No products in the cart.
Description
Pharmacodynamics
Antitumor drug. Fludarabine phosphate, a component of the drug, is a water-soluble fluorinated nucleotide analogue of the antiviral agent vidarabine, 9-β-D-arabinofuranosyladenine (ara-A), relatively resistant to the action of adenosine deaminase. Fludarabine phosphate is rapidly dephosphorylated to 2-fluoro-ar-A, which is taken up by the cells and then phosphorylated intracellularly by deoxycytidine kinase to active triphosphate (2-fluoro-ar-AATP). This metabolite inhibits ribonucleotide reductase, DNA polymerase, DNA primase, and DNA ligase, which inhibits DNA synthesis. In addition, RNA polymerase II is partially inhibited with a subsequent decrease in protein synthesis. In vitro studies have shown that exposure of lymphocytes of patients with chronic lympholeukemia to 2-fluoroar-A activates the mechanism of intense DNA fragmentation and apoptosis.
Pharmacokinetics
Fludarabine phosphate (2-fluoroura-A-MP) is a water-soluble precursor of fludarabine (2-fluoroura-A). In humans, 2-fluoroar-ar-AMP is rapidly and completely dephosphorylated to the nucleoside 2-fluoroar-ar-A.
Intake
After a single infusion in patients with chronic lympholeukemia of 2-fluoroura-ar-AMP at a dose of 25 mg/m2 for 30 min, the Cmax of 2-fluoroura-A is 3.5-3.7 μmol and is reached by the end of the infusion. Determinations of the corresponding 2-fluoroura-A levels after 5 administrations of the drug showed moderate cumulation with a mean Cmax of 4.4-4.8 μmol by the end of the infusion. During 5 days of treatment, plasma levels of 2-fluoroar-A increased 2-fold. However, cumulation of 2-Fluoro-Ara-A after several cycles of therapy may be insignificant.
Distribution
The binding of 2-Fluoro-Ara-A to plasma proteins is insignificant.
The Cmax of 2-fluoroura-AATP in leukemia lymphocytes of patients with CLL was observed an average of 4 h after infusion and was characterized by a significant variation in the mean value of approximately 20 μmol. The concentration of 2-fluoroar-ATP in leukemia cells was always significantly higher than its maximum concentration in plasma, indicating cumulation of the substance in target cells. A comparison of the pharmacokinetics of 2-fluoroura-A showed an average total plasma clearance of 79±40 ml/min/m2 (2.2±1.2 ml/min/kg) and an average Vd of 83±55 l/m2 (2.4±1.61 l/kg). The findings indicate high individual variability. After IV administration, the plasma concentration of 2-fluoroar-A and AUC increase in a linear dose-dependent manner, whereas T1/2,plasma clearance and Vd remain constant regardless of dose.
Metabolism and excretion
2-Fluoro-Ara-A is delivered to leukemia cells by active transport, where it is rephosphorylated to monophosphate and partially to di- and triphosphate. Triphosphate (2-fluoroura-ATP) is the major intracellular metabolite and is the only known metabolite with cytotoxic activity. The T1/2 of 2-fluoroura-ATP from target cells averaged 15 and 23 h.
After reaching Cmax in plasma, levels of 2-fluoroura-ATP decrease in three phases: the T1/2 in the alpha phase is approximately 5 min, the beta phase 1-2 h and in the terminal phase about 20 h.
2-Fluoro-Ara-A is excreted primarily by the kidneys (40-60% of the IV dose administered).
Pharmacokinetics in Special Clinical Cases
No clear correlation between the pharmacokinetics of 2-fluoro-ar-A and the therapeutic effect of the drug in cancer patients has been found; however, the frequency of neutropenia and changes in hematocrit indicate a dose-dependent nature of the cytotoxic action of fludarabine phosphate in the form of suppression of hematopoiesis.
In persons with decreased renal function, a decrease in total clearance of the drug was observed, indicating the need to reduce the dose.
Indications
Indications
Fludarabine-Teva is used for the treatment of chronic B-cell lymphocytic leukemia in adults with sufficient bone marrow reserve (bone marrow is an organ of the hematopoietic system that carries out the process of creating new blood cells to replace dying and dying ones). Initial treatment of chronic lymphocytic leukemia with Fludarabine-Teva should be started in adults with advanced disease or when signs of disease progression appear.
Chronic B-cell lymphocytic leukemia is a malignant disease characterized by the production of excess numbers of abnormal, immature blood cells called lymphocyte precursors (immune system cells that are a type of white blood cell).
In chronic leukemia, lymphocyte cells mature only partially and may resemble normal white blood cells. But they do not function properly and do not fight infection like normal white blood cells. Such cells (atypical B lymphocytes) gradually accumulate in the bone marrow. They interfere with the production and functioning of normal blood cells. At some point, atypical B lymphocytes leave the bone marrow, their number in the blood increases, and they can enter other organs – the liver, spleen, lymph nodes, causing the appearance of specific symptoms (weakness, pallor, rapid heartbeat, frequent infectious diseases, decreased appetite, weight loss, enlarged liver, spleen). These B lymphocytes reproduce uncontrollably.
Fludarabine-Teva is used to treat low-grade non-Hodgkin lymphoma.
Low-grade non-Hodgkin’s lymphoma is a malignant disease of the lymphatic system (lymphatic vessels, lymph nodes, organs – thymus, spleen). The development of this disease occurs due to mutation of lymphocytes, i.e. when they transform into malignant cells. Lymphocytes are cells of the immune system, which are a type of white blood cell. Most often, the process develops in the lymph nodes. The grade indicates whether the lymphoma is slowly progressive (low grade, slow growing) or aggressive (high grade, fast growing).
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Antitumor drug. Fludarabine phosphate, which is part of the drug, is a water-soluble fluorinated nucleotide analogue of the antiviral agent vidarabine, 9-β-D-arabinofuranosyladenine (ara-A), which is relatively resistant to the action of adenosine deaminase. Fludarabine phosphate is rapidly dephosphorylated to 2-fluoro-ara-A, which is taken up by cells and then intracellularly phosphorylated by deoxycytidine kinase to active triphosphate (2-fluoro-ara-ATP). This metabolite inhibits ribonucleotide reductase, DNA polymerase, DNA primase and DNA ligase, as a result of which DNA synthesis is inhibited. In addition, RNA polymerase II is partially inhibited with a subsequent decrease in protein synthesis. In vitro studies have shown that exposure of lymphocytes from patients with chronic lymphocytic leukemia to 2-fluoro-ara-A activates the mechanism of intense DNA fragmentation and apoptosis.
Pharmacokinetics
Fludarabine phosphate (2-fluoro-ara-AMP) is a water-soluble precursor of fludarabine (2-fluoro-ara-A). In the human body, 2-fluoro-ara-AMP is quickly and completely dephosphorylated to the nucleoside 2-fluoro-ara-A.
Suction
After a single infusion of 2-fluoro-ara-AMP in patients with chronic lymphocytic leukemia at a dose of 25 mg/m2 for 30 minutes, the Cmax of 2-fluoro-ara-A is 3.5-3.7 µmol and is achieved by the end of the infusion. Determinations of the corresponding level of 2-fluoro-ara-A after 5 administrations of the drug showed moderate accumulation with an average Cmax of 4.4-4.8 µmol at the end of the infusion. During the five-day treatment, plasma 2-fluoro-ara-A levels increased 2-fold. However, the accumulation of 2-fluoro-ara-A after several cycles of therapy may be insignificant.
Distribution
The association of 2-fluoro-ara-A with blood plasma proteins is insignificant.
Cmax of 2-fluoro-ara-ATP in leukemic lymphocytes of patients with CLL was observed on average 4 hours after infusion and was characterized by a significant fluctuation in the average value of approximately 20 μmol. The concentration of 2-fluoro-ara-ATP in leukemic cells was always significantly higher than its maximum concentration in plasma, indicating accumulation of the substance in target cells. A comparison of the pharmacokinetics of 2-fluoro-ara-A showed that the average total plasma clearance was 79 ± 40 ml/min/m2 (2.2 ± 1.2 ml/min/kg), and the average Vd was 83 ± 55 l/m2 (2.4 ± 1.61 l/kg). The data obtained indicate high individual variability. After intravenous administration, the plasma concentration of 2-fluoro-ara-A and AUC increase linearly with dose, while T1/2, plasma clearance and Vd remain constant regardless of dose.
Metabolism and excretion
2-fluoro-ara-A is delivered to leukemia cells by active transport, where it is rephosphorylated to monophosphate and partially to di- and triphosphate. Triphosphate (2-fluoro-ara-ATP) is the main intracellular metabolite and the only known metabolite with cytotoxic activity. T1/2 of 2-fluoro-ara-ATP from target cells averaged 15 and 23 hours.
After reaching Cmax in plasma, 2-fluoro-ara-A levels decrease in three phases: T1/2 in the alpha phase is approximately 5 minutes, in the beta phase – 1-2 hours and in the terminal phase about 20 hours.
2-fluoro-ara-A is excreted primarily by the kidneys (40-60% of the administered intravenous dose).
Pharmacokinetics in special clinical situations
There was no clear correlation between the pharmacokinetics of 2-fluoro-ara-A and the therapeutic effect of the drug in cancer patients; however, the frequency of neutropenia and changes in hematocrit indicate a dose-dependent nature of the cytotoxic effect of fludarabine phosphate in the form of inhibition of hematopoiesis.
In individuals with reduced renal function, a decrease in the overall clearance of the drug was observed, indicating the need for dose reduction.
Special instructions
Special instructions
Driving vehicles and working with machinery
Fludarabine-Teva may cause fatigue, weakness, visual disturbances, confusion, agitation and seizures and may therefore affect the ability to drive and operate machines.
Fludarabine-Teva contains sodium
This medicine contains less than 1 mmol (23 mg) sodium per ml, i.e. the drug actually does not contain sodium.
Active ingredient
Active ingredient
Fludarabine
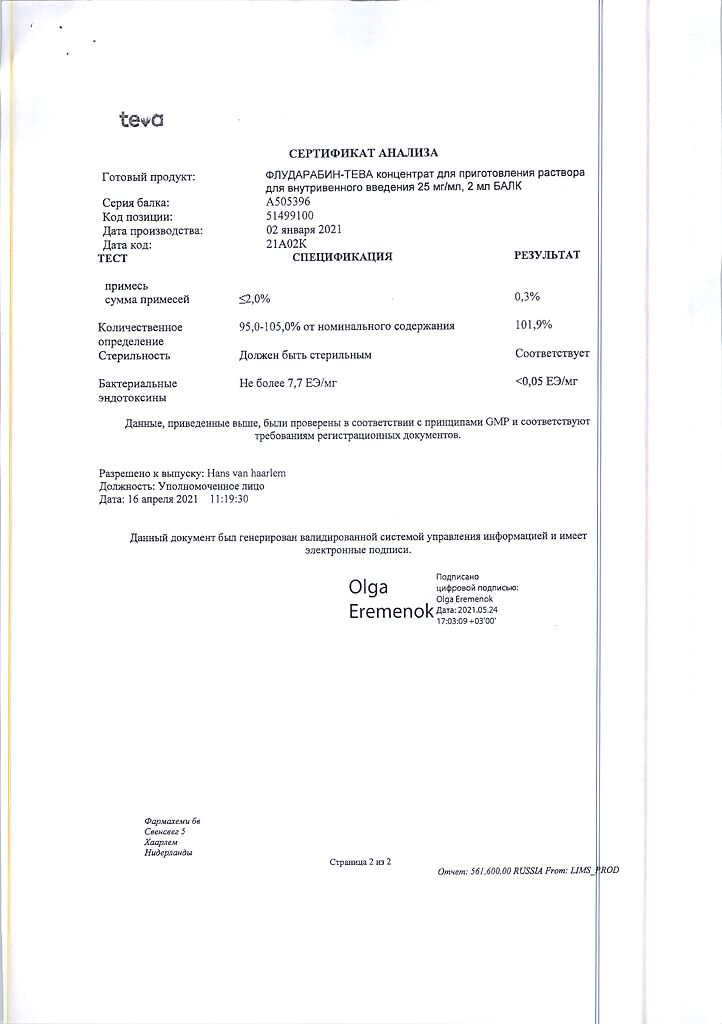
Composition
Composition
The active ingredient is fludarabine.
1 ml of concentrate contains 25 mg of fludarabine (as phosphate).
Each 2 ml vial contains 50 mg fludarabine (as phosphate).
Other ingredients (excipients): mannitol, sodium hydroxide, water for injection.
Pregnancy
Pregnancy
You should tell your doctor if you are pregnant, think you are pregnant, or are trying to become pregnant, so your doctor can decide whether Fludarabine-Teva is right for you.
Men and women of childbearing age should use effective contraception during treatment and for at least 6 months after treatment. It is possible that Fludarabine-Teva may harm the fetus. Your doctor will carefully consider the benefits of treatment against the potential risks to your unborn baby and, if you are pregnant, will only prescribe Fludarabine-Teva if absolutely necessary.
You should not take Fludarabine-Teva if you are pregnant because animal studies and limited experience in humans indicate a potential risk of defects in the unborn child. If you are a woman of childbearing age, you should avoid pregnancy. If you become pregnant, you should tell your doctor immediately.
If you are breastfeeding or plan to do so, you should stop breastfeeding before starting treatment with Fludarabine-Teva, and you should not start it while taking Fludarabine-Teva.
Check with your doctor or pharmacist before taking this drug.
Contraindications
Contraindications
Do not use Fludarabine-Teva if:
you are allergic to fludarabine or any of the other ingredients of this medicine (listed in section 6).
you have severe renal failure.
you have any form of anemia (decompensated hemolytic anemia, that is, a lack of red blood cells).
You are breastfeeding.
In this case, do not take Fludarabine-Teva without consulting your doctor.
Special instructions and precautions
Before using Fludarabine-Teva, consult your doctor or pharmacist.
Before taking Fludarabine-Teva, make sure your doctor knows that:
you have allergic reactions to other medications.
you have kidney problems.
You have been diagnosed with a serious illness that may require immediate hospitalization.
you have a weakened immune system.
you have or have had a history of skin cancer.
You suffer from a chronic heart or respiratory disease.
You require a blood transfusion and are taking (or have been treated with) Fludarabine-Teva.
You need stem cell collection and are taking (or have been treated with) Fludarabine-Teva.
During treatment with Fludarabine-Teva, tell your doctor immediately if:
You know of a disorder of the blood-forming organ, or if you have a weakened or suppressed immune system, or have a history of serious infections.
You feel very unwell if you notice an unusual bruise on your skin, if you are bleeding more than usual after an injury, or if you have several infections.
Your urine has a red or brownish tint, or if a rash, blisters, or blisters develop on your skin.
These may be signs of a decreased number of red blood cells (erythrocytes), which may be caused by the disease itself or by treatment. This condition can last up to a year, regardless of whether you have previously taken fludarabine or not. During treatment, the immune system may also perceive its own tissues or red blood cells (red blood cells) as foreign and damage them (this is called an “autoimmune disease”). These conditions can be life-threatening.
If this happens, your doctor will stop treatment and you may be given other treatments, such as irradiated blood transfusions (see below) and adrenocorticoids.
During treatment with Fludarabine-Teva, you will have regular blood tests and be closely monitored by your doctor.
You notice unusual nervous system symptoms, such as blurred vision.
The effect of Fludarabine-Teva on the central nervous system during long-term use is unknown. Patients receiving the recommended dose for up to 26 cycles tolerated treatment successfully. However, cases of blindness, coma and death have been reported in patients receiving doses four times the recommended dose. It was noted that approximately 60 days or more after stopping treatment, patients experienced recovery from coma and restoration of vision.
You have pain in your side, blood in your urine, or decreased urine output.
If your condition is very severe, your body may not be able to eliminate all the waste products from the cells destroyed by Fludarabine-Teva. This is called “tumor lysis syndrome” (the death of large numbers of tumor cells) and can lead to kidney failure and cardiac dysfunction starting in the first week of treatment.
Have you noticed any changes in your skin both during and after treatment?
For patients with renal failure taking fludarabine
If you have kidney problems or are over 65 years of age, you will need to have regular blood tests and/or tests to check your kidney function. If you have kidney failure, this drug is contraindicated for you (see also section 2 and section 3).
For patients with liver failure taking fludarabine
If you have liver failure, you should take this medicine with caution.
Vaccination
If you need a vaccination, discuss this with your doctor as live vaccines should be avoided during and after treatment with Fludarabine-Teva.
Elderly patients
If you are over 75 years of age, your doctor will prescribe Fludarabine-Teva with caution.
Children and teenagers
Do not give the drug to children aged 0 to 18 years due to the risk of ineffectiveness and possible unsafety (the safety and effectiveness of Fludarabine-Teva in children aged 0 to 18 years have not been established).
Side Effects
Side Effects
Like other medicines, this drug can cause side effects, although not everyone gets them. If you don’t know what the side effects listed below mean, ask your doctor to explain them to you.
Some side effects can be life-threatening.
If you notice any of these symptoms, seek medical help immediately.
If you have difficulty breathing, cough or chest pain, with or without fever, these symptoms may be signs of a lung infection.
If you notice unusual bruising on your skin, bleeding more than usual after an injury, or if you get an infection, this may be caused by a decrease in the number of blood cells, which can lead to an increased risk of serious infections. Including the development of opportunistic infections – infections that develop against the background of a damaged, weakened immune system and are caused by microorganisms that usually do not lead to illness in healthy people, including late reactivation of viruses such as herpes zoster.
If you feel pain in your side, notice blood in your urine, or are passing less urine. This may indicate tumor lysis syndrome (see section 2).
If you notice a reaction on the skin and/or mucous membranes resulting in redness, inflammation, blistering and tissue destruction. These may be signs of a serious allergic reaction (Lyell’s syndrome, Stevens-Johnson syndrome).
If you experience rapid heartbeat, which may occur suddenly, or chest pain. This may indicate heart problems.
Other unwanted reactions that may occur:
Very often
(may affect more than 1 in 10 people)
Infections (sometimes serious)
Infections that develop against the background of a damaged, weakened immune system and are caused by microorganisms that usually do not lead to illness in healthy people (opportunistic infections)
Inflammatory changes in the lung tissue (pneumonia), with possible symptoms such as difficulty breathing and/or cough with or without fever
Low platelet count in the blood (thrombocytopenia) with risk of skin bruising and bleeding
Low number of neutrophils (white blood cells or white blood cells) (neutropenia)
Decreased hemoglobin in the blood (anemia), as well as erythrocytes (red blood cells) (erythropenia)
Cough
Vomiting, nausea, diarrhea (frequent bowel movements, in which the stool has a liquid consistency)
High temperature
Fatigue
Weakness
Often
(may affect less than 1 in 10 people)
Other cancers that affect blood cells (myelodysplastic syndrome (a group of diseases in which the hematopoietic cell that gives rise to all blood cells (red blood cells, white blood cells and platelets) is affected), acute myeloid leukemia (a malignant disease of the blood and bone marrow)). Most patients with these conditions were previously, concurrently or later treated with other antineoplastic drugs (alkylating agents, inhibitors topoisomerase) or radiation therapy.
Decreased number of blood cells produced in the bone marrow (myelosuppression)
Lack of appetite when there is a physiological need for nutrition (anorexia)
Damage to peripheral nerves, which may manifest as muscle weakness, loss of coordination, pain, decreased or increased sensitivity in the corresponding area of the nerves (peripheral neuropathy)
Visual impairment
Inflammation of the oral mucosa (stomatitis)
Skin rash
Excessive accumulation of fluid in the body (edema)
Inflammatory lesions of the mouth, pharynx, esophagus and gastrointestinal tract (mucositis)
Feeling cold with goosebumps and muscle tremors (chills)
Feeling of general malaise.
Uncommon
(may affect 1 in 100 people)
Autoimmune disease (see section 2)
Tumor lysis syndrome (see section 2)
Confusion
Development of pathologies in the lungs: formation of fibrous (scar) tissue in the lungs (pulmonary fibrosis), inflammatory process in the lungs (pneumonitis), disturbance of the frequency, rhythm and depth of breathing with a feeling of lack of air or difficulty breathing (shortness of breath)
Bleeding in the stomach or intestines
Abnormal levels of liver or pancreatic enzymes.
Rarely
(may affect 1 in 1000 people)
Disturbances in the lymphatic system due to viral infection (EBV-associated lymphoproliferative disorder)
Profound depression of the central nervous system with loss of consciousness, loss of reactions to external stimuli and disruption of vital functions (coma)
Epileptic seizures
Increased mental and motor activity (excitement)
Blindness
Inflammation or damage to the optic nerve (neuritis or optic neuropathy)
Mechanical failure of the heart to maintain blood circulation (heart failure)
Irregular heartbeat (arrhythmia)
Skin cancer
The appearance of redness, inflammation, blistering and tissue decomposition on the skin and/or mucous membranes (Lyell’s syndrome, Stevens-Johnson syndrome).
Frequency unknown
(cannot be estimated from available data)
Inflammation of the bladder mucosa, characterized by the presence of blood in the urine (hemorrhagic cystitis)
Bleeding from the respiratory tract (pulmonary hemorrhage)
Bleeding in the brain (cerebral hemorrhage).
Interaction
Interaction
Tell your doctor or pharmacist if you are taking, have recently taken, or may start taking other medications. These include over-the-counter medications. The following medications are especially important:
• pentostatin (deoxycoformycin) is a drug that has a lymphocytotoxic effect (has an inhibitory effect on the cell cycle of lymphocytes). Taking these drugs together may cause serious lung problems.
• dipyridamole is an antiplatelet drug that reduces the tendency of platelets to unite/stick together (aggregation), thereby reducing the likelihood of blood clots forming in blood vessels (arteries) and other similar drugs. These drugs may reduce the effectiveness of treatment with Fludarabine-Teva.
• Cytarabine (ara-C) is a drug used to treat chronic lymphocytic leukemia. When Fludarabine-Teva is combined with cytarabine, the concentration of Fludarabine-Teva in malignant cells may increase. However, it has not been shown to affect total blood levels of fludarabine and its elimination from the body.
Storage conditions
Storage conditions
Keep the drug out of the reach of children and so that the child cannot see it. Do not use the drug after the expiration date (shelf life) indicated on the carton or bottle after “Best before:”. The expiration date is the last day of the given month.
Store at a temperature of 2 to 8 °C, protected from light. Do not freeze.
The drug does not contain antimicrobial preservatives. Therefore, from a microbiological point of view, the solution should be used immediately after preparation. If it is not used immediately after preparation, then the person who prepared the solution is responsible for the terms and conditions of storage. Typically, the prepared solution should not be stored for more than 24 hours at a temperature of 2-8 ° C or 8 hours at room temperature.
Do not throw away (pour) the drug down the drain. Ask your pharmacist how to dispose of (destroy) a drug that is no longer needed. These measures will protect the environment.
Shelf life
Shelf life
3 years.
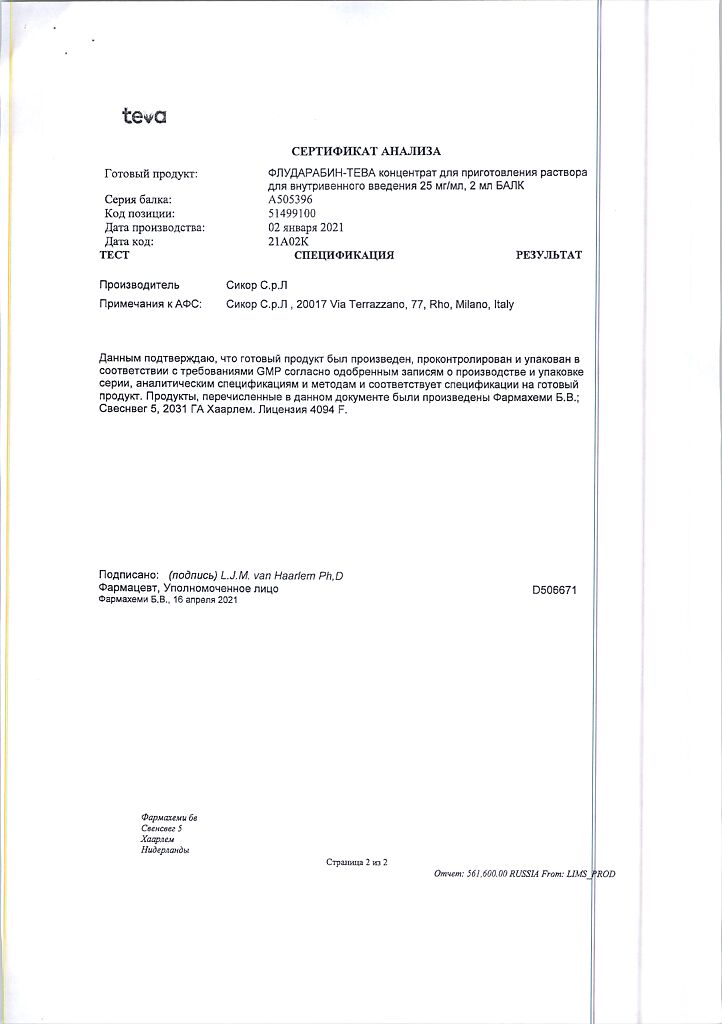
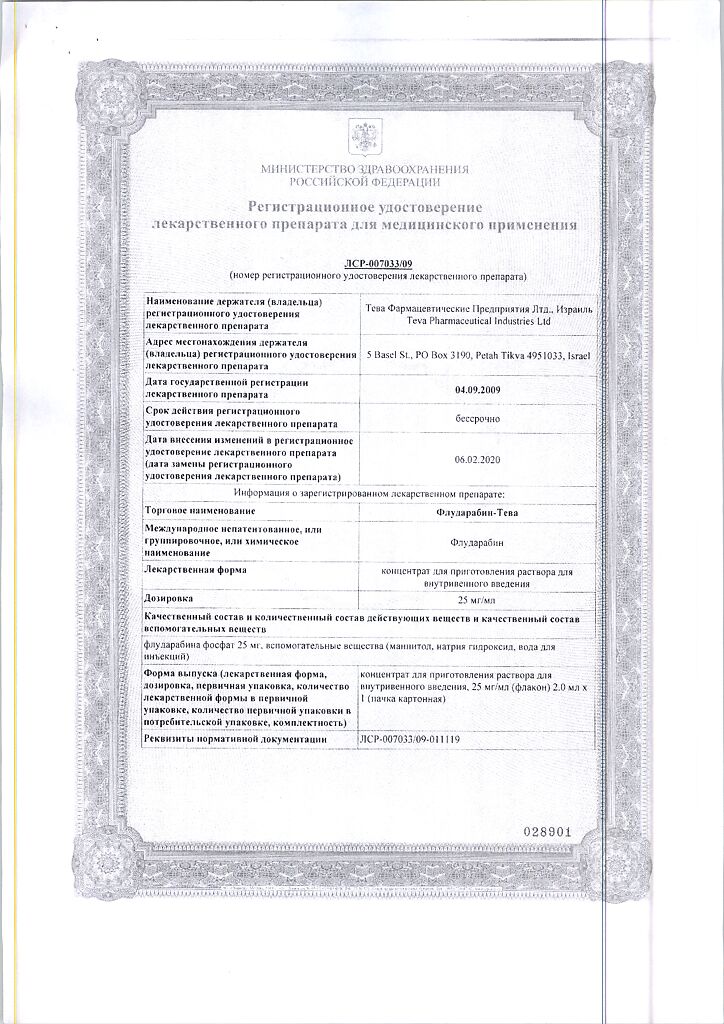
Manufacturer
Manufacturer
Farmahemi B.V., Netherlands
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Keep out of reach of children, protected from light, at 2° to 8°C. |
| Manufacturer | Pharmahemi B.V., The Netherlands |
| Medication form | solution concentrate |
| Brand | Pharmahemi B.V. |
Related products
Buy Fludarabine-Teva, 25 mg/ml concentrate 2 ml with delivery to USA, UK, Europe and over 120 other countries.