No products in the cart.
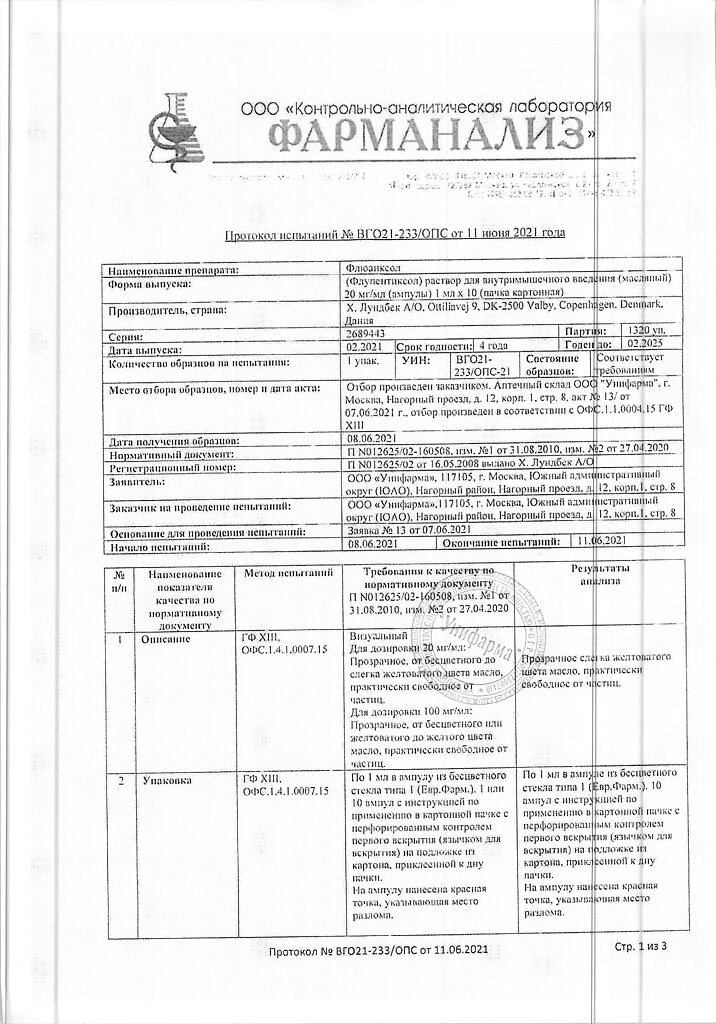
Fluanxol, (oil) 20 mg/ml 1 ml 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
The antipsychotic effect of neuroleptics is associated with blockade of dopamine receptors, but possibly with blockade of 5 HT (5-hydroxytryptamine) receptors as well.
The antipsychotic effects of Fluanxol begin to appear as early as at a daily dose of 3 mg and their intensity increases with increasing dose. Fluanksol has a pronounced anxiolytic effect. The drug has disinhibiting (anti-anxiety and activating) properties, promotes activation of patients, increases their sociability and facilitates their social adaptation.
In small and medium doses (up to 25 mg per day) Fluanxol has no sedative effect, but when prescribing the drug in doses over 25 mg/day a sedative effect can develop.
In low doses (up to 3 mg/day), Fluanxol has an antidepressant effect.
Pharmacokinetics
Intake
After oral administration, Cmax flupentixol in plasma is reached after 3-6 hours. Bioavailability is about 40%.
After intramuscular administration cis(Z)-flupentixol decanoate undergoes enzymatic cleavage into the active component cis(Z)-flupentixol and decanoic acid. Cmax of cis(Z)-flupentixol in serum is reached by the end of the first week after injection.
Distribution
The apparent Vd is about 14.1 L/kg. Binding to plasma proteins is about 99%. Css is achieved after 3 months of drug administration when administered intramuscularly in a solution for injection.
Flupentixol and cis(Z)-flupentixol slightly penetrate the placental barrier and are excreted in small amounts with breast milk.
Metabolism
The metabolites have no neuroleptic activity.
The serum concentration curve decreases exponentially with a T1/2 of approximately 3 weeks upon intramuscular administration of the solution for injection, reflecting the rate of release of flupentixol from the depot.
Flupentixol metabolites have no neuroleptic activity. They are excreted mainly in the feces and partially in the urine. T1/2 is approximately 35 hours.
Pharmacokinetically, a dose of Fluanksol 40 mg when administered intramuscularly once every 2 weeks is equivalent to a dose of Fluanksol 10 mg/day when taken orally for 2 weeks.
Indications
Indications
For oral administration at a dose of up to 3 mg/day
mild to moderate depression with anxiety, asthenia and lack of initiative;
chronic neurotic disorders with anxiety, depression and apathy;
psychosomatic disorders with asthenic reactions.
For oral administration at a dose of 3 mg/day or more
Schizophrenia and schizophrenia-like psychoses with a predominance of hallucinatory symptoms, delusions, thinking disorders, also accompanied by apathy, anergy, decreased mood and autism.
For intramuscular administration
Schizophrenia and other psychotic conditions occurring with hallucinations, delusions and thinking disorders, accompanied by apathy, anergy, decreased mood and autism.
Pharmacological effect
Pharmacological effect
The antipsychotic effect of neuroleptics is associated with blockade of dopamine receptors, but possibly also with blockade of 5 HT (5-hydroxytryptamine) receptors.
The antipsychotic effect of Fluanxol begins to appear already when a daily dose of 3 mg is prescribed and its severity increases with increasing dose. Fluanxol has a pronounced anxiolytic effect. The drug has disinhibiting (anti-autistic and activating) properties, promotes activation of patients, increases their sociability and facilitates social adaptation.
In small and medium doses (up to 25 mg per day), Fluanxol does not have a sedative effect, however, when the drug is prescribed at a dose of more than 25 mg/day. A sedative effect may develop.
When taken in small doses (up to 3 mg/day), Fluanxol has an antidepressant effect.
Pharmacokinetics
Suction
After oral administration, Cmax of flupenthixol in plasma is achieved within 3-6 hours. Bioavailability is about 40%.
After intramuscular administration of cis(Z)-flupenthixol decanoate undergoes enzymatic cleavage into the active component cis(Z)-flupenthixol and decanoic acid. Cmax of cis(Z)-flupenthixol in serum is achieved by the end of the first week after injection.
Distribution
The apparent Vd is about 14.1 l/kg. Plasma protein binding is about 99%. With intramuscular injection of the solution for injection, Css is achieved after 3 months of using the drug.
Flupentixol and cis(Z)-flupenthixol slightly penetrate the placental barrier and are excreted in small quantities in breast milk.
Metabolism
Metabolites do not have neuroleptic activity.
Removal
When the injection solution is administered intramuscularly, the serum concentration curve decreases exponentially with a T1/2 of approximately 3 weeks, reflecting the rate of release of flupenthixol from the depot.
Metabolites of flupenthixol do not have neuroleptic activity. They are excreted mainly in feces and, partially, in urine. T1/2 is approximately 35 hours.
Pharmacokinetically, a dose of Fluanxol 40 mg when administered intramuscularly once every 2 weeks is equivalent to a dose of Fluanxol 10 mg/day when taken orally for 2 weeks.
Special instructions
Special instructions
With concomitant treatment of diabetes mellitus, the administration of Fluanxol may require adjustment of the insulin dose.
If the patient was previously treated with antipsychotics or tranquilizers with a sedative effect, then their use should be stopped gradually.
During long-term therapy, especially with the use of large doses of Fluanxol, it is necessary to conduct careful monitoring and periodic assessment of the patient’s condition.
During pregnancy, Fluanxol should be used only if the expected benefit to the mother outweighs the potential risk to the fetus.
Infants whose mothers took antipsychotic drugs in the last trimester of pregnancy or during labor may experience signs of toxicity, such as lethargy, tremors, and excessive excitability. In addition, these newborns have a low Apgar score.
During treatment with Fluanxol, breastfeeding is allowed if deemed clinically necessary. However, it is recommended to monitor the condition of the newborn, especially in the first 4 weeks after birth.
During the treatment period, it is necessary to refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Flupenthixol
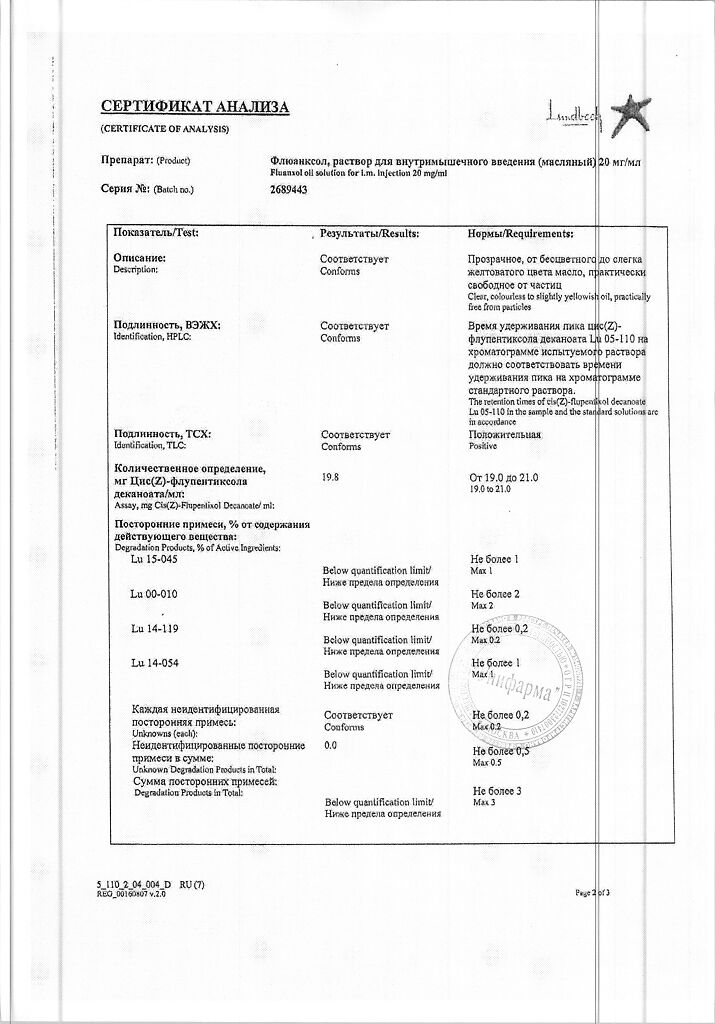
Composition
Composition
1 ml of solution for intramuscular administration contains:
active substance:
cis(Z)-flupenthixol decanoate 20 mg,
excipients:
triglycerides with medium chains.
Pregnancy
Pregnancy
The use of Fluanxol during pregnancy and lactation (breastfeeding) is possible only in cases where the expected benefit of therapy for the mother outweighs the potential risk to the fetus.
Newborns whose mothers took antipsychotics in the third trimester of pregnancy or during childbirth may experience signs of intoxication, such as lethargy, tremor, and excessive excitability. In addition, these newborns have a low Apgar score.
During treatment with Fluanxol, breastfeeding is allowed if deemed clinically necessary.
In such cases, it is recommended to monitor the condition of the newborn, especially in the first 4 weeks after birth.
Contraindications
Contraindications
hypersensitivity to the components of the drug Fluanxol;
vascular collapse;
depression of consciousness of any origin (including those caused by the intake of alcohol, barbiturates or opioid analgesics);
coma;
children and adolescents up to 18 years of age;
hypersensitivity to phenothiazines;
hereditary intolerance to galactose and/or fructose; lapp lactase deficiency; sucrase and isomaltase deficiency; impaired absorption of glucose and galactose (when taking tablets).
Use with caution in patients with organic brain diseases, seizure disorders, incl. with epilepsy (as a result of a decrease in the threshold of convulsive readiness, an increase in seizures is possible);
with severe liver failure;
with hypokalemia, hypomagnesemia; history of cardiovascular diseases (risk of transient decrease in blood pressure), incl. with prolongation of the QT interval, bradycardia less than 50 beats/min, with recent acute myocardial infarction, with uncompensated heart failure, with arrhythmia;
with risk factors for stroke;
with glaucoma (and predisposition to it);
with peptic ulcer of the stomach and duodenum; with alcoholism (possible increased inhibitory effect on the central nervous system); with pheochromocytoma;
with leukopenia; breathing problems associated with acute infectious diseases, bronchial asthma or emphysema; with Parkinson’s disease (increased extrapyramidal effects);
with urinary retention, prostatic hyperplasia with clinical manifestations (risk of urinary retention); with Reye’s syndrome (increased risk of hepatotoxicity); during pregnancy, during lactation (breastfeeding).
It is not recommended to prescribe Fluanxol at a dose of up to 25 mg/day to patients in a state of psychomotor agitation, because the activating effect of Fluanxol in small doses (when taken orally up to 3 mg/day or when administered intramuscularly 10-20 mg once every 2 weeks) can lead to an exacerbation of these symptoms.
Side Effects
Side Effects
The incidence of side effects and their severity are most pronounced at the beginning of treatment and decrease as therapy continues.
From the nervous system: drowsiness, dizziness, headache, tremor, akathisia, parkinsonism, hypokinesia, dystonia; uncommon – attention disorders, extrapyramidal disorders (mainly muscle rigidity and hyperkinesis), dyskinesia, amnesia, convulsive disorders, tardive dystonia.
From the side of mental activity: insomnia, nervousness, agitation; infrequently – decreased libido, depression, confusion.
From the cardiovascular system: infrequently – palpitations, orthostatic hypotension.
From the hematopoietic organs: rarely – granulocytopenia, agranulocytosis (more likely between 4 and 10 weeks of treatment), leukopenia, hemolytic anemia.
From the organs of vision: disturbance of accommodation, clouding of the cornea and/or lens with possible visual impairment; infrequently – oculogyric crisis.
From the digestive system: dry mouth, digestive disorders (including constipation, diarrhea, dyspepsia, nausea), increased salivation, vomiting, cholestatic jaundice (more likely between 2 and 4 weeks of treatment).
Metabolic and eating disorders: uncommon – decreased appetite, increased appetite.
From the respiratory system: infrequently – shortness of breath.
From the endocrine system: dysmenorrhea, gynecomastia, diabetes mellitus, decreased potency, changes in carbohydrate metabolism, hot flashes.
From the urinary system: infrequently – urinary retention, painful urination.
Allergic reactions: uncommon – itching, dermatitis, skin rash, photosensitivity, increased sweating.
Disorders of the musculoskeletal system and connective tissue: infrequently – arthralgia.
From the reproductive system: infrequently – erectile dysfunction, galactorrhea.
From the body as a whole: weakness, asthenia; infrequently – weight gain.
There is evidence of the development of neuroleptic malignant syndrome (NMS). The main symptoms of NMS are hyperthermia, muscle rigidity and impaired consciousness in combination with dysfunction of the autonomic nervous system (labile blood pressure, tachycardia, increased sweating). In addition to immediate cessation of antipsychotic medication, the use of general supportive measures and symptomatic treatment is essential.
Patients on long-term treatment may develop tardive dyskinesia. Antiparkinsonian drugs do not eliminate its symptoms and may worsen them. It is recommended to reduce the dose or, if possible, discontinue treatment.
For persistent akathisia, benzodiazepines or propranolol may be helpful.
There are isolated reports of the development of minor transient changes in liver function test parameters.
When taking flupenthixol, the following side effects that occurred when taking other antipsychotics were also recorded: in rare cases, prolongation of the QT interval, ventricular (ventricular) arrhythmia – ventricular fibrillation, ventricular tachycardia, sudden death and the development of paroxysms of ventricular tachycardia (Torsade de Pointes).
Interaction
Interaction
Fluanxol can enhance the sedative effect of alcohol, the effect of barbiturates and other CNS depressants.
Fluanxol should not be prescribed together with guanethidine or similar active drugs due to the possible weakening of the hypotensive effect of these drugs.
Concomitant use of antipsychotics and lithium increases the risk of neurotoxicity.
Tricyclic antidepressants and antipsychotics mutually inhibit each other’s metabolism.
Fluanxol may reduce the effect of levodopa and the effect of adrenergic drugs, and the combination with metoclopramide and piperazine increases the risk of developing extrapyramidal disorders.
The increase in the QT interval, characteristic of therapy with antipsychotic drugs, can be enhanced by concomitant use of drugs that prolong the QT interval: class IA and III antiarrhythmic drugs (quinidine, amiodarone, sotalol, dofetilide), some antipsychotics (thioridazine), some macrolide antibiotics (erythromycin) and quinolone antibiotics (gatifloxacin, moxifloxacin), some antihistamines (terfenadine, astemizole), as well as cisapride, lithium and other drugs that increase the QT interval. The simultaneous use of Fluanxol and the above drugs should be avoided.
Fluanxol should be administered with caution concomitantly with drugs that cause electrolyte disturbances (thiazide and thiazide-like diuretics) and drugs that can increase plasma concentrations of flupenthixol, due to a possible increased risk of QT prolongation and life-threatening arrhythmias.
Pharmaceutical interactions
Fluanxol in the form of a solution for intramuscular injection should not be mixed with deposited forms based on sesame oil, because this may have a significant impact on the pharmacokinetics of administered drugs.
Overdose
Overdose
Symptoms. Drowsiness, coma, extrapyramidal symptoms, convulsions, shock, hyperthermia/hypothermia.
When taken simultaneously with drugs that affect cardiac activity, ECG changes, prolongation of the QT interval, development of paroxysms of ventricular tachycardia (Torsade de Pointes), cardiac arrest, and ventricular arrhythmia were recorded.
Treatment. Symptomatic and supportive. Gastric lavage should be performed as quickly as possible, and the use of activated carbon is recommended. Measures should be taken to maintain the functioning of the respiratory and cardiovascular systems. Epinephrine (adrenaline) should not be used because this may lead to a subsequent decrease in blood pressure. Seizures can be treated with diazepam, and extrapyramidal symptoms with biperiden.
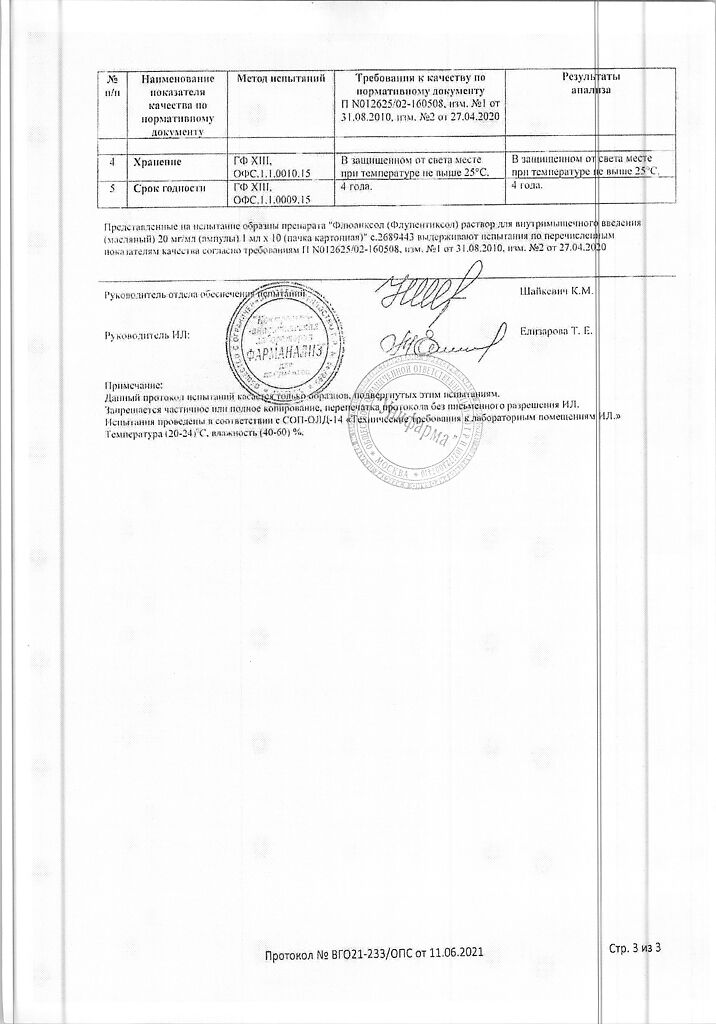
Storage conditions
Storage conditions
At a temperature not higher than 25C.
Shelf life
Shelf life
4 years
Manufacturer
Manufacturer
H. Lundbeck A/O, Denmark
Additional information
| Shelf life | 4 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25C. |
| Manufacturer | Х. Lundbeck A/O, Denmark |
| Medication form | solution |
| Brand | Х. Lundbeck A/O |
Related products
Buy Fluanxol, (oil) 20 mg/ml 1 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.