No products in the cart.
Foradil Combi, 12 mcg+200 mcg 120 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Foradil Combi is a drug with anti-inflammatory and bronchodilatorial action. Formoterol is a selective β 2 -adrenoreceptor agonist. It has a bronchodilator effect in patients with both reversible and irreversible airway obstruction. The action of the drug is fast (within 1-3 minutes) and lasts for 12 hours after inhalation. When the drug is used in therapeutic doses, the effect on the cardiovascular system is minimal and only rarely observed.
Inhibits the release of histamine and leukotrienes from mast cells. Some anti-inflammatory properties of formoterol have been shown in animal experiments, such as the ability to inhibit the development of edema and the accumulation of inflammatory cells.
In studies in humans, Foradyl Combi has been shown to effectively prevent bronchospasm caused by inhaled allergens, exercise, cold air, histamine or methacholine.
Since the bronchodilator effect of Foradil Combi remains pronounced for 12 hours after inhalation, maintenance therapy in which Foradil Combi is prescribed 2 times/day allows in most cases to provide the necessary control of bronchospasm in chronic lung disease both during the day and at night.
In patients with chronic obstructive pulmonary disease (COPD) of stable course formoterol causes rapid onset of bronchodilator effect and improvement of quality of life parameters.
Budesonide is an inhaled glucocorticosteroid (GCS) with almost no systemic action. Budesonide has anti-inflammatory, anti-allergic and immunosuppressive effects. It increases production of lipocortin, which is an inhibitor of phospholipase A2, inhibits the release of arachidonic acid, inhibits the synthesis of products of arachidonic acid metabolism – cyclic endoperoxides and prostaglandins.
Prevent margin accumulation of neutrophils, decreases inflammatory exudation and cytokines production, inhibits macrophages migration, decreases intensity of infiltration and granulation processes, formation of chemotaxis substance (this explains its effectiveness at “late” allergy reactions); inhibits release of inflammatory mediators from mast cells (immediate allergy reaction). It increases quantity of “active” β-adrenoreceptors, restores patient’s response to bronchodilators, allowing reducing frequency of their use, decreases mucous membrane edema of bronchi, mucus production, sputum formation and reduces airway hyperresponsiveness.
Enhances mucociliary transport.
The therapeutic effect of the drug in patients requiring GCS treatment develops on average within 10 days after the start of therapy. When used regularly in patients with bronchial asthma budesonide reduces severity of chronic inflammation in lungs and this way improves lung function, bronchial asthma course, reduces bronchial hyperresponsiveness and prevents exacerbations of disease.
Indications
Indications
Bronchial asthma:
Insufficiently controlled by taking inhaled corticosteroids and short-acting beta 2-agonists as on-demand therapy;
Adequately controlled by inhaled corticosteroids and long-acting beta 2 agonists.
Chronic obstructive pulmonary disease (COPD) (with proven effectiveness of the use of GCS).
Pharmacological effect
Pharmacological effect
Foradil Combi is a drug with anti-inflammatory and bronchodilator effects. Formoterol is a selective β 2 -adrenergic receptor agonist. It has a bronchodilator effect in patients with both reversible and irreversible airway obstruction. The effect of the drug occurs quickly (within 1-3 minutes) and persists for 12 hours after inhalation. When using the drug in therapeutic doses, the effect on the cardiovascular system is minimal and is observed only in rare cases.
Inhibits the release of histamine and leukotrienes from mast cells. Animal experiments have shown some anti-inflammatory properties of formoterol, such as the ability to inhibit the development of edema and the accumulation of inflammatory cells.
In human studies, Foradil Combi has been shown to be effective in preventing bronchospasm caused by inhaled allergens, exercise, cold air, histamine or methacholine.
Since the bronchodilator effect of Foradil Combi remains pronounced for 12 hours after inhalation, maintenance therapy, in which Foradil Combi is prescribed 2 times a day, allows in most cases to provide the necessary control of bronchospasm in chronic lung diseases both during the day and at night.
In patients with stable chronic obstructive pulmonary disease (COPD), formoterol causes a rapid onset of a bronchodilator effect and an improvement in quality of life parameters.
Budesonide is a glucocorticosteroid (GCS) for inhalation use with virtually no systemic effect. Budesonide has anti-inflammatory, antiallergic and immunosuppressive effects. Increases the production of lipocortin, which is an inhibitor of phospholipase A2, inhibits the release of arachidonic acid, inhibits the synthesis of arachidonic acid metabolic products – cyclic endoperoxides and prostaglandins.
Prevents the marginal accumulation of neutrophils, reduces inflammatory exudation and the production of cytokines, inhibits the migration of macrophages, reduces the severity of infiltration and granulation processes, the formation of a chemotaxis substance (which explains the effectiveness in “late” allergy reactions); inhibits the release of inflammatory mediators from mast cells (immediate allergic reaction). Increases the number of “active” β-adrenergic receptors, restores the patient’s response to bronchodilators, allowing them to be reduced in frequency, reduces swelling of the bronchial mucosa, mucus production, sputum formation and reduces airway hyperreactivity.
Increases mucociliary transport.
The therapeutic effect of the drug in patients requiring treatment with GCS develops on average within 10 days after the start of therapy. When used regularly in patients with bronchial asthma, budesonide reduces the severity of chronic inflammation in the lungs, and thus improves pulmonary function, the course of bronchial asthma, reduces bronchial hyperreactivity and prevents exacerbations of the disease.
Special instructions
Special instructions
Formoterol
It has been shown that the use of formoterol improves the quality of life of patients with COPD.
Formoterol belongs to the class of long-acting beta2-agonists. Another long-acting beta2-agonist, salmeterol, was associated with an increased incidence of asthma-related deaths (13 of 13,176 patients) compared with placebo (3 of 13,179 patients). Clinical studies have not been conducted to assess the incidence of deaths associated with bronchial asthma during the use of formoterol.
Anti-inflammatory therapy
In patients with asthma, formoterol should be used only as an adjunctive treatment when symptoms are insufficiently controlled on inhaled corticosteroid monotherapy or when the disease is severe and requires the use of an inhaled corticosteroid and a long-acting β2-adrenergic agonist. Formoterol should not be co-administered with other long-acting β2-adrenergic agonists.
When prescribing formoterol, it is necessary to assess the condition of patients regarding the adequacy of the anti-inflammatory therapy they receive. After starting treatment with formoterol, patients should be advised to continue anti-inflammatory therapy without changes, even if improvement is noted.
To relieve an acute attack of bronchial asthma, short-acting beta2-adrenergic receptor agonists should be used. If the condition suddenly worsens, patients should seek medical help immediately.
Severe exacerbations of bronchial asthma
In clinical studies, with the use of formoterol, there was a slight increase in the incidence of severe exacerbations of bronchial asthma compared to placebo, especially in children 6-12 years of age.
In placebo-controlled clinical trials, patients receiving formoterol for 4 weeks experienced an increased incidence of severe exacerbations of asthma (0.9% with a dosage regimen of 10-12 mcg 2 times a day, 1.9% with 24 mcg 2 times a day) compared with the placebo group (0.3%), especially in children 6-12 years of age.
In two large controlled clinical trials that included 1095 adults and children 12 years of age and older, severe exacerbations of asthma (requiring hospitalization) were more common in patients receiving formoterol 24 mcg twice daily (9/271, 3.3%) compared with formoterol 12 mcg twice daily (1/275, 0.4%), placebo. (2/277, 0.7%) and albuterol (2/272, 0.7%).
When formoterol was used for 16 weeks, another large clinical trial of 2085 adults and adolescents did not find an increase in the incidence of severe asthma exacerbations with increasing formoterol dosage. However, in this study, the incidence of severe exacerbations was higher in the formoterol group (with a dosage regimen of 24 mcg 2 times / day – 2/527, 0.4%, with 12 mcg 2 times / day – 3/527, 0.6%) compared with placebo (1/517, 0.2%). In the open-label phase of this study, when using formoterol at a dose of 12 mcg 2 times a day (if necessary, patients could use up to two additional doses of the drug), the incidence of severe exacerbations of bronchial asthma was 1/517, 0.2%.
In a 52-week multicenter, randomized, double-blind clinical trial that included 518 children aged 6 to 12 years, the incidence of severe asthma exacerbations was higher with formoterol at doses of 24 mcg twice a day (11/171, 6.4%), 12 mcg twice a day (8/171, 4.7%) compared with placebo. (0/176, 0.0%).
However, the results of the above clinical studies do not allow us to quantify the incidence of severe exacerbations of bronchial asthma in different groups.
Hypokalemia
Therapy with beta2-agonists, including formoterol, may result in potentially serious hypokalemia. Hypokalemia may increase susceptibility to the development of arrhythmias.
Because this effect of the drug can be enhanced by hypoxia and concomitant treatment; special caution should be observed in patients with severe bronchial asthma. In these cases, regular monitoring of serum potassium concentration is recommended.
Paradoxical bronchospasm
As with other inhalation therapy, the possibility of developing paradoxical bronchospasm should be taken into account. If it occurs, the drug should be discontinued immediately and alternative treatment should be prescribed.
Impact on the ability to drive vehicles and operate machinery
Patients who experience dizziness or other central nervous system disorders while using the drug formoterol should refrain from driving vehicles or operating machinery during the period of using the drug.
Budesonide
To ensure that budesonide reaches the lungs, it is important to instruct patients to correctly inhale the drug in accordance with the instructions for use.
Patients should be informed that the drug is not intended to relieve attacks, but for regular daily preventive use even in the absence of symptoms of bronchial asthma.
If paradoxical bronchospasm develops, you should immediately stop using budesonide, assess the patient’s condition and, if necessary, prescribe therapy with other drugs. Paradoxical bronchospasm must be immediately relieved with a short-acting beta2-agonist. Patients should always have a short-acting beta2-agonist inhaler available to relieve acute exacerbations of bronchial asthma.
Patients should be informed about the need to consult a doctor if their condition worsens (increased need for short-acting bronchodilators, increased attacks of shortness of breath). In such cases, it is necessary to examine the patient and consider the possibility of increasing the dose of inhaled or oral GCS.
To reduce the risk of developing candidal infections of the oral cavity and pharynx, the patient should thoroughly rinse his mouth with water after each inhalation of the drug. With the development of candidal infection of the oral cavity and pharynx, local antifungal therapy can be performed without stopping treatment with budesonide.
In case of exacerbation of bronchial asthma, the dose of budesonide should be increased or, if necessary, a short course of systemic corticosteroids should be administered and/or antibiotic therapy should be prescribed if infection develops.
It is necessary to regularly monitor the growth dynamics of children and adolescents receiving long-term therapy with inhaled corticosteroids. If growth is delayed, the need to reduce the dose of inhaled corticosteroids (prescribed in the minimum effective dose) and refer the child for consultation to an allergist should be considered. The long-term consequences of growth retardation (impact on final adult height) in children receiving therapy with inhaled corticosteroids have not been studied.
There has been no adequate study of the possibility of compensating for growth retardation in children after discontinuation of therapy with oral corticosteroids.
Budesonide usually has no effect on adrenal function. However, in some patients, with long-term use at recommended daily doses, systemic effects of budesonide may be observed.
When prescribing inhaled GCS in high doses or over a long period of time, systemic adverse reactions may develop (however less often than when using oral GCS), such as suppression of adrenal cortex function, hypercorticism/Cushing’s syndrome, growth retardation in children and adolescents, decreased bone mineral density, hypersensitivity reactions, cataracts, glaucoma and, less commonly, a number of behavioral disorders, including psychomotor hyperactivity, sleep disorders, agitation, depression or aggression (especially in children).
Patients with hormone-independent bronchial asthma
In patients with hormone-independent bronchial asthma, the therapeutic effect of budesonide develops on average within 10 days after the start of treatment. At the beginning of budesonide therapy in patients with increased bronchial secretion, oral corticosteroids can be added to the drug inhalations in a short course (lasting about 2 weeks).
Patients with hormone-dependent bronchial asthma
When switching from oral corticosteroids to inhaled budesonide, patients should be in a relatively stable condition. During the first 10 days, high doses of budesonide are prescribed in combination with previously used oral corticosteroids at the same dose. Then the daily dose of oral corticosteroids begins to be gradually reduced (2.5 mg every month in terms of prednisolone) to the minimum possible level. Treatment with corticosteroids, including budesonide, should not be abruptly interrupted.
The patient’s condition should be carefully monitored in the first months after transition until the hypothalamic-pituitary-adrenal axis has recovered sufficiently to provide an adequate response to stressful situations (for example, trauma, surgery, or severe infection). The function of the hypothalamic-pituitary-adrenal system should be regularly monitored.
In some cases, patients with reduced adrenal cortex function may need additional administration of GCS for oral administration during stressful situations. This category of patients is recommended to always carry a warning card with them, which should indicate that in stressful situations they need additional systemic administration of GCS.
When transferring patients from systemic corticosteroids to inhaled budesonide therapy, reactions such as allergic rhinitis, eczema, lethargy, pain in muscles and joints, and sometimes nausea and vomiting, which were previously suppressed by taking systemic corticosteroids, may occur. Treatment of these reactions should be carried out with antihistamines or local corticosteroids.
Impact on the ability to drive vehicles and operate machinery
There is no data on the effect of budesonide on the ability to drive vehicles and operate machinery. A negative effect of the drug on the ability to drive vehicles and operate machinery is unlikely.
Active ingredient
Active ingredient
Budesonide, Formoterol [set]
Composition
Composition
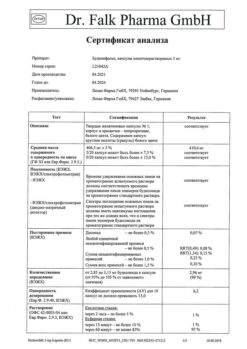
1 capsule of Formoterol contains:
active ingredient:
formoterol fumarate 0.012 mg,
excipients:
lactose monohydrate – up to 25 mg,
capsule shell:
gelatin 100% – 79 mg,
1 capsule of Budesonide contains:
active ingredient:
budesonide 200 mcg,
excipients:
lactose monohydrate – 24.77,
capsule shell:
iron oxide red (E172);
titanium dioxide (E171);
water;
gelatin,
ink composition:
iron oxide black (E172);
shellac;
n-butyl alcohol;
purified water;
soy lecithin liquid;
antifoam compound dc 1510;
methanol 74 OR.
Pregnancy
Pregnancy
Formoterol
The safety of using Foradil Combi during pregnancy and lactation has not yet been established.
Use during pregnancy is possible only if the expected benefit to the mother outweighs the potential risk to the fetus. Formoterol, as well as other beta2-agonists, can slow down the process of labor due to its tocolytic effect (relaxing effect on the smooth muscles of the uterus).
It is not known whether formoterol is excreted into breast milk in humans. Breastfeeding should be stopped while taking Foradil Combi.
Budesonide
Experimental studies on animals revealed a possible teratogenic effect of GCS on the fetus. There is no data on the teratogenic effect of budesonide or on the presence of reproductive toxicity in the drug when used in humans.
Use during pregnancy is possible only if the expected benefit to the mother outweighs the potential risk to the fetus. If it is necessary to carry out GCS therapy during pregnancy, it is preferable to prescribe them in the form of inhalations, because GCS for inhalation have less systemic effect compared to oral GCS.
It is not known whether budesonide is excreted into breast milk in humans.
Fertility
There is no data on the effect of the drug on fertility. Experimental studies on animals did not reveal any effect on fertility with oral formoterol and subcutaneous administration of budesonide.
Contraindications
Contraindications
Lactation period (breastfeeding).
Active pulmonary tuberculosis.
Hereditary galactose intolerance, severe lactase deficiency and glucose-galactose malabsorption syndrome.
Children’s age up to 6 years.
Hypersensitivity to formoterol, budesonide or any other component of Foradil Combi.
Side Effects
Side Effects
Adverse reactions observed in clinical studies are distributed according to frequency of occurrence. The following criteria were used to assess frequency: very often (≥1/10); often (from ≥1/100, <1/10); uncommon (≥1/1000, <1/100); rare (≥1/10,000, <1/1000); very rare (<1/10,000), including isolated reports. Within each group, adverse reactions are distributed in order of decreasing importance.
Formoterol
Allergic reactions: very rarely – hypersensitivity reactions, such as arterial hypotension, urticaria, angioedema, itching, rash.
From the mental side: infrequently – agitation, anxiety, increased excitability, insomnia.
From the nervous system: often – headache, tremor; infrequently – dizziness; very rarely – taste disturbances.
From the cardiovascular system: often – palpitations; infrequently – tachycardia; very rarely – peripheral edema.
From the respiratory system: infrequently – bronchospasm, including paradoxical, irritation of the mucous membrane of the pharynx and larynx.
From the digestive system: infrequently – dryness of the oral mucosa; very rarely – nausea.
From the musculoskeletal system: infrequently – muscle spasm, myalgia.
Adverse reactions according to post-marketing observations when prescribing formoterol (Foradil)
Laboratory and instrumental data: hypokalemia, hyperglycemia, prolongation of the QT interval (during ECG), increased blood pressure (including arterial hypertension).
From the respiratory system: cough.
From the skin and subcutaneous tissues: rash.
From the cardiovascular system: angina pectoris, heart rhythm disturbances, incl. atrial fibrillation, ventricular extrasystoles, tachyarrhythmia.
Budesonide
From the endocrine system: rarely – suppression of adrenal cortex function, Cushing’s syndrome, hypercortisolism, growth retardation in children and adolescents.
From the side of the organ of vision: rarely – cataracts, glaucoma.
Allergic reactions: rarely – hypersensitivity reactions, rash, urticaria, angioedema, itching, contact dermatitis (delayed hypersensitivity reaction type IV).
From the psyche: post-marketing observations – psychomotor hyperactivity, sleep disturbances, anxiety, depression, aggressive behavior, behavioral disorders (especially in children).
From the musculoskeletal system: rarely – a decrease in bone mineral density.
From the respiratory system: often – cough; rarely – paradoxical bronchospasm, candidiasis of the oral mucosa and larynx, pharyngeal irritation, dysphonia, which disappears after stopping budesonide therapy or reducing the dose of the drug.
In a three-year clinical study, when using budesonide in patients with COPD, there was an increase in the incidence of subcutaneous hematomas (10%) and pneumonia (6%) compared with the placebo group (4% and 3%, with p <0.001 and p <0.01, respectively).
Interaction
Interaction
Formoterol
Formoterol (as well as other beta2-agonists) should be administered with caution to patients receiving drugs such as quinidine, disopyramide, procainamide, phenothiazines, antihistamines, macrolides, MAO inhibitors, tricyclic antidepressants, and other drugs known to prolong the QT interval, because in these cases, the effect of adrenergic stimulants on the cardiovascular system may be enhanced. When using drugs that can prolong the QT interval, the risk of ventricular arrhythmias increases.
Concomitant use of other sympathomimetic agents may result in increased side effects of formoterol.
The simultaneous use of xanthine derivatives, corticosteroids or diuretics may enhance the potential hypokalemic effect of beta2-agonists.
Patients receiving anesthesia using halogenated hydrocarbons are at increased risk of developing arrhythmias.
Beta blockers may reduce the effect of formoterol. In this regard, formoterol should not be prescribed together with beta-blockers (including eye drops), unless the use of such a combination of drugs is forced by any emergency reasons.
Budesonide
Use of the drug together with inhibitors of CYP3A4 (for example, itraconazole, ketoconazole, ritonavir, nelfinavir, amiodarone, clarithromycin) may lead to a decrease in the metabolism of budesonide and an increase in its systemic concentration. When prescribing budesonide together with CYP3A4 inhibitors, adrenal function should be regularly monitored and the dose of budesonide adjusted if necessary.
When budesonide is used together with drugs that induce CYP3A4 (for example, rifampicin, phenobarbital, phenytoin), it is possible to increase the metabolism of budesonide and reduce its systemic concentration.
Methandrostenolone and estrogens enhance the effect of budesonide.
Overdose
Overdose
Formoterol
Symptoms: an overdose of formoterol can presumably lead to phenomena characteristic of the excessive action of other beta2-agonists, such as nausea, vomiting, headache, tremor, drowsiness, palpitations, tachycardia, ventricular arrhythmias, metabolic acidosis, hypokalemia, hyperglycemia, arterial hypertension.
Treatment: maintenance and symptomatic therapy is indicated. In serious cases, hospitalization is necessary. The use of beta blockers may be considered, but only with extreme caution and under close medical supervision, as the use of such drugs may cause bronchospasm.
Budesonide
Budesonide has low acute toxicity. A single inhalation of a large amount of the drug can lead to temporary suppression of the function of the hypothalamic-pituitary-adrenal system, which does not require emergency treatment. In case of budesonide overdose, treatment can be continued in doses sufficient to maintain the therapeutic effect.
Storage conditions
Storage conditions
At a temperature not exceeding 25°C.
Shelf life
Shelf life
2 years.
Manufacturer
Manufacturer
Novartis Pharma GmbH, Germany
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25°C. |
| Manufacturer | Novartis Pharma GmbH, Germany |
| Medication form | capsules with powder for inhalation |
| Brand | Novartis Pharma GmbH |
Related products
Buy Foradil Combi, 12 mcg+200 mcg 120 pcs with delivery to USA, UK, Europe and over 120 other countries.