dose of metformin can be adjusted during treatment and after its cessation.
Antihypertensive drugs, with the exception of angiotensin-converting enzyme inhibitors, can reduce blood glucose concentrations. If necessary, the dose of metformin should be adjusted.
With simultaneous use of the drug Formetin® with sulfonylurea derivatives, insulin, acarbose, and salicylates, hypoglycemia may develop.
Nifedipine increases the absorption and Cmax of metformin.
Cationic drugs (amiloride, digoxin, morphine, procainamide, quinidine, quinine, ranitidine, triamterene, trimethoprim and vancomytium) secreted in the renal tubules compete with metformin for tubular transport systems and may lead to an increase in its Cmax.
The hypoglycemic effect of metformin can be reduced by phenothiazines, glucagon, estrogens, oral contraceptives, phenytoin, sympathomimetics, nicotinic acid, isoniazid, blockers of “slow” calcium channels, sodium levothyroxine.
Concomitant use with cimetidine reduces the rate of excretion of metaphorine, which can lead to the development of lactic acidosis.
In healthy volunteers, with simultaneous use of metformin and propranolol, as well as with the use of metformin and ibuprofen, no changes in their pharmacokinetic parameters were observed.
Metformin may reduce the effect of indirect anticoagulants.
Organic cation transporter substrates 1 and 2 (OCT1 and OCT2).
Metformin is a substrate of organic cations OCT1 and OCT2.
When used together with metformin:
– OCT 1 inhibitors (such as verapamil) may reduce the hypoglycemic effect of metformin;
– OCT 1 inducers (such as rifampicin) can increase the absorption of metformin in the gastrointestinal tract and enhance its hypoglycemic effect;
– OCT2 inhibitors (such as cimetidine, dolutegravir, ranolazine, trimethoprim, vadetanib, isavuconazole) may reduce the renal excretion of metformin and lead to an increase in its plasma concentration;
– OCT1 and OCT2 inhibitors (such as crizotinib, olaparide) can reduce the hypoglycemic effect of metformin.
Overdose
Overdose
When using metformin at a dose of 85 g (42.5 times the maximum daily dose
dose) the development of hypoglycemia was not observed. However, in this case, the development of lactic acidosis was observed. Significant overdose or associated risk factors may lead to the development of lactic acidosis (see “Special Instructions”).
Treatment: if signs of lactic acidosis appear, treatment with the drug must be stopped immediately, the patient must be urgently hospitalized and, having determined the lactate concentration, the diagnosis must be clarified. The most effective measure for removing lactate and metformin from the body is hemodialysis. Symptomatic treatment is also carried out.
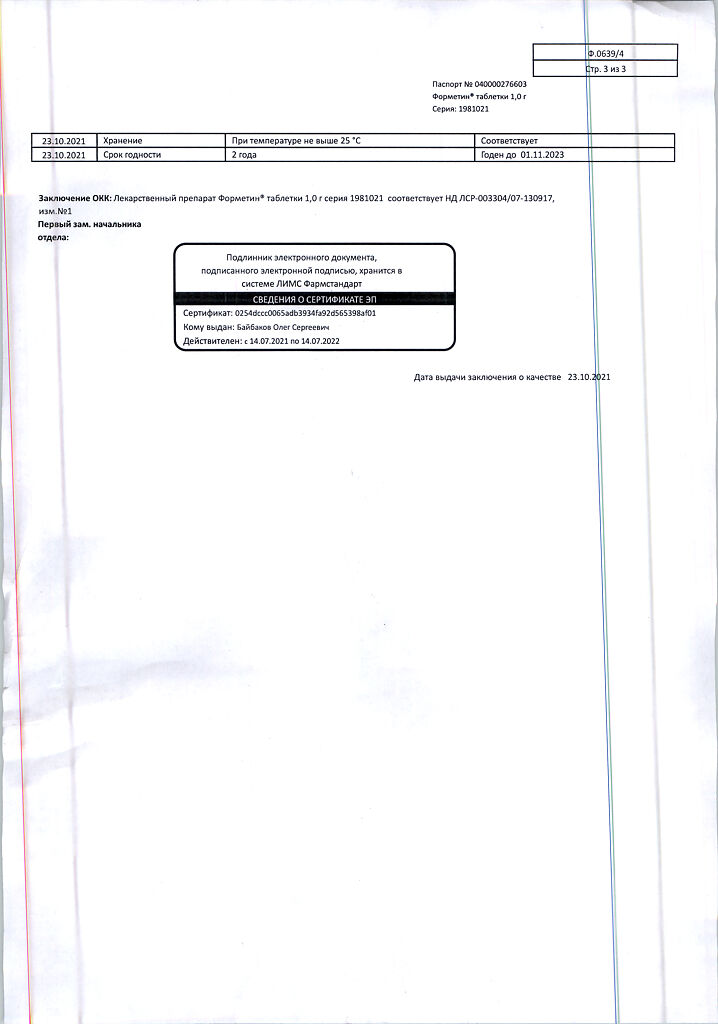
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use after the expiration date indicated on the package.
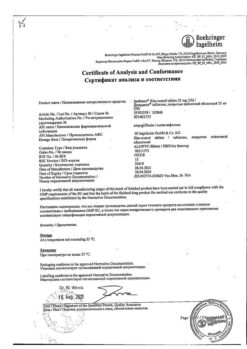
Manufacturer
Manufacturer
Pharmstandard-Leksredstva, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Pharmstandard-Leksredstva, Russia |
| Medication form | pills |
| Brand | Pharmstandard-Leksredstva |
Other forms…
Related products
Buy Formetin, 1 g tablets 60 pcs with delivery to USA, UK, Europe and over 120 other countries.