No products in the cart.
Forciga, 10 mg 30 pcs.
€69.75 €58.12
Description
Pharmacotherapeutic group: hypoglycemic agent for oral use – type 2 sodium-dependent glucose transporter inhibitor
ATX code: A10BK01
Pharmacological properties
Mechanism of action
Dapagliflozin is a potent (inhibition constant (Ki) 0.55 nM), selective reversible inhibitor of sodium-glucose co-transporter type 2 (SGLT2).
Inhibition of SGLT2 by dapagliflozin causes reduction of glucose reabsorption from glomerular filtrate in proximal renal tubules with concomitant reduction of sodium reabsorption, leading to renal glucose excretion and osmotic diuresis. Thus, dapagliflozin increases sodium delivery to the distal tubules, which enhances tubule-glove feedback and decreases intraclavian pressure. This, combined with osmotic diuresis, results in decreased volume overload, decreased blood pressure, and decreased preload and postload, which may have beneficial effects on cardiac remodeling and preserving renal function. Other effects include increased hematocrit and decreased body weight.
The beneficial effects of dapagliflozin on the cardiovascular system and the kidneys are not only due to a decrease in blood glucose concentrations and are not only observed in patients with diabetes. In addition to osmotic diuresis and the associated hemodynamic action resulting from SGLT2 inhibition, secondary effects on myocardial metabolism, ion channels, fibrosis, adipokines and uric acid may be potential mechanisms that provide beneficial effects of dapagliflozin on the cardiovascular system and kidneys.
Dapagliflozin reduces fasting and postprandial plasma glucose concentrations and glycated hemoglobin concentrations by reducing glucose reabsorption in the renal tubules, promoting glucose excretion by the kidneys. Glucose excretion (glucosuric effect) is observed after the first dose of the drug, lasts for the next 24 hours and lasts during the whole therapy. The amount of glucose excreted by the kidneys through this mechanism depends on blood glucose concentration and glomerular filtration rate (GFR). Thus, in patients with normal blood glucose concentration and/or low GFR, against the background of dapagliflozin administration, there is a low propensity to develop hypoglycemia, because the amount of filtered glucose is small and can be reabsorbed by the SGLT1 vector and the unblocked SGLT2 vector. Dapagliflozin does not disrupt normal endogenous glucose production in response to hypoglycemia. The action of dapagliflozin is independent of insulin secretion and insulin sensitivity. In clinical trials, dapagliflozin has improved beta-cell function (HOMA, homeostasis model assessment). SGLT2 is selectively expressed in the kidneys. Dapagliflozin has no effect on other glucose transporters that transport glucose to peripheral tissues and is more than 1,400 times more selective for SGLT2 than for SGLT1, the main transporter in the gut responsible for glucose absorption.
Pharmacodynamics
After dapagliflozin administration in healthy volunteers and patients with type 2 diabetes mellitus (DM2), an increase in the amount of glucose excreted by the kidneys was observed. When dapagliflozin was administered at a dose of 10 mg/day for 12 weeks in patients with T2DM, approximately 70 g of glucose per day was excreted by the kidneys (corresponding to 280 kcal/day). In patients with DM2 who took dapagliflozin at a dose of 10 mg/day for a long time (up to 2 years), glucose excretion was maintained throughout the course of therapy.
Kidney excretion of glucose with dapagliflozin also leads to osmotic diuresis and increased urine volume. The increase in urine volume in patients with DM2 taking dapagliflozin at a dose of 10 mg/day persisted for 12 weeks and was approximately 375 mL/day. The increase in urine volume was accompanied by a small and transient increase in renal sodium excretion, which did not lead to changes in serum sodium concentration.
Clinical efficacy of DM2
The analysis of 13 placebo-controlled studies demonstrated a 3.7 mm Hg reduction in systolic blood pressure (SBP). systolic blood pressure (BP) and diastolic blood pressure (DBP) by 1.8 mm Hg at 24 weeks of dapagliflozin therapy at a dose of 10 mg/day compared with a decrease in BP and BP by 0.5 mm Hg in the placebo group. A similar reduction in blood pressure was observed over 104 weeks of treatment.
The combination therapy of dapagliflozin 10 mg and prolonged-acting exenatide resulted in a significantly greater reduction in BP at 28 weeks of therapy (by 4.3 mm Hg) compared to the reduction in BP with dapagliflozin therapy (by 1.8 mm Hg) and with prolonged-acting exenatide therapy (by 1.2 mm Hg).
. When dapagliflozin was used at a dose of 10 mg/day in patients with DM2 with inadequate glycemic control and arterial hypertension receiving angiotensin II receptor blockers, angiotensin-converting enzyme inhibitors, including in combination with another hypotensive drug, there was a 3.1% decrease in the glycated hemoglobin index and a 4.3 mm Hg decrease in BP. Hg after 12 weeks of therapy compared to placebo.
The effect of dapagliflozin compared with placebo on cardiovascular and renal outcomes when added to current baseline therapy was established in the DECLARE clinical trial conducted in 17160 patients with DM2 and two or more additional cardiovascular risk factors (age ≥55 years in men or ≥60 years in women and one or more of the following: dyslipidemia, hypertension, or tobacco smoking) or with diagnosed cardiovascular disease.
Dapagliflozin 10 mg demonstrated superiority compared with placebo in preventing the primary combined end point, which included hospitalization for heart failure or cardiovascular death (hazard ratio (HR) 0.83 [95% confidence interval (CI) 0.73, 0.95]; p=0.005). The difference in the effect of therapy was due to hospitalization for heart failure (OR 0.73 [95% CI 0.61, 0.88]), with no difference in cardiovascular death (OR 0.98 [95% CI 0.82 to 1.17]).
The benefit of dapagliflozin therapy compared with placebo was observed in patients with and without diagnosed cardiovascular disease, with or without baseline heart failure, and was comparable in key subgroups including age, sex, renal function (rCF), and region.
Dapagliflozin reduced the incidence of combined point events, which included a confirmed sustained decrease in rSKF, end-stage renal failure, death due to renal complications, or cardiovascular death. The difference between the groups was due to a decrease in the number of events of the combined renal outcome endpoint components, which included a sustained decrease in rSKF, end-stage renal failure, and death due to renal complications.
The hazard ratio of time to nephropathy (sustained decrease in rSKF, end-stage renal failure, or death due to renal complications) was 0.53 (95% CI 0.43, 0.66) for dapagliflozin compared with placebo.
Dapagliflozin also reduced the risk of new cases of persistent albuminuria (OR 0.79 [95% CI 0.72, 0.87]) and resulted in greater regression of macroalbuminuria (OR 1.82 [95% CI 1.51, 2.20]) compared with placebo.
Chronic Heart Failure
. The DAPA-HF study involving 4,744 patients with chronic heart failure (New York Heart Association [NYHA] functional class II-IV) with reduced ejection fraction (left ventricular ejection fraction [LVEF] ≤ 40%) was conducted to determine whether dapagliflozin reduced the risk of cardiovascular death and hospitalization for heart failure.
Dapagliflozin reduced the incidence of the primary combined end point, which included cardiovascular death, hospitalization for heart failure, or emergency admission for worsening heart failure (OR 0.74 [95% CI 0.65, 0.85]; p< 0.0001). All three components of the primary combined endpoint individually contributed to the treatment effect (cardiovascular death: OR 0.82 [95% CI 0.69, 0.98], hospitalization for heart failure: OR 0.70 [95% CI 0.59, 0.83], emergency care seeking due to worsening heart failure: OR 0.43 [95% CI 0.20, 0.90]). There were several urgent requests for care due to worsening of the course of heart failure. Dapagliflozin also reduced the incidence of cardiovascular death or hospitalization for heart failure (OR 0.75 [95% CI 0.65, 0.85], p< 0.0001).
Dapagliflozin also reduced the total number of hospitalizations for heart failure (first and recurrent) and cardiovascular death; there were 567 cases in the dapagliflozin group compared with 742 cases in the placebo group (odds ratio 0.75 [95% CI 0.65, 0.88]; p=0.0002).
The incidence of death from any cause was lower in the dapagliflozin therapy group compared with placebo (OR 0.83 [95% CI 0.71, 0.97]).
The results for the primary combined endpoint were comparable in patients with and without heart failure with and without DM2 and in other key subgroups, including heart failure severity, renal function (rCF), age, gender, and region.
Dapagliflozin therapy resulted in a statistically significant and clinically meaningful advantage over placebo for heart failure symptoms, as assessed by change after 8 months from baseline in the Kansas Cardiomyopathy Questionnaire Total Symptom Score (KCCQ-TSS) (probability of advantage 1.18 [95% CI 1.11, 1.26]; p< 0.0001). Symptom frequency and symptom severity contributed to the outcome obtained on therapy efficacy. A benefit was observed in both improvement of heart failure symptoms and prevention of worsening of heart failure symptoms.
Chronic kidney disease
. The effect of dapagliflozin on renal outcomes and cardiovascular mortality in patients with chronic kidney disease was established in the DAPA-CKD study, in which dapagliflozin was compared with placebo when added to standard basic therapy in patients with chronic kidney disease with rCF ≥ 25 to ≤ 75 ml/min/1.73 m2 and albuminuria (urinary albumin/creatinine ratio (urinary A/Cp) ≥200 and ≤5,000 mg/g).
Dapagliflozin was superior to placebo in reducing the incidence of the primary combined endpoint, which included a sustained ≥50% decrease in rCF, achievement of end-stage renal failure, cardiovascular death, or death due to renal complications (OR 0.61 [95% CI 0.51, 0.72]; p< 0.0001).
All four components of the primary combined endpoint individually contributed to the treatment effect. Dapagliflozin also reduced the incidence of the combined endpoint, which included a sustained ≥50% decrease in rCF, end-stage renal failure, or death due to renal complications (OR 0.56 [95% CI 0.45, 0.68], p< 0.0001), the combined end point including cardiovascular death and hospitalization for heart failure (OR 0.71 [95% CI 0.55, 0.92], p=0.0089), and death from any cause (OR 0.69 [95% CI 0.53, 0.88], p=0.0035).
The benefit of dapagliflozin therapy compared with placebo for the primary combined endpoint was comparable in patients with chronic kidney disease with or without DM2 and in other key subgroups, including urinary pSCF and A/Cp values, age, gender, and region.
Pharmacokinetics
Absorption
After oral administration, dapagliflozin is rapidly and completely absorbed in the gastrointestinal tract and may be taken either with or without meals. Maximum plasma concentration of dapagliflozin (Cmax) is usually reached within 2 hours after an empty stomach. Cmax and AUC values (area under the concentration-time curve) increase in proportion to the dose of dapagliflozin. Absolute bioavailability of dapagliflozin at an oral dose of 10 mg is 78%. Food intake had a moderate effect on the pharmacokinetics of dapagliflozin in healthy volunteers. High-fat meal decreased Cmax of dapagliflozin by 50%, prolonged Tmax (time to reach maximum plasma concentration) by approximately 1 hour, but had no effect on AUC compared to fasting meal. These changes are not clinically significant.
Distribution
Dapagliflozin is approximately 91% protein-bound. In patients with various diseases, such as renal or liver dysfunction, this figure did not change.
Metabolism
Dapagliflozin is a C-linked glucoside whose aglycon is bound to glucose by a carbon-carbon bond, which makes it resistant to glucosidases. Mean plasma elimination half-life (T1/2) in healthy volunteers was 12.9 hours after a single oral dapagliflozin dose of 10 mg. Dapagliflozin is metabolized to form mainly the inactive metabolite dapagliflozin-3-O-glucuronide.
After oral administration of 50 mg of 14C-dapagliflozin, 61% of the dose taken is metabolized to dapagliflozin-3-O-glucuronide, which accounts for 42% of total plasma radioactivity (by AUC0-12 h). The unchanged drug accounts for 39% of total plasma radioactivity. The shares of the remaining metabolites individually do not exceed 5% of total plasma radioactivity. Dapagliflozin-3-O-glucuronide and other metabolites have no pharmacological effect. Dapagliflozin-3-O-glucuronide is formed under the action of uridine diphosphate-glucuronosyltransferase 1A9 (UGT1A9) enzyme, which is present in the liver and kidneys, cytochrome CYP isoenzymes are involved in metabolism to a lesser extent.
Elimation
Dapagliflozin and its metabolites are excreted primarily by the kidneys, and only less than 2% are excreted unchanged. After administration of 50 mg of 14C-dapagliflozin, 96% radioactivity was detected – 75% in urine and 21% in feces. Approximately 15% of the radioactivity detected in the feces was from unchanged dapagliflozin.
Pharmacokinetics in special patient groups
Patients with impaired renal function
At equilibrium (mean AUC), systemic exposure of dapagliflozin was 32%, 60%, and 87% higher in patients with DM2 and mild, moderate, or severe renal impairment (determined by yohexol clearance) than in patients with DM2 and normal renal function, respectively. The amount of glucose excreted by the kidneys during the day when dapagliflozin was taken in equilibrium depended on the state of renal function. Patients with DM2 and normal renal function and with mild, moderate, or severe renal dysfunction excreted 85, 52, 18, and 11 g of glucose per day, respectively. No differences were found in the binding of dapagliflozin to proteins in healthy volunteers and in patients with renal impairment of varying degrees of severity. It is unknown whether hemodialysis has an effect on dapagliflozin exposure. The effect of reduced renal function on systemic drug exposure was evaluated using a population-based pharmacokinetic model. The model predicted AUC was higher in patients with chronic kidney disease compared with patients with normal renal function and did not differ significantly in patients with chronic kidney disease with or without DM2, consistent with previous findings.
Patients with impaired hepatic function
In patients with mild to moderate hepatic impairment, the mean Cmax and AUC values of dapagliflozin were 12% and 36% higher, respectively, compared with healthy volunteers. These differences are not clinically significant, therefore no dose adjustment of dapagliflozin in mild to moderate hepatic insufficiency is required (see section “Dosage and administration”). In patients with severe hepatic impairment (Child-Pugh class C) mean values of Cmax and AUC of dapagliflozin were 40% and 67% higher, respectively, compared to healthy volunteers.
Elderly patients (≥65 years)
There was no clinically significant increase in exposure in patients under 70 years of age (unless factors other than age are considered). However, increased exposure can be expected due to decreased renal function associated with age. Exposure data in patients over 70 years of age are insufficient. Gender
In women, the average AUC at equilibrium is 22% higher than in men.
Race
There were no clinically significant differences in systemic exposure among Caucasoid, Negroid and Mongoloid races.
Body weight
Lower values of exposure were noted with increased body weight. Therefore, some increased exposure may be noted in patients with low body weight, and some decreased exposure to dapagliflozin in patients with increased body weight. However, these differences are not clinically significant.
Indications
Indications
Diabetes mellitus type 2
Type 2 diabetes mellitus in adult patients, in addition to diet and exercise to improve glycemic control as:
monotherapy, when the use of metformin is impossible due to intolerance;
combination therapy with metformin, sulfonylurea derivatives (including in combination with metformin), thiazolidinediones, dipeptidyl peptidase 4 (DPP-4) inhibitors (including in combination with metformin); long-acting glucagon-like polypeptide-1 (GLP-1) receptor agonist exenatide in combination with metformin; insulin preparations (including in combination with one or two hypoglycemic drugs for oral administration) in the absence of adequate glycemic control on this therapy;
starting combination therapy with metformin, if this therapy is appropriate.
Type 2 diabetes mellitus in adult patients with established cardiovascular disease or two or more cardiovascular risk factors* to reduce the risk of hospitalization for heart failure.
* age ≥ 55 years in men or ≥ 60 years in women and the presence of at least one risk factor: dyslipidemia, hypertension, smoking.
Chronic heart failure
Chronic heart failure (NYHA functional class II-IV) with reduced ejection fraction in adult patients to reduce the risk of cardiovascular death and hospitalization for heart failure.
Chronic kidney disease
Chronic kidney disease in adults at risk of progression to reduce the risk of sustained decline in eGFR, end-stage renal disease, cardiovascular death, and hospitalization for heart failure.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Hypoglycemic agent for oral use – inhibitor of sodium-dependent glucose transporter type 2
Special instructions
Special instructions
General information
Dapagliflozin is contraindicated in patients with type 1 diabetes mellitus (see subsection
“Diabetic ketoacidosis” below in the text of the section).
Renal dysfunction
Due to limited experience, initiation of treatment with dapagliflozin is contraindicated in patients with GFR < 25 mL/min.
The glucose-lowering efficacy of dapagliflozin is dependent on renal function and is reduced in patients with eGFR less than 45 mL/min/1.73 m2 and is likely absent in patients with severe renal impairment (see Dosage and Administration, Pharmacodynamics, and Pharmacokinetics).
In one study of patients with type 2 diabetes with moderate renal impairment (eGFR < 60 ml/min/1.73 m2), adverse reactions of increased creatinine, phosphorus, parathyroid hormone and hypotension were observed in a higher proportion of patients in the dapagliflozin group than in the placebo group.
Liver dysfunction
Clinical studies have provided limited data on the use of the drug in patients with impaired liver function. Exposure to dapagliflozin is increased in patients with severe hepatic impairment (see sections “Dosage and Administration”, “Precautions” and “Pharmacokinetics”).
Use in patients at risk of decreased blood volume and/or arterial hypotension
In accordance with the mechanism of action, dapagliflozin increases diuresis, which may lead to a slight decrease in blood pressure noted in clinical studies (see section “Pharmacodynamics”). The diuretic effect may be more pronounced in patients with very high blood glucose concentrations.
Caution should be exercised in patients for whom dapagliflozin-induced reductions in blood pressure may pose a risk, such as patients receiving antihypertensive therapy, a history of hypotensive episodes, or elderly patients.
In the case of intercurrent conditions that may lead to a decrease in blood volume (for example, gastrointestinal diseases), careful monitoring of blood volume (for example, physical examination, blood pressure measurement, laboratory tests, including hematocrit and electrolyte concentrations) is recommended. Temporary discontinuation of treatment with dapagliflozin is recommended for patients who develop hypovolemia until it is corrected (see section “Side Effects”).
Diabetic ketoacidosis
Rare cases of diabetic ketoacidosis, including life-threatening and fatal cases, have been reported in patients receiving SGLT2 inhibitors, including dapagliflozin. In some cases, the clinical picture of the condition was atypical, with a moderate, below 14 mmol/l (250 mg/dl), increase in blood glucose concentration.
The risk of diabetic ketoacidosis should be considered if nonspecific symptoms such as nausea, vomiting, anorexia, abdominal pain, excessive thirst, difficulty breathing, confusion, fatigue or drowsiness occur.
If these symptoms occur, patients should be immediately evaluated for ketoacidosis, regardless of blood glucose concentration.
In patients with suspected or diagnosed diabetic ketoacidosis, treatment with dapagliflozin should be discontinued immediately.
Treatment should be suspended in patients hospitalized due to major surgery or acute serious illness. In these patients, it is recommended to monitor the level of ketone bodies. Measuring the concentration of ketone bodies in the blood is preferable to measuring the concentration of ketone bodies in the urine. Treatment with dapagliflozin can be resumed when ketone body concentrations normalize and the patient’s condition stabilizes.
Before prescribing dapagliflozin, consider patient history that may predispose to ketoacidosis.
Patients who may be at increased risk for developing diabetic ketoacidosis include patients with low reserve of beta-cell function (eg, patients with type 2 diabetes with low C-peptide levels or latent autoimmune diabetes of adults (LADA diabetes) or patients with a history of pancreatitis); patients with medical conditions that result in food restriction or severe dehydration; patients who have reduced doses of insulin medications; and patients with an increased need for insulin medications due to acute illness, surgery, or alcohol abuse. Caution should be exercised when using SGLT2 inhibitors in such patients.
In patients with diabetic ketoacidosis that occurs during treatment with an SGLT2 inhibitor, resumption of SGLT2 inhibitor therapy is not recommended unless another clear precipitating factor has been identified and corrected.
In studies of dapagliflozin, diabetic ketoacidosis was common in patients with type 1 diabetes. Dapagliflozin is contraindicated for the treatment of patients with type 1 diabetes mellitus.
Necrotizing perineal fasciitis (Fournier’s gangrene)
Post-marketing cases of necrotizing perineal fasciitis (also called Fournier’s gangrene) have been reported in women and men taking SGLT2 inhibitors (see Adverse Reactions section). This is a rare but serious and potentially life-threatening phenomenon that requires emergency surgery and antibiotics.
Patients are advised to consult a doctor if they experience pain, tenderness, erythema or swelling in the genital or perineal area, accompanied by fever and malaise. It should be remembered that either a urogenital infection or a perineal abscess may precede necrotizing fasciitis.
If Fournier’s gangrene is suspected, use of Forxiga should be discontinued and immediate treatment (including antibiotics and surgical debridement) initiated.
Urinary tract infections
Urinary glucose excretion may be associated with an increased risk of urinary tract infection. Therefore, when treating pyelonephritis or urosepsis, the possibility of suspending dapagliflozin therapy should be considered.
Elderly patients (≥ 65 years)
In elderly patients, the risk of a decrease in blood volume may be increased, and they are more often prescribed diuretics.
Elderly patients are more likely to have impaired renal function and/or be treated with antihypertensive drugs that may cause changes in renal function, such as angiotensin-converting enzyme inhibitors and angiotensin II type 1 receptor blockers. For elderly patients, the same recommendations regarding renal function apply as for other patients (see sections “Dosage and Administration”, “Side Effects” and “Pharmacodynamics”).
Chronic heart failure
Experience with the use of dapagliflozin in patients with chronic heart failure of functional class IV according to the NYHA classification is limited.
Infiltrative cardiomyopathy
The use of dapagliflozin in patients with infiltrative cardiomyopathy has not been studied.
Chronic kidney disease
There is no experience with the use of dapagliflozin for the treatment of chronic kidney disease in patients without type 2 diabetes and albuminuria. Patients with albuminuria may benefit more from treatment with dapagliflozin.
Lower limb amputation
An increase in lower extremity amputations (primarily toes) was observed in long-term clinical studies of SGLT2 inhibitors in patients with type 2 diabetes. It is unknown whether this is an effect of the SGLT2 class of drugs. It is important to recommend ongoing preventive foot care for patients with type 2 diabetes.
Evaluation of urine test results
Due to the drug’s mechanism of action, urine glucose test results will be positive in patients taking Forxiga.
Lactose
The drug contains lactose. This drug is contraindicated in patients with rare hereditary lactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome.
Effect on the ability to drive vehicles and machines No studies have been conducted to study the effect of dapagliflozin on the ability to drive vehicles and machines.
Active ingredient
Active ingredient
Dapagliflozin
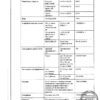
Composition
Composition
1 film-coated tablet, 5 mg contains:
Pregnancy
Pregnancy
Pregnancy
Due to the fact that the use of dapagliflozin during pregnancy has not been studied, the drug is contraindicated during pregnancy. If pregnancy is diagnosed, dapagliflozin therapy should be discontinued.
Breastfeeding period
It is unknown whether dapagliflozin and/or its inactive metabolites are excreted in breast milk. A risk to newborns/infants cannot be excluded. Dapagliflozin is contraindicated during breastfeeding.
Contraindications
Contraindications
• Hypersensitivity or a history of angioedema to dapagliflozin and/or to any of the excipients in the drug.
• Diabetes mellitus type 1.
• Diabetic ketoacidosis.
• Impaired renal function with estimated GFR (eGFR) < 25 ml/min/1.73 m2 (at initiation of therapy).
• End-stage chronic renal failure requiring dialysis.
• Hereditary lactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome.
• Pregnancy and breastfeeding.
• Age under 18 years (due to the lack of clinical data on the effectiveness and safety of dapagliflozin in this age population).
With caution: severe liver failure, urinary tract infections, increased hematocrit.
Side Effects
Side Effects
Security Profile Summary
Type 2 diabetes
In clinical studies, more than 15,000 patients with type 2 diabetes were treated with dapagliflozin.
The primary assessment of safety and tolerability was conducted in a prespecified pooled analysis of 13 short-term (up to 24 weeks) placebo-controlled studies involving 2360 patients receiving dapagliflozin 10 mg and 2295 patients receiving placebo.
In the Cardiovascular Outcomes Study of Dapagliflozin in Type 2 Diabetes (DECLARE Study, see Pharmacodynamics), 8574 patients received dapagliflozin 10 mg and 8569 patients received placebo for a median treatment duration of 48 months. Overall, the mean exposure to dapagliflozin was 30,623 patient-years.
The most common adverse reactions noted in clinical studies were genital infections.
Chronic heart failure
In the Cardiovascular Outcomes Study of Dapagliflozin in Patients with Chronic Heart Failure with Reduced Ejection Fraction (DAPA-HF Study), 2368 patients received dapagliflozin 10 mg and 2368 patients received placebo for a median treatment duration of 18 months. The study population included patients with type 2 diabetes and patients without diabetes, as well as patients with eGFR ≥ 30 ml/min/1.73 m2. In the Dapagliflozin Cardiovascular Outcomes Study in Patients with Chronic Heart Failure with Left Ventricular Ejection Fraction >40% (DELIVER), 3126 patients received dapagliflozin 10 mg and 3127 patients received placebo for a median treatment duration of 27 months. The patient population included patients with and without type 2 diabetes, as well as patients with eGFR ≥ 25 ml/min/1.73 m2.
The overall safety profile of dapagliflozin in patients with chronic heart failure was consistent with the known safety profile of dapagliflozin.
Chronic kidney disease
In the Dapagliflozin Efficacy on Renal Outcomes in Patients with Chronic Kidney Disease (DAPA-CKD) study, 2149 patients received dapagliflozin 10 mg and 2149 patients received placebo for a median treatment duration of 27 months. The study population included patients with type 2 diabetes, without type 2 diabetes, with eGFR ≥ 25 and ≤ 75 ml/min/1.73 m2 and albuminuria (urine A/Cr ≥ 200 and ≤ 5000 mg/g). Treatment was continued if eGFR decreased to less than 25 ml/min/1.73 m2. The overall safety profile of dapagliflozin in patients with chronic kidney disease was consistent with the known safety profile of dapagliflozin.
List of adverse reactions
Adverse reactions observed in placebo-controlled studies1 of dapagliflozin and during post-marketing surveillance are listed below. Adverse reactions were not dose-related. Adverse reactions are distributed according to systemic organ classes indicating the frequency of their occurrence: very often (≥1/10), often (≥1/100, <1/10), infrequently (≥1/1000, <1/100), rarely (≥1/10000, <1/1000), very rarely (<1/10000) and the frequency is unknown (based on available data). data cannot be assessed). Infectious and parasitic diseases: often* – vulvovaginitis, balanitis and associated genital infections*,2,3, urinary tract infection*,2,4; uncommon** – fungal infectious diseases**; very rarely – necrotizing fasciitis of the perineum (Fournier’s gangrene)2,9.
Metabolic and nutritional disorders: very often – hypoglycemia (when used in combination with a sulfonylurea derivative or insulin)2; infrequently** – decrease in blood volume2.5, thirst**; rarely – diabetic ketoacidosis (when used for type 2 diabetes)2,9,11.
Nervous system disorders: often* – dizziness.
Gastrointestinal disorders: uncommon** – constipation**, dry mouth**.
Disorders of the skin and subcutaneous tissues: often* – rash10; very rarely – angioedema.
Disorders of the musculoskeletal system and connective tissue: often* – back pain*.
Renal and urinary tract disorders: often* – dysuria, polyuria*,6; uncommon** – nocturia**; very rarely – tubulointerstitial nephritis.
Disorders of the genital organs and breast: uncommon** – vulvovaginal itching**, genital itching**.
Laboratory and instrumental data: often* – increased hematocrit7, decreased renal clearance of creatinine at the initial stage of therapy2, dyslipidemia8; uncommon** – increased creatinine concentration in the blood at the initial stage of therapy**,2, increased urea concentration in the blood**, decreased body weight**.
1 Data are presented on the use of the drug for up to 24 weeks (short-term therapy), regardless of the use of an additional hypoglycemic drug.
2 See the relevant subsection below for more information.
3 Vulvovaginitis, balanitis and related genital infections include, for example, the following predefined preferred terms: vulvovaginal fungal infection, vaginal infection, balanitis, genital fungal infection, vulvovaginal candidiasis, vulvovaginitis, candidal balanitis, genital candidiasis, genital infection, genital infection in men, penile infection, vulvitis, bacterial vaginitis, vulvar abscess.
4 Urinary tract infection includes the following preferred terms, listed in descending order of frequency: urinary tract infection, cystitis, Escherichia urinary tract infection, genitourinary tract infection, pyelonephritis, trigonitis, urethritis, kidney infection and prostatitis.
5 Decreased blood volume includes, for example, the following predefined preferred terms: dehydration, hypovolemia, hypotension.
6 Polyuria includes the preferred terms: pollakiuria, polyuria, and increased diuresis.
7 The mean change from baseline in hematocrit was 2.30% in the dapagliflozin 10 mg group compared with -0.33% in the placebo group. Hematocrit values >55% were observed in 1.3% of patients receiving dapagliflozin 10 mg compared with 0.4% of patients receiving placebo.
8 The mean percentage changes from baseline in the dapagliflozin 10 mg group and placebo group, respectively, were: total cholesterol 2.5% versus 0.0%; HDL cholesterol 6.0% versus 2.7%; cholesterol-
LDL 2.9% versus -1.0%; triglycerides -2.7% compared to -0.7%.
9 See “Special Instructions” section.
10 Adverse reactions were noted during post-registration surveillance. Rash includes the following preferred terms, listed in order of frequency of occurrence in clinical studies: rash, generalized rash, pruritic rash, macular rash, maculopapular rash, pustular rash, vesicular rash, erythematous rash. In placebo-controlled and active-controlled clinical trials (dapagliflozin group: n = 5936, control group: n = 3403), the incidence of rash was similar in patients treated with dapagliflozin (1.4%) and patients in the control group (1.4%).
11 Noted in the Cardiovascular Outcomes in Patients with Type 2 Diabetes (DECLARE) study. Frequency is based on an annual rate.
*Occurred in ≥ 2% of patients and ≥ 1% more often and in at least 3 more patients in the dapagliflozin 10 mg group compared with placebo.
**Judged by the investigator to be possibly related, likely related, or related to study therapy and observed in ≥0.2% of patients and ≥0.1% more often and in at least 3 more patients in the dapagliflozin 10 mg group compared with placebo.
Description of selected adverse reactions
Vulvovaginitis, balanitis and associated genital infections
In pooled safety data from 13 studies, vulvovaginitis, balanitis, and associated genital infections were reported in 5.5% and 0.6% of patients treated with dapagliflozin 10 mg and placebo, respectively. Most infections were mild or moderate; The initial course of standard therapy was effective, and patients rarely discontinued dapagliflozin. These infections occurred more frequently in women (8.4% and 1.2% with dapagliflozin and placebo, respectively) and were more likely to recur in patients with a history of such infections.
In the DECLARE study, the number of patients with serious adverse events of genital infections was small and balanced: 2 patients each in the dapagliflozin group and the placebo group.
In the DAPA-HF study, there were no patients with serious adverse events such as genital infections in the dapagliflozin group; in the placebo group, a serious adverse event was reported in 1 patient. In the dapagliflozin group, 7 (0.3%) patients experienced adverse events leading to discontinuation of treatment due to genital infections, and no patients in the placebo group. In the DELIVER study, 1 (<0.1%) patient in each treatment group experienced a serious adverse event of genital infection. In the dapagliflozin group, 3 (0.1%) patients experienced adverse events leading to discontinuation of treatment due to genital infections, while in the placebo group there were no patients with such events.
In the DAPA-CKD study, there were 3 (0.1%) patients with serious adverse events of genital infections in the dapagliflozin group and no patients with such events in the placebo group. In the dapagliflozin group, 3 (0.1%) patients experienced adverse events leading to discontinuation of treatment due to genital infections, while in the placebo group there were no patients with such events. Serious adverse events such as genital infections and adverse events such as genital infections leading to treatment discontinuation were not reported in patients without type 2 diabetes.
Necrotizing perineal fasciitis (Fournier’s gangrene)
Post-marketing cases of Fournier’s gangrene have been reported in patients taking SGLT2 inhibitors, including dapagliflozin (see section “Special Instructions”).
In the DECLARE study, in 17,160 patients with type 2 diabetes and a median treatment duration of 48 months, a total of 6 cases of Fournier’s gangrene were reported: one in the dapagliflozin group and 5 in the placebo group.
Hypoglycemia
The incidence of hypoglycemia depended on the type of background therapy used in clinical trials in patients with type 2 diabetes.
In studies of dapagliflozin as monotherapy, as an add-on to metformin, and as an add-on to sitagliptin (with or without metformin) for up to 102 weeks, the incidence of mild hypoglycemia was similar (<5%) in treatment groups including placebo. Severe hypoglycemia was uncommon in all studies and the incidence was comparable between the dapagliflozin and placebo groups.
In studies of dapagliflozin added to a sulfonylurea or insulin, a higher incidence of hypoglycemia was noted (see section
“Interaction with other drugs”).
In a study adding dapagliflozin to glimepiride at weeks 24 and 48, minor episodes of hypoglycemia were reported more often in the dapagliflozin 10 mg and glimepiride group (6.0% and 7.9%, respectively) than in the placebo and glimepiride group (2.1% and 2.1%, respectively).
In a study of adding dapagliflozin to insulin, episodes of significant hypoglycemia were reported in 0.5% and 1.0% of patients receiving dapagliflozin 10 mg and insulin at 24 and 104 weeks, respectively, and in 0.5% of patients receiving placebo and insulin at 24 and 104 weeks. At weeks 24 and 104, minor episodes of hypoglycemia were reported in 40.3% and 53.1% of patients receiving dapagliflozin 10 mg and insulin and in 34.0% and 41.6% of patients receiving placebo and insulin, respectively.
In a study adding dapagliflozin to metformin and a sulfonylurea for up to 24 weeks, no episodes of severe hypoglycemia were reported. Minor episodes of hypoglycemia were reported in 12.8% of patients receiving dapagliflozin 10 mg in combination with metformin and sulfonylureas and in 3.7% of patients receiving placebo in combination with metformin and sulfonylureas.
In the DECLARE study, there was no increased risk of severe hypoglycemia with dapagliflozin compared with placebo. Cases of severe hypoglycemia were reported in 58 (0.7%) patients receiving dapagliflozin and 83 (1.0%) patients receiving placebo.
In the DAPA-HF study, severe hypoglycemia occurred in 4 (0.2%) patients in both the dapagliflozin and placebo groups. In the DELIVER trial, severe hypoglycemia occurred in 6 (0.2%) patients in the dapagliflozin group and 7 (0.2%) patients in the placebo group. Cases of severe hypoglycemia were observed only in patients with type 2 diabetes.
In the DAPA-CKD study, severe hypoglycemia occurred in 14 (0.7%) patients in the dapagliflozin group and in 28 (1.3%) patients in the placebo group and was observed only in patients with type 2 diabetes.
Decrease in BCC
In pooled safety data from 13 studies, adverse reactions indicating a decrease in volume (including reports of dehydration, hypovolemia, or hypotension) were observed in 1.1% and 0.7% of patients taking dapagliflozin 10 mg and placebo, respectively; Serious adverse reactions were reported in <0.2% of patients and were comparable between the dapagliflozin 10 mg and placebo groups (see section 4.4).
In the DECLARE study, the number of patients with events indicating a decrease in blood volume was balanced between treatment groups: 213 (2.5%) and 207 (2.4%) in the dapagliflozin and placebo groups, respectively. Serious adverse events were reported in 81 (0.9%) and 70 (0.8%) patients in the dapagliflozin and placebo groups, respectively. Events were generally balanced between treatment groups for age, diuretic use, blood pressure, and angiotensin-converting enzyme inhibitor/angiotensin II receptor blocker use. In patients with baseline eGFR < 60 mL/min/1.73 m2, there were 19 cases of serious adverse events indicating a decrease in blood volume in patients with baseline eGFR < 60 mL/min/1.73 m2 in the dapagliflozin group and 13 - in the placebo group.
In the DAPA-HF study, events indicating a decrease in blood volume were observed in 170 (7.2%) patients in the dapagliflozin group and 153 (6.5%) in the placebo group. There were fewer patients in the dapagliflozin group (23 [1.0%] patients) with serious adverse events in the form of symptoms indicating a decrease in blood volume compared with the placebo group (38 [1.6%] patients). Results were similar regardless of baseline diabetes and baseline eGFR. In the DELIVER study, the number of patients with serious adverse events in the form of symptoms indicating a decrease in volume was 35 (1.1%) in the dapagliflozin group and 31 (1.0%) in the placebo group.
In the DAPA-CKD study, the number of patients with events indicating a decrease in volume was 120 (5.6%) in the dapagliflozin group and 84 (3.9%) in the placebo group. In the dapagliflozin group, 16 (0.7%) patients experienced serious events in the form of symptoms indicating a decrease in blood volume, and in 15 (0.7%) patients in the placebo group.
Diabetic ketoacidosis in type 2 diabetes
In the DECLARE trial, with a median treatment duration of 48 months, diabetic ketoacidosis was reported in 27 patients in the dapagliflozin 10 mg group and 12 patients in the placebo group. These phenomena occurred evenly throughout the study period. In the dapagliflozin group, of the 27 patients with diabetic ketoacidosis, 22 were receiving concomitant insulin therapy at the time of the event. Factors predisposing to the development of diabetic ketoacidosis were expected for the population with type 2 diabetes (see section “Special Instructions”).
In the DAPA-HF study, cases of diabetic ketoacidosis were reported in 3 patients with type 2 diabetes in the dapagliflozin group; there were no cases of diabetic ketoacidosis in the placebo group. In the DELIVER study, cases of diabetic ketoacidosis were reported in 2 patients with type 2 diabetes in the dapagliflozin group, and no cases of diabetic ketoacidosis were observed in the placebo group.
In the DAPA-CKD study, diabetic ketoacidosis was reported in no patients in the dapagliflozin group, but was reported in 2 patients with type 2 diabetes in the placebo group.
Urinary tract infections
In pooled safety data from 13 studies, urinary tract infections were reported more frequently with dapagliflozin 10 mg than with placebo (4.7% versus 3.5%, respectively; see Precautions). Most infections were mild or moderate; The initial course of standard therapy was effective, and patients rarely discontinued dapagliflozin. These infections occurred more frequently in women, and in patients with a history of such infections they were more likely to recur.
In the DECLARE study, serious urinary tract infections were reported less frequently with dapagliflozin 10 mg compared with placebo: 79 (0.9%) events versus 109 (1.3%) events, respectively.
In the DAPA-HF study, serious adverse events of urinary tract infections were reported in 14 (0.6%) patients in the dapagliflozin group and 17 (0.7%) patients in the placebo group. In the Dapagliflosin and placebo group, there were 5 (0.2%) patients with undesirable phenomena that led to the cessation of treatment due to the development of urinary tract infections. In the Deliver study, serious unwanted phenomena in the form of urinary tract infections were noted in 41 (1.3%) patients in the Dapagliflosin group and 37 (1.2%) patients in the placebo group. In the Dapagliflosin group, in 13 (0.4%) patients, undesirable phenomena were noted that led to the cessation of treatment due to the development of urinary tract infections, and in the placebo group in 9 (0.3%) patients.
In the DAPA-KKD study, serious unwanted phenomena in the form of urinary tract infections were noted in 29 (1.3%) patients in the Dapagliflosin group and in 18 (0.8%) patients in the placebo group. In the Dapagliflosin group there were 8 (0.4%) patients with undesirable phenomena that led to the cessation of treatment due to urinary tract infections, and 3 (0.1%) of the patient in the placebo group. The number of patients without type 2 diabetes, which had serious undesirable phenomena or undesirable phenomena that led to the cessation of treatment due to urinary tract infections, were similar between treatment groups (6 [0.9%] compared to 4 [0.6%] for serious unwanted phenomena; 1 [0.1%] compared to adverse phenomena, which led to the cessation of treatment).
Increasing creatinine concentration
Unwanted reactions associated with an increase in the concentration of creatinine were grouped (for example, a decrease in the renal clearance of creatinine, impaired renal function, an increase in the concentration of creatinine in the blood and a decrease in the SCF). In the combined security data 13, this group of reactions was noted in 3.2% and 1.8% of patients who received Dapagliflosin 10 mg and placebo, respectively. In patients with a normal renal function or mild renal function (initially RSKF ≥ 60 ml/min/1.73 m2), this reaction group was registered in 1.3% and 0.8% of patients receiving 10 mg and placebo dapagliflosin, respectively. These reactions were often observed in patients with the source RSKF ≥ 30 and <60 ml/min/1.73 m2 (18.5% in the Dapagliflosin group of 10 mg compared with 9.3% in the placebo group).
An additional assessment of patients with undesirable phenomena associated with the function of the kidneys showed that most of these patients noted a change in the concentration of creatinine in serum by ≤ 44 μmol/l (≤ 0.5 mg/DL) relative to the initial value. An increase in the concentration of creatinine as a whole was temporary against the background of continuing therapy or reversible after the cessation of therapy.
In the Declare study, which included elderly patients and patients with impaired renal function (RSKF less than 60 ml/min/1.73 m2), RSKF was reduced over time in both groups of treatment. After 1 year of therapy, the average value of the RSKF in the Dapaglyflosin group was slightly lower, and after 4 years of therapy – slightly higher compared to the placebo group.
In the DAPA-HF study, as well as in the Deliver study, RSKF was reduced over time both in the Dapagliflosin group and in the placebo group. In the DAPA-HF study, the initial decrease in the average RSKF value was –4.3 ml/min/1.73 m2 in the Dapagliflosin group and -1.1 ml/min/1.73 m2 in the placebo group. After 20 months, the change in the RSKF regarding the initial value was similar in treatment groups: –5.3 ml/min/1.73 m2 in the Dapagliflosin group and –4.5 ml/min/1.73 m2 in the placebo group. In the Deliver study, a decrease in the average RSKF value after 1 month amounted to –3.7 ml/min/1.73 m2 in the Dapagliflosin group and –0.4 ml/min/1.73 m2 in the placebo group. After 24 months, the change in RSKF regarding the initial value was similar in treatment groups: –4.2 ml/min/1.73 m2 in the Dapagliflosin group and -3.2 ml/min/1.73 m2 in the placebo group.
In a study by DAPA-KKD, RSKF was reduced over time both in the Dapagliflosin group and in the placebo group. The initial (on the 14th day) reduction of the average RSKF was –4.0 ml/min/1.73 m2 in the Dapagliflosin group and –0.8 ml/min/1.73 m2 in the placebo group. After 28 months, the change in the RSKF regarding the initial value was 7.4 ml/min/1.73 m2 in the Dapagliflosin group and -8.6 ml/min/1.73 m2 in the placebo group.
Interaction
Interaction
Pharmacodynamic interaction
Overdose
Overdose
Dapagliflozin is safe and well tolerated in healthy volunteers when administered in single doses up to 500 mg (50 times the recommended dose). Glucose was determined in urine after taking the drug (at least for 5 days after taking a dose of 500 mg), and no cases of dehydration, arterial hypotension, electrolyte imbalance, or clinically significant effect on the QTc interval were detected. The incidence of hypoglycemia was similar to that observed with placebo. In clinical studies in healthy volunteers and patients with type 2 diabetes who took the drug in single doses up to 100 mg (10 times the maximum recommended dose) for 2 weeks, the incidence of hypoglycemia was slightly higher than with placebo and was not dose dependent. The incidence of adverse events, including dehydration or hypotension, was similar to the placebo group, and there were no clinically significant, dose-related changes in laboratory parameters, including serum concentrations of electrolytes and biomarkers of renal function.
In case of overdose, maintenance therapy should be carried out, taking into account the patient’s condition. Elimination of dapagliflozin by hemodialysis has not been studied.
Storage conditions
Storage conditions
At a temperature not higher than 30°C. Keep out of the reach of children.
Shelf life
Shelf life
3 years. Do not use after the expiration date stated on the package.
Manufacturer
Manufacturer
AstraZeneca Industry/AstraZeneca Pharmaceuticals LP, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | At the temperature not more than 30 ° C. Keep out of reach of children. |
| Manufacturer | AstraZeneca Industry/AstraZeneca Pharmaceuticals LP, Russia |
| Medication form | pills |
| Brand | AstraZeneca Industry/AstraZeneca Pharmaceuticals LP |
Related products
Buy Forciga, 10 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.