No products in the cart.
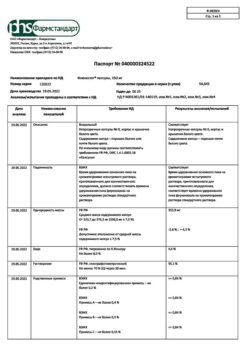
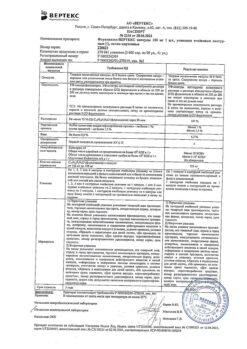
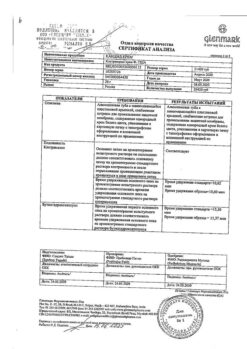
Fluconazole-Vertex, 150 mg capsules 2 pcs
€2.08 €1.89
Description
Antifungal agent, has a highly specific action by inhibiting the activity of cytochrome P450-dependent enzymes of fungi. It blocks transformation of lanosterol of fungi cells into membrane lipid – ergosterol; it increases cell membrane permeability, disrupts its growth and replication.
Fluconazole, being highly selective for cytochrome P450 of fungi, practically does not inhibit these enzymes in human body (in comparison with itraconazole, clotrimazole, econazole and ketoconazole it inhibits cytochrome P450 dependent oxidation processes in human liver microsomes to a lesser extent). It does not have antiadrogenic activity.
It is active in opportunistic mycoses, including those caused by Candida spp. (including generalized candidiasis against immunosuppression), Cryptococcus neoformans and Cossidioides immitis (including intracranial infections), Microsporum spp. and Trichophyton spp.; in endemic mycoses caused by Blastomyces dermatidis, Histoplasma capsulatum (including immunosuppression).
Pharmacokinetics
Fluconazole is well absorbed after oral administration, the absorption rate of fluconazole is not affected by food, its bioavailability is 90%.
The time of maximum concentration after oral administration on an empty stomach of 150 mg of the preparation is 0.5-1.5 h, Cmax is 90% of concentrations in plasma in a dose of 2.5-3.5 mg/l.T1/2 fluconazole is 30 h. Binding to plasma proteins is 11-12%. Plasma concentration is in direct dose dependence. 90% level of equilibrium concentration is reached by 4-5 days of treatment with the drug (when taken once daily).
The administration of a shock dose (on the first day), 2 times the usual daily dose, allows reaching the level of concentration corresponding to 90% of the equilibrium concentration by the second day.
Fluconazole penetrates well into all body fluids. Concentrations of the active substance in breast milk, joint fluid, saliva, sputum and peritoneal fluid are similar to its levels in plasma. Constant values in vaginal secretion are reached 8 hours after oral administration and are maintained at these levels for at least 24 hours.
Fluconazole penetrates cerebrospinal fluid (CSF) well – in fungal meningitis the concentration in CSF is about 85% of its level in plasma. In sweat fluid, epidermis and stratum corneum (selective accumulation), concentrations exceeding serum concentrations are achieved. After oral administration of 150 mg on day 7, the concentration in the stratum corneum of the skin is 23.4 µg/g, and 1 week after the second dose – 7.1 µg/g; the concentration in the nails after 4 months of use at a dose of 150 mg once a week is 4.05 µg/g in healthy and 1.8 µg/g in the affected nails. The volume of distribution approximates the total water content of the body.
It is an inhibitor of CYP2C9 isoenzyme in the liver. It is excreted mainly by the kidneys (80% – unchanged, 11% – as metabolites). Fluconazole clearance is proportional to creatinine clearance. No fluconazole metabolites were detected in peripheral blood.
The pharmacokinetics of fluconazole significantly depends on the functional state of the kidneys, and there is an inverse relationship between the elimination half-life and creatinine clearance. After hemodialysis within 3 hours plasma concentration of fluconazole decreases by 50%.
Indications
Indications
cryptococcosis, including cryptococcal meningitis and other localizations of this infection (including lungs, skin), both in patients with a normal immune response and in patients with various forms of immunosuppression (including in patients with AIDS, with organ transplantation); the drug can be used to prevent cryptococcal infection in patients with AIDS;
generalized candidiasis, including candidemia, disseminated candidiasis and other forms of invasive candidal infections (infections of the peritoneum, endocardium, eyes, respiratory and urinary tract). Treatment can be carried out in patients with malignant neoplasms, patients in intensive care units, patients undergoing a course of cytostatic or immunosuppressive therapy, as well as in the presence of other factors predisposing to the development of candidiasis;
candidiasis of the mucous membranes, including the oral cavity and pharynx (including atrophic candidiasis of the oral cavity associated with wearing dentures), esophagus, non-invasive bronchopulmonary candidiasis, candiduria, skin candidiasis; prevention of relapse of oropharyngeal candidiasis in patients with AIDS;
genital candidiasis: vaginal candidiasis (acute and chronic recurrent), prophylactic use to reduce the frequency of relapses of vaginal candidiasis (3 or more episodes per year); candidal balanitis;
prevention of fungal infections in patients with malignant neoplasms who are predisposed to such infections as a result of cytostatic chemotherapy or radiation therapy;
mycoses of the skin, including mycoses of the feet, body, and groin area; pityriasis versicolor, onychomycosis; skin candidiasis;
deep endemic mycoses, including coccidioidomycosis and histoplasmosis in patients with normal immunity.
Pharmacological effect
Pharmacological effect
An antifungal agent that has a highly specific effect, inhibiting the activity of fungal enzymes dependent on cytochrome P450. Blocks the conversion of lanosterol from fungal cells into the membrane lipid – ergosterol; increases the permeability of the cell membrane, disrupts its growth and replication.
Fluconazole, being highly selective for fungal cytochrome P450, practically does not inhibit these enzymes in the human body (in comparison with itraconazole, clotrimazole, econazole and ketoconazole, it suppresses cytochrome P450-dependent oxidative processes in human liver microsomes to a lesser extent). Does not have antiadrogenic activity.
Active against opportunistic mycoses, incl. caused by Candida spp. (including generalized forms of candidiasis due to immunosuppression), Cryptococcus neoformans and Coccidioides immitis (including intracranial infections), Microsporum spp. and Trichophyton spp.; for endemic mycoses caused by Blastomyces dermatidis, Histoplasma capsulatum (including immunosuppression).
Pharmacokinetics
After oral administration, fluconazole is well absorbed; food intake does not affect the rate of absorption of fluconazole, its bioavailability is 90%.
The time to reach maximum concentration after oral administration of 150 mg of the drug on an empty stomach is 0.5–1.5 hours, Cmax is 90% of the plasma concentration when administered intravenously at a dose of 2.5–3.5 mg/l. T1/2 of fluconazole is 30 hours. Communication with plasma proteins is 11–12%. Plasma concentration is directly dependent on dose. A 90% level of equilibrium concentration is achieved by the 4th–5th day of treatment with the drug (when taken once a day).
Administration of a loading dose (on the first day), 2 times higher than the usual daily dose, allows one to achieve a concentration level corresponding to 90% of the equilibrium concentration by the second day.
Fluconazole penetrates well into all biological fluids of the body. Concentrations of the active substance in breast milk, joint fluid, saliva, sputum and peritoneal fluid are similar to its levels in plasma. Constant values in vaginal secretions are achieved 8 hours after oral administration and are maintained at this level for at least 24 hours.
Fluconazole penetrates well into the cerebrospinal fluid (CSF) – with fungal meningitis, the concentration in the CSF is about 85% of its plasma level. In sweat fluid, epidermis and stratum corneum (selective accumulation) concentrations exceeding serum levels are achieved. After oral administration of 150 mg on the 7th day, the concentration in the stratum corneum of the skin is 23.4 mcg/g, and 1 week after taking the second dose – 7.1 mcg/g; concentration in nails after 4 months of use at a dose of 150 mg once a week is 4.05 mcg/g in healthy and 1.8 mcg/g in affected nails. The volume of distribution approaches the total water content of the body.
It is an inhibitor of the CYP2C9 isoenzyme in the liver. It is excreted primarily by the kidneys (80% unchanged, 11% in the form of metabolites). Fluconazole clearance is proportional to creatinine clearance. No fluconazole metabolites were detected in peripheral blood.
The pharmacokinetics of fluconazole depends significantly on the functional state of the kidneys, and there is an inverse relationship between the half-life and creatinine clearance. After hemodialysis for 3 hours, the concentration of fluconazole in plasma decreases by 50%.
Special instructions
Special instructions
Treatment can be started in the absence of culture or other laboratory test results, but if they are available, appropriate adjustment of fungicidal therapy is recommended.
Since fluconazole is excreted primarily by the kidneys, caution should be exercised in patients with renal impairment. During long-term treatment with fluconazole, dosing should be carried out taking into account QC.
Caution should be exercised when prescribing fluconazole to patients with impaired liver function. During treatment, it is necessary to regularly monitor the activity of liver enzymes and monitor the patient to identify possible toxic effects. If the activity of liver enzymes increases, the doctor must weigh the benefits brought by the therapy against the risk of developing severe liver damage. The hepatotoxic effect of fluconazole is usually reversible: symptoms disappear after discontinuation of therapy.
People with AIDS are more likely to develop severe skin reactions when taking many drugs. In cases where a rash develops in patients with a superficial fungal infection, and it is assessed as definitely related to fluconazole, the drug should be discontinued. If a rash appears in patients with invasive/systemic fungal infections, they should be carefully monitored and fluconazole should be discontinued if bullous changes or erythema multiforme occur.
It is necessary to monitor prothrombin time in patients simultaneously receiving fluconazole and coumarin anticoagulants. Treatment must be continued until clinical and microbiological remission occurs. Premature cessation of treatment leads to relapses.
The dye azorubine, which is part of the drug, can cause an allergic reaction, including bronchial asthma. Allergic reactions are more common in patients with intolerance to acetylsalicylic acid.
Effect on the ability to drive a car or use other mechanical means: experience with the use of fluconazole indicates that impairment of the ability to drive a car or operate machinery associated with the use of the drug is unlikely.
Active ingredient
Active ingredient
Fluconazole
Composition
Composition
1 capsule contains:
Active substance:
fluconazole 150 mg.
Excipients:
corn starch,
povidone (polyvinylpyrrolidone),
colloidal silicon dioxide (aerosil),
sodium lauryl sulfate,
calcium stearate,
lactose.
Hard gelatin capsules:
for a dosage of 50 mg – gelatin, titanium dioxide, azorubine dye, sunset yellow dye and for a dosage of 150 mg – gelatin, titanium dioxide.
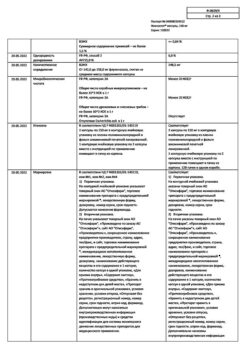
Contraindications
Contraindications
Hypersensitivity to fluconazole, other components of the drug or other azole compounds;
simultaneous use of terfenadine (while constantly taking fluconazole at a dose of 400 mg per day or more), cisapride or astemizole and other drugs that prolong the QT interval and increase the risk of developing severe arrhythmias;
lactose intolerance;
lactase deficiency; glucose-galactose malabsorption; lactation period; children under 3 years of age (for this dosage form).
With caution: liver and/or renal failure, the appearance of a rash due to the use of fluconazole in patients with superficial fungal infection and invasive/systemic fungal infections, simultaneous use of terfenadine and fluconazole at a dose of less than 400 mg per day, potentially proarrhythmogenic conditions in patients with multiple risk factors (organic heart disease, disorders electrolyte balance, simultaneous use of medications that cause arrhythmias); patients with acetylsalicylic acid intolerance, pregnancy.
Side Effects
Side Effects
From the digestive system: decreased appetite, change in taste, nausea, vomiting, diarrhea, flatulence, abdominal pain, rarely – increased activity of liver enzymes and impaired liver function (jaundice, hyperbilirubinemia, increased activity of alanine aminotransferase (ALT), aspartic aminotransferase (AST) and alkaline phosphatase (ALP), hepatitis, hepatocellular necrosis), incl. with a fatal outcome.
From the nervous system: headache, dizziness, rarely – convulsions.
From the hematopoietic organs: rarely – agranulocytosis, neutropenia. Patients with severe fungal infections may experience hematological changes (leukopenia and thrombocytopenia).
From the cardiovascular system: increased duration of the QT interval on the electrocardiogram (ECG), ventricular fibrillation/flutter.
Allergic reactions: skin rash, exudative erythema multiforme (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome), bronchial asthma (more often with intolerance to acetylsalicylic acid), anaphylactoid reactions (including angioedema, facial edema, urticaria, itching).
Others: rarely – impaired renal function, alopecia, hypercholesterolemia, hypertriglyceridemia, hypokalemia.
Interaction
Interaction
A single dose of fluconazole for the treatment of vaginal candidiasis is not accompanied by significant interactions. However, when using several or higher doses of the drug simultaneously with other drugs, the following drug interactions are possible:
The interaction of fluconazole with terfenadine, cisapride and astemizole can lead to an increase in the plasma concentrations of these drugs, which in turn can cause a prolongation of the QT interval and lead to serious cardiac arrhythmias. Fluconazole inhibits enzymes of the P450 system in the liver, thereby reducing the metabolism of terfenadine, cisapride and astemizole. The simultaneous administration of fluconazole and these drugs is contraindicated.
When warfarin and fluconazole are prescribed together, an increase in prothrombin time is observed. In this regard, it is necessary to monitor prothrombin time in patients simultaneously receiving fluconazole and coumarin anticoagulants.
Fluconazole prolongs T1/2 of oral hypoglycemic drugs (sulfonylurea derivatives). In patients with diabetes mellitus, fluconazole and sulfonylurea derivatives can be co-administered, but the possible risk of hypoglycemia must be taken into account.
It must be taken into account that with repeated simultaneous administration of hydrochlorothiazide and fluconazole, the concentration of fluconazole in plasma increases.
Rifampicin accelerates the metabolism of fluconazole. It is necessary to increase the dose of fluconazole accordingly when using them simultaneously.
In patients who have undergone renal transplantation, fluconazole may increase plasma concentrations of cyclosporine. In this regard, it is recommended to monitor cyclosporine concentrations in patients simultaneously receiving cyclosporine and fluconazole.
Fluconazole increases plasma theophylline concentrations. In this regard, it is recommended to monitor theophylline concentrations in patients simultaneously receiving theophylline and fluconazole.
Fluconazole may increase plasma concentrations of indinavir and midazolam. When these drugs are co-administered with fluconazole, their dose should be reduced accordingly.
Clinical studies have shown that, as a result of slower metabolism of zidovudine, its plasma concentration may increase when administered concomitantly with fluconazole. Monitoring of patients receiving both of these drugs simultaneously is necessary, as in this case the incidence of side effects of zidovudine may increase.
Enhances the pharmacological effects of rifabutin (with simultaneous use, cases of uveitis have been described) and phenytoin to a clinically significant extent (with combined use, monitoring the concentration of phenytoin in plasma is necessary). Fluconazole increases serum concentrations of phenytoin. When administered concomitantly, it is necessary to monitor the dose of phenytoin and adjust it accordingly.
Increases tacrolimus concentrations – risk of nephrotoxicity.
Doctors should note that interactions with other drugs have not been specifically studied, but are possible.
Overdose
Overdose
Symptoms: nausea, vomiting, diarrhea; in severe cases, convulsions, hallucinations, and paranoid behavior may occur.
Treatment: symptomatic, gastric lavage; Since fluconazole is excreted by the kidneys, forced diuresis is recommended. Hemodialysis within 3 hours reduces plasma concentrations by 2 times.
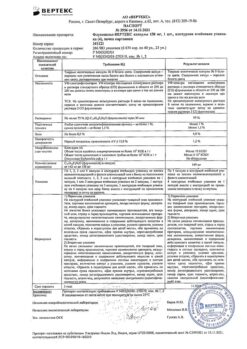
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 25 °C.
Shelf life
Shelf life
2 years
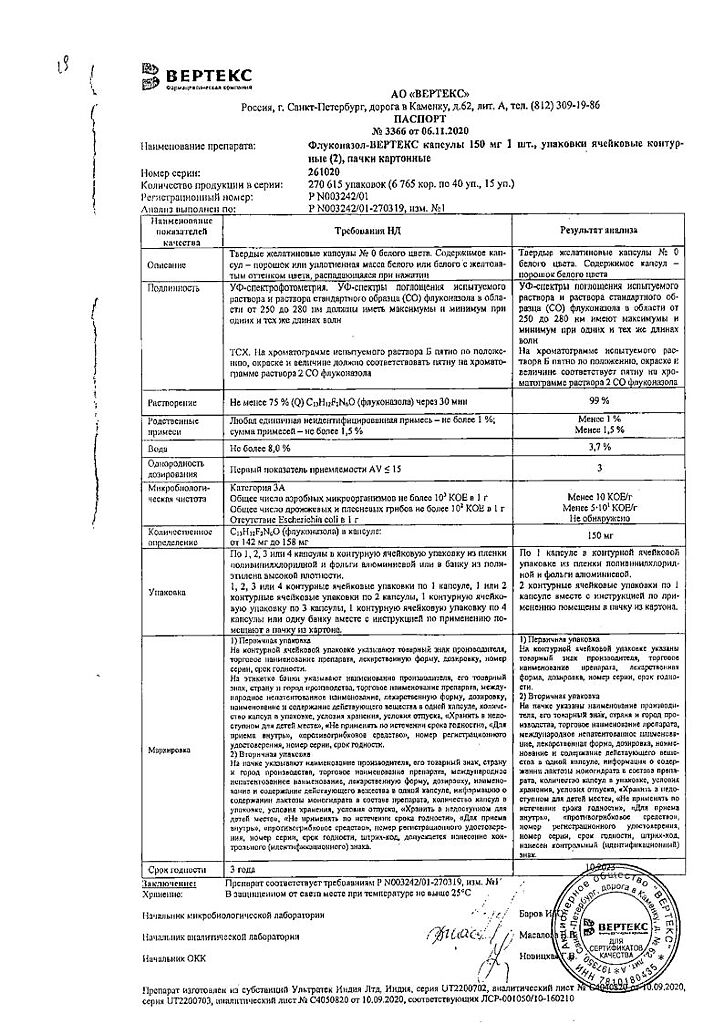
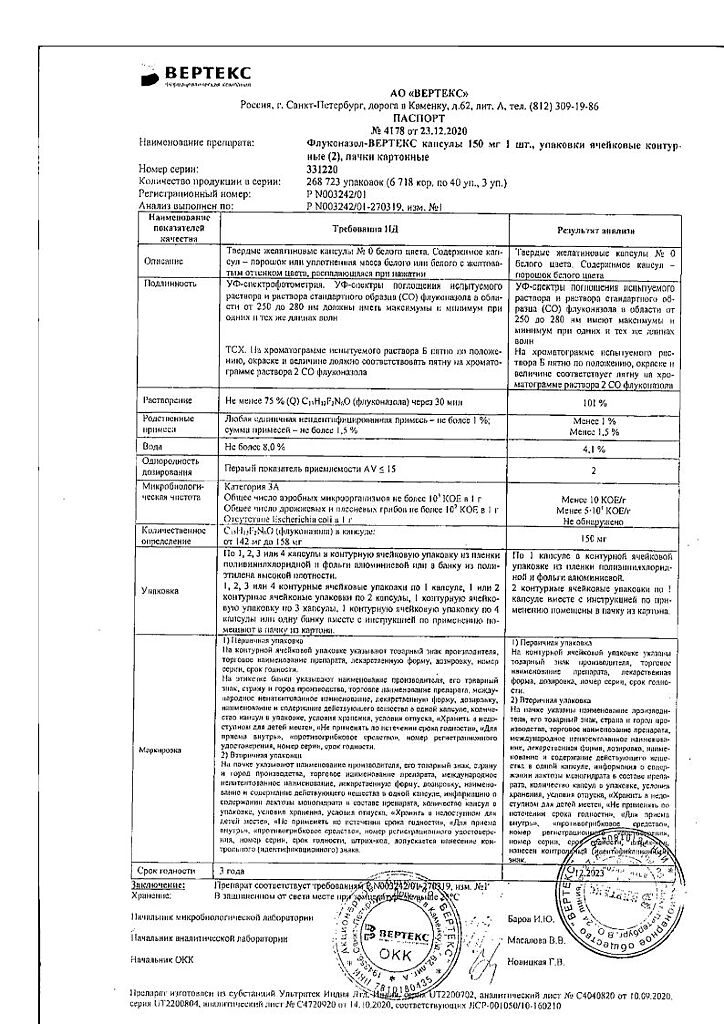
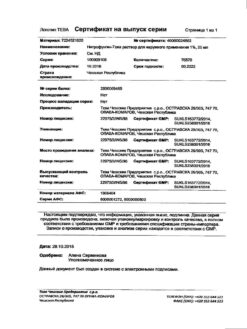
Manufacturer
Manufacturer
Vertex, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a light-protected place at a temperature not exceeding 25 °C. |
| Manufacturer | Vertex, Russia |
| Medication form | capsules |
| Brand | Vertex |
Other forms…
Related products
Buy Fluconazole-Vertex, 150 mg capsules 2 pcs with delivery to USA, UK, Europe and over 120 other countries.