No products in the cart.
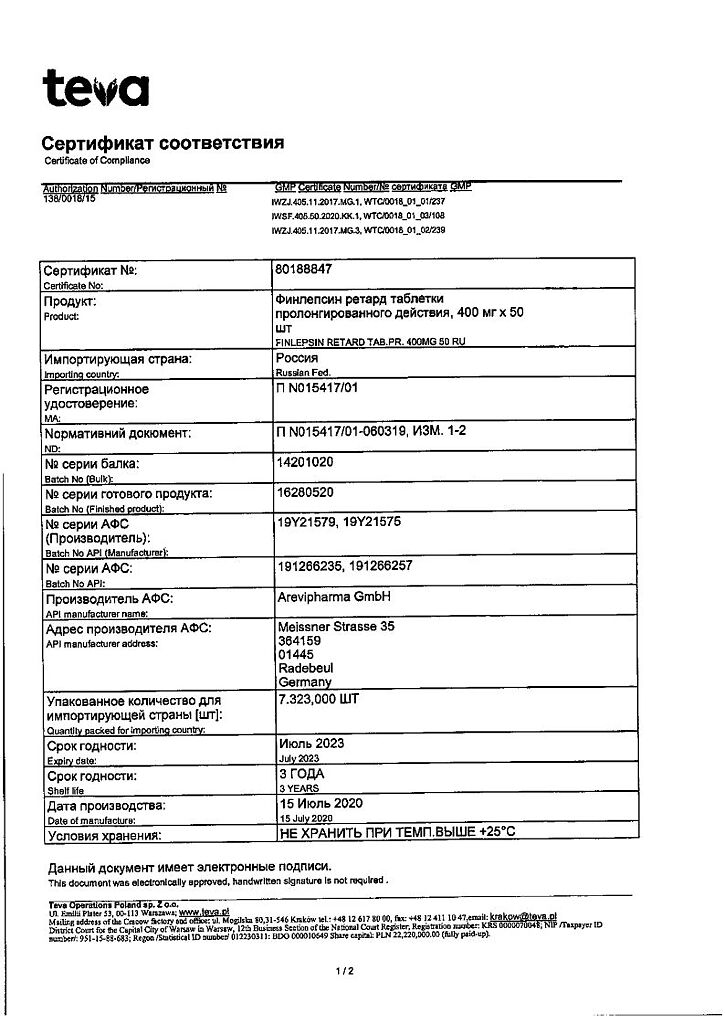
Finlepsin retard, 400 mg 50 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
An antiepileptic drug (dibenzazepine derivative) that also has antidepressant, antipsychotic and antidiuretic effects. Finlepsin has analgesic effect in patients with neuralgia.
The main mechanism of action of the medication is associated with the blockade of potential-dependent sodium channels resulting in stabilization of membranes of overexcited neurons, inhibition of burst discharges of neurons and reduction of synaptic conduction of impulses.
The drug also prevents the re-formation of Na+-dependent action potentials in depolarized neurons. In addition, it markedly reduces the release of glutamate (an amino acid with excitatory neurotransmitter properties), increases the reduced threshold of seizure readiness and thus reduces the risk of an epileptic seizure.
It increases transport of potassium ions and modulates potential-dependent calcium channels, which may also contribute to the anticonvulsant effect of the drug. The same effect of the drug is seen in focal (partial) epileptic seizures (simple and complex), accompanied or not accompanied by secondary generalization, in generalized tonic-clonic epileptic seizures, as well as in combinations of these types of seizures (usually ineffective in small seizures – petit mal, absences and myoclonic seizures).
In patients with epilepsy (especially in children and adolescents) a positive effect on the symptoms of anxiety and depression, as well as decreased irritability and aggressiveness has been noted. The effect on cognitive function and psychomotor performance depends on the dose.
The onset of anticonvulsant effects varies from several hours to several days (sometimes up to 1 month due to autoinduction of metabolism).
In essential and secondary trigeminal neuralgia, it prevents the onset of painful attacks in most cases. Relief of pain in trigeminal neuralgia is noted in 8-72 hours.
In alcohol withdrawal syndrome it increases the threshold of seizure readiness (which is usually lowered in this condition) and reduces the severity of clinical manifestations of the syndrome (increased agitation, tremor, gait disturbances).
The antipsychotic (antimanic) effect develops after 7-10 days, which may be due to inhibition of dopamine and noradrenaline metabolism.
The prolonged dosage form maintains more stable carbamazepine blood concentrations when taken 1-2 times daily.
Pharmacokinetics
Intake
When the drug is taken orally carbamazepine is slowly but almost completely absorbed from the gastrointestinal tract (eating has no significant effect on the speed and extent of absorption).
After a single tablet administration the Cmax is reached after 32 hours. The mean Cmax value of the unchanged active ingredient after a single dose of 400 mg carbamazepine is about 2.5 µg/mL.
Distribution
The Css in plasma is reached after 1-2 weeks of continuous administration (the rate of reaching depends on individual characteristics of metabolism: autoinduction of liver enzyme systems, heteroinduction by other concurrently used drugs, as well as on the patient’s condition, the drug dose and duration of treatment).
There are significant interindividual differences in Css values in the therapeutic range: in most patients these values range from 4 to 12 µg/mL (17-50 µmol/L). The concentration of carbamazepine-10,11-epoxide (pharmacologically active metabolite) is about 30% of the carbamazepine concentration.
The binding to plasma proteins in children is 55-59%, in adults – 70-80%. Apparent Vd is 0.8-1.9 l/kg. In cerebrospinal fluid and saliva there are concentrations proportional to the amount of active substance unbound to proteins (20-30%).
It penetrates through the placental barrier and is excreted with breast milk (concentration is 25-60% of that in blood plasma).
Metabolism
Metabolized in the liver, mainly by the epoxide route, with the formation of the main metabolites: active – carbamazepine-10,11-epoxide and inactive conjugate with glucuronic acid. The main isoenzyme providing biotransformation of carbamazepine to carbamazepine-10,11-epoxide is CYP3A4.
These metabolic reactions also produce the metabolite 9-hydroxy-methyl-10-carbamoylacridan, which has weak pharmacological activity. Carbamazepine can induce its own metabolism.
Elevation
The T1/2 after an oral single dose is 60-100 h (average about 70 h), with prolonged administration the T1/2 is reduced due to autoinduction of liver enzyme systems. After a single oral administration, 72% of the administered dose is excreted in the urine and 28% in the feces; about 2% is excreted in the urine as unchanged carbamazepine, about 1% as a 10,11-epoxide metabolite.
Pharmacokinetics in Special Clinical Cases
There is no evidence that the pharmacokinetics of carbamazepine changes in elderly patients.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
One retard tablet (sustained release) contains 400 mg of the active ingredient carbamazepine.
Other constituents:
methacrylate copolymers,
triacetin,
talc,
Microcrystalline cellulose,
High dispersible silicon dioxide,
Magnesium stearate,
Crospovidone.
How to take, the dosage
How to take, the dosage
The drug is taken orally during or after meals with plenty of fluid.
For ease of use, the tablet (as well as half or a quarter of it) can be dissolved in water or juice beforehand, because the property of prolonged release of the active substance is retained after dissolving the tablet in liquid. The range of administered doses is 400-1200 mg/day. Daily dose is divided into 1-2 doses.
The maximum daily dose is 1600 mg.
Epilepsy
Whenever possible, Finlepsin® retard should be prescribed as monotherapy. Treatment begins with a small daily dose and is slowly increased until optimal effect is achieved.
The addition of Finlepsin® Retard to pre-existing antiepileptic therapy should be done gradually, with no change in the doses of the drugs used or adjustment if necessary.
If another dose of the medication is missed, the missed dose should be taken as soon as noticed, and no double dose of the medication should be taken.
Adults
The initial dose is 200-400 mg/day, then the dose is slowly increased until optimal therapeutic effect is achieved. The maintenance dose is 800-1200 mg/day in 1-2 doses.
Children
The starting dose for children aged 6 to 15 years is 200 mg/day, then the dose is gradually increased by 100 mg/day until optimal effect is achieved.
The maintenance doses for children aged 6-10 years are 400-600 mg/day (in 2 doses), for children aged 11-15 years are 600-1000 mg/day (in 2 doses).
The recommended dosing regimen is shown in the table.
The duration of use depends on the indication and the patient’s individual response to the drug.
The decision to change the patient to Finlepsin® Retard, the duration of treatment or discontinuation of treatment is made by the physician individually. The drug dose may be reduced or completely discontinued not earlier than after 2-3 years of complete absence of seizures.
The treatment is discontinued, gradually reducing the dose over 1-2 years, under EEG control. In children, when reducing the daily dose, the increase in body weight with age should be taken into account.
Truncal neuralgia, idiopathic pharyngeal neuralgia
The initial dose is 200-400 mg/day in 2 doses. The initial dose is increased until the pain completely disappears, on average up to 400-800 mg/day. Thereafter, therapy may be continued with a lower maintenance dose of 400 mg/day in a certain proportion of patients.
In elderly patients and patients with individual sensitivity to the effects of carbamazepine, Finlepsin® Retard is indicated in a starting dose of 200 mg once daily.
Pain in diabetic neuropathy
The drug is prescribed in 200 mg in the morning and 400 mg in the evening. In exceptional cases, Finlepsin® retard may be prescribed in a dose of 600 mg twice daily.
Treatment of alcohol withdrawal in hospital settings
The average daily dose is 600 mg (200 mg in the morning and 400 mg in the evening). In severe cases in the first days the dose can be increased up to 1200 mg/day in 2 doses.
If necessary, Finlepsin® retard may be combined with other drugs used for treatment of alcohol withdrawal, except sedatives and hypnotics.
The plasma levels of carbamazepine must be monitored regularly during treatment.
Because of the development of adverse reactions from the CNS and autonomic nervous system, patients are monitored closely in a hospital setting.
Epileptiform seizures in multiple sclerosis
The average daily dose is 200-400 mg 2 times per day.
The treatment and prevention of psychosis
The starting dose and maintenance dose are generally the same: 200-400 mg/day. If necessary, the dose can be increased to 400 mg 2 times a day.
Interaction
Interaction
Co-administration with CYP3A4 isoenzyme inhibitors may increase plasma concentrations of carbamazepine and lead to adverse reactions.
The concomitant use with inducers of CYP3A4 isoenzyme may lead to acceleration of metabolism and decrease of plasma concentration of carbamazepine and decrease of therapeutic effect. On the contrary, their withdrawal may decrease the biotransformation rate of carbamazepine and lead to an increase in its concentration.
When used together, plasma concentrations of carbamazepine are increased by verapamil, diltiazem, felodipine, dextropropoxyphene, viloxazine, fluoxetine, fluvoxamine, cimetidine, acetazolamide, danazol, desipramine, nicotinamide (in adults, in high doses only); macrolides (erythromycin, jozamycin, clarithromycin, troleandomycin); azoles (itraconazole, ketoconazole, fluconazole), terfenadine, loratadine, isoniazid, propoxyphene, grapefruit juice, protease inhibitors used in HIV therapy (such as ritonavir) (when using such combinations, dosing adjustments or monitoring of carbamazepine plasma concentrations are required).
Felbamate decreases plasma concentrations of carbamazepine and increases concentrations of carbamazepine-10,11-epoxide, and there may be a simultaneous decrease in serum concentrations of felbamate.
In co-administration phenobarbital, phenytoin, primidone, methsuximide, fensuximide, theophylline, rifampicin, cisplatin, doxorubicin reduce carbamazepine concentrations. Clonazepam, valpromide, valproic acid, oxcarbazepine, and herbal preparations containing Hypericum perforatum may have similar effects.
When used together, valproic acid and primidone may displace carbamazepine from plasma protein binding and increase concentrations of the pharmacologically active metabolite (carbamazepine-10,11-epoxide). When co-administration of Finlepsin® retard with valproic acid in exceptional cases coma and confusion may occur.
In co-administration, isotretinoin alters the bioavailability and/or clearance of carbamazepine and carbamazepine-10,11-epoxide (monitoring of plasma carbamazepine concentrations is necessary).
When used concomitantly, carbamazepine may decrease plasma concentrations and, therefore, reduce or even completely negate the effects and require dose adjustments of the following drugs: clobazam, clonazepam, digoxin, ethosuximide, primidone, valproic acid, alprazolam, GCS (prednisolone, dexamethasone), cyclosporine, tetracyclines (doxycycline), haloperidol, methadone, oral drugs estrogen and/or progesterone (alternative methods of contraception should be selected), theophylline, oral anticoagulants (warfarin, phenprocoumon, dicumarol), lamotrigine, topiramate, tricyclic antidepressants (imipramine, amitriptyline, nortriptyline, clomipramine), clozapine, felbamate, tiagabine, oxcarbazepine, protease inhibitors used in HIV therapy (indinavir, ritonavir, saquinavir), calcium channel blockers (dihydropyridine group, such as felodipine), itraconazole, levothyroxine, midazolam, olanzapine, praziquantel, risperidone, tramadol, ziprasidone.
There is a possibility of increased or decreased plasma phenytoin with carbamazepine and increased levels of mephenytoin (in rare cases).
Concomitant use of carbamazepine and lithium preparations may increase the neurotoxic effects of both active substances.
The tetracyclines may impair the therapeutic effect of carbamazepine.
Carbamazepine combined with paracetamol increases the risk of its toxic effects on the liver and reduces the therapeutic effectiveness (metabolism acceleration of paracetamol).
The simultaneous administration of carbamazepine with phenothiazine, pimozide, thioxanthenes (chlorprotixene), molindone, haloperidol, maprotiline, clozapine and tricyclic antidepressants leads to increased CNS depression and weakened anticonvulsant effect of carbamazepine.
MAO inhibitors increase the risk of hyperthermic crises, hypertensive crises, seizures, and death (before prescribing carbamazepine, MAO inhibitors should be withdrawn at least 2 weeks or, if the clinical situation allows, even longer).
The simultaneous administration with diuretics (hydrochlorothiazide, furosemide) may lead to hyponatremia accompanied by clinical manifestations.
Carbamazepine when used together weakens the effects of nondepolarizing myorelaxants (pancuronium). If this combination is used, it may be necessary to increase the dose of myorelaxants, and patients should be closely monitored, since they may stop their effects more quickly.
Limits tolerance to ethanol.
Myelotoxic drugs increase the manifestation of hematotoxicity of carbamazepine.
Accelerates the metabolism of indirect anticoagulants, hormonal contraceptive drugs, folic acid; praziquantel.
May increase the elimination of thyroid hormones.
Accelerates the metabolism of anesthetics (enflurane, halothane, fluorothane) with an increased risk of hepatotoxic effects.
Accelerates the formation of nephrotoxic metabolites of methoxyflurane.
Accelerates the hepatotoxic effects of isoniazid.
Special Instructions
Special Instructions
The drug should be used only with regular medical supervision.
Monotherapy for epilepsy starts with prescribing the drug in low doses, gradually increasing them until the desired therapeutic effect is achieved.
In some cases, treatment with antiepileptic drugs has been accompanied by suicide attempts/suicidal intentions. This was also confirmed in a meta-analysis of randomized clinical trials with antiepileptic drugs. Since the mechanism of suicide attempts with antiepileptic drugs is not known, their occurrence cannot be excluded with treatment with Finlepsin® retard. Patients and caregivers should be warned to watch for suicidal thoughts/suicidal behavior and seek medical attention immediately if symptoms occur.
It is advisable to determine plasma concentrations of carbamazepine in order to select the optimal dose, especially with combination therapy. In individual cases the dose required for therapy may deviate significantly from the recommended initial and maintenance doses, e.g. due to accelerated metabolism due to induction of microsomal liver enzymes or due to drug-drug interactions in combination therapy.
Finlepsin® retard should not be combined with sedative-hypnotics. If necessary, it may be combined with other substances used to treat alcohol withdrawal.
When transferring a patient to carbamazepine, the dose of the previously prescribed antiepileptic drug should be gradually reduced until it is completely withdrawn. Sudden discontinuation of carbamazepine may provoke epileptic seizures. If abrupt interruption of treatment is necessary, the patient should be transferred to another antiepileptic drug under cover of a drug indicated in such cases (e.g. diazepam v/v or rectally, or phenytoin v/v).
There have been several reported cases of vomiting, diarrhea and/or reduced feeding, seizures and/or respiratory depression in neonates whose mothers took carbamazepine concomitantly with other anticonvulsants (these reactions may represent manifestations of neonatal withdrawal syndrome).
Please note that carbamazepine may adversely affect the reliability of oral contraceptives, so women of childbearing age should use alternative methods of contraception during treatment (intermenstrual bleeding in women with concomitant use of oral contraceptives is likely).
Before prescribing carbamazepine and during treatment it is necessary to monitor liver function parameters, especially in patients with a history of liver disease and in elderly patients. In case of aggravation of already existing liver dysfunction or in case of appearance of active liver disease, the drug should be stopped immediately. Before start of treatment it is necessary to carry out investigation of blood picture (including platelets count, reticulocytes count), serum iron level, general urine analysis, blood urea level, EEG, determination of electrolytes concentration in serum; blood (and periodically during the treatment, because hyponatremia may occur). Thereafter, these parameters should be monitored weekly during the first month of treatment and then monthly.
In most cases, transient or persistent decreases in platelet and/or leukocyte counts are not precursors to the onset of aplastic anemia or agranulocytosis. However, clinical blood counts, including platelet counts and possibly reticulocyte counts, as well as serum iron levels should be performed before initiating treatment and periodically during treatment. Non-progressive asymptomatic leukopenia does not require withdrawal, but treatment should be discontinued if progressive leukopenia or leukopenia accompanied by clinical symptoms of infectious disease occurs.
Carbamazepine should be immediately discontinued if hypersensitivity reactions or symptoms suspected of developing Stevens-Johnson syndrome or Lyell syndrome occur. Mild skin reactions (isolated maculopapular or maculopapular rash) usually go away within a few days or weeks, even if treatment is continued or after reduction of the drug dose (the patient should be under medical supervision during this time).
When using the drug, the possibility of activation of latent psychosis should be considered, and in elderly patients, the possibility of disorientation or psychomotor agitation.
Male fertility and/or spermatogenesis disorders may occur (the relationship of these disorders to carbamazepine administration has not yet been established).
The patient should be informed about possible early signs of hematopoietic, hepatic and dermatologic toxic reactions and the need to seek medical attention immediately if there are adverse reactions such as fever, sore throat, rash, oral mucosal ulceration, bruising without cause, petechiae or purpura hemorrhage.
We recommend an ophthalmologic examination, including slit-lamp examination of the eye fundus and measurement of intraocular pressure if necessary, before initiating treatment. Patients with elevated intraocular pressure require constant monitoring when the drug is prescribed.
Patients with severe cardiovascular disease, liver or kidney disease, or older patients should use lower doses.
While there is little correlation between carbamazepine dose, concentrations, and clinical efficacy or tolerability, regular determination of plasma concentrations of carbamazepine is also useful when there is a rapid increase in seizure frequency; to check the regularity of patient administration; in pregnancy; when treating children or adolescents; when absorption is suspected; when toxic reactions are suspected when the patient is taking multiple medications.
The use of the drug is recommended to withhold alcohol.
Contraindications
Contraindications
. The preparation should be used with caution in decompensated chronic heart failure, liver and/or kidney function disorders, elderly patients, patients with chronic alcoholism (CNS depression increases, carbamazepine metabolism increases), in hyponatremia of dilution (ADH hypersecretion syndrome, hypopituitarism, hypothyroidism, insufficiency of the adrenal cortex), inhibition of bone marrow hematopoiesis during drug administration (history), in prostatic hyperplasia, increased intraocular pressure; concomitant use with sedative and hypnotic drugs.
The use in patients with hepatic impairment
The drug should be used with caution in patients with hepatic impairment.
The use of the drug in impaired renal function
The drug should be used with caution in impaired renal function.
Performance in elderly patients
In elderly patients, Finlepsin® Retard is indicated in starting dose of 200 mg once daily, use with caution.
Side effects
Side effects
The following criteria were used to evaluate the incidence of various adverse reactions: very common (â¥10%), common (â¥1%, but
CNS and peripheral nervous system disorders: frequent – dizziness, ataxia, somnolence, general weakness, headache, accommodation paresis; sometimes – abnormal involuntary movements (e.g., tremor, “fluttering” tremor, dystonia, tics), nystagmus; rarely – hallucinations (visual or auditory), depression, decreased appetite, anxiety, aggressive behavior, psychomotor agitation, disorientation, psychosis activation, orofacial dyskinesia, oculomotor disorders, speech disorders (such as dysarthria or slurred speech), choreoathetoid disorders, peripheral neuritis, paresthesias, muscle weakness and paresis. The role of carbamazepine in the development of MNS, especially in combination with neuroleptics, remains unclear.
The development of CNS side effects may result from a relative overdose of the drug or significant fluctuations in plasma concentrations of carbamazepine.
Allergic reactions: often – urticaria; sometimes – erythroderma, multiorgan hypersensitivity reactions of delayed type with fever, skin rash, vasculitis (including erythema nodosum as a manifestation of cutaneous vasculitis), lymphadenopathy, lymphoma-like signs, arthralgia, leukopenia, eosinophilia, hepatosplenomegaly and altered liver function parameters (the above manifestations occur in various combinations).
Overdose
Overdose
Symptoms and complaints arising in overdose usually reflect CNS, cardiovascular and respiratory system disorders.
CNS and sense organs: CNS depression, disorientation, somnolence, agitation, hallucinations, coma, blurred vision, slurred speech, dysarthria, nystagmus, ataxia, dyskinesia, hyperreflexia turning into hyporeflexia, seizures, psychomotor disorders, myoclonus, hypothermia, mydriasis.
Cardiovascular system disorders: tachycardia, decreased BP, sometimes increased BP, intraventricular conduction disorders with enlarged QRS complex, syncope, cardiac arrest.
Respiratory system: respiratory depression, pulmonary edema.
In the digestive system: nausea, vomiting, delayed evacuation of food from the stomach, decreased motility of the large intestine.
Uses of the urinary system: urinary retention, oliguria or anuria; fluid retention.
Laboratory findings: leukocytosis or leukopenia, hyponatremia, possible metabolic acidosis, possible hyperglycemia and glucosuria, increased CPK muscle fraction.
Treatment: there is no specific antidote. Symptomatic supportive treatment in ICU, monitoring of cardiac function, body temperature, corneal reflexes, renal and bladder function, correction of electrolyte disorders are necessary. It is necessary to determine the concentration of carbamazepine in plasma to confirm poisoning with this agent and assess the degree of overdose, gastric lavage, prescription of activated charcoal. Late evacuation of gastric contents may lead to delayed absorption for 2 and 3 days and reappearance of intoxication symptoms during recovery). Forced diuresis, hemodialysis and peritoneal dialysis are ineffective; however, dialysis is indicated when severe poisoning and renal failure are combined. Hemotransfusion may be necessary in children.
Pregnancy use
Pregnancy use
The drug should be used only with regular medical supervision.
Monotherapy for epilepsy starts with prescribing the drug in low doses, gradually increasing them until the desired therapeutic effect is achieved.
In some cases, treatment with antiepileptic drugs has been accompanied by suicide attempts/suicidal intentions. This was also confirmed in a meta-analysis of randomized clinical trials with antiepileptic drugs.
As the mechanism of suicide attempts with antiepileptic drugs is not known, their occurrence cannot be ruled out with treatment with Finlepsin® retard. Patients and caregivers should be warned to watch for suicidal thoughts/suicidal behavior and seek medical attention immediately if symptoms occur.
It is advisable to determine plasma concentrations of carbamazepine in order to select the optimal dose, especially with combination therapy.
In individual cases the dose required for therapy may deviate significantly from the recommended initial and maintenance doses, e.g. due to accelerated metabolism due to induction of hepatic microsomal enzymes or due to drug interactions in combination therapy.
Finlepsin® retard should not be combined with sedative-hypnotics. If necessary, it may be combined with other substances used to treat alcohol withdrawal.
When transferring a patient to carbamazepine, the dose of the previously prescribed antiepileptic drug should be gradually reduced until it is completely withdrawn. Sudden discontinuation of carbamazepine may provoke epileptic seizures.
If abrupt interruption of treatment is necessary, the patient should be switched to another antiepileptic drug under cover of a medication indicated in such cases (e.g., diazepam IV or rectally, or phenytoin IV).
There have been several reported cases of vomiting, diarrhea and/or reduced feeding, seizures and/or respiratory depression in neonates whose mothers took carbamazepine concomitantly with other anticonvulsants (these reactions may represent manifestations of neonatal withdrawal syndrome).
Please note that carbamazepine may adversely affect the reliability of oral contraceptives, so women of childbearing age should use alternative methods of contraception during treatment (intermenstrual bleeding in women with concomitant use of oral contraceptives is likely).
Before prescribing carbamazepine and during treatment it is necessary to monitor liver function parameters, especially in patients with a history of liver disease and in elderly patients. If pre-existing liver dysfunction worsens or if active liver disease occurs, the drug should be discontinued immediately.
Before initiating treatment, a blood count (including platelet count, reticulocyte count), serum iron levels, urinalysis, blood urea levels, EEG, determination of serum electrolyte concentration (and periodically during treatment, as hyponatremia may occur) should be performed.
Thereafter, these parameters should be monitored weekly for the first month of treatment and then monthly.
Similarities
Similarities
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
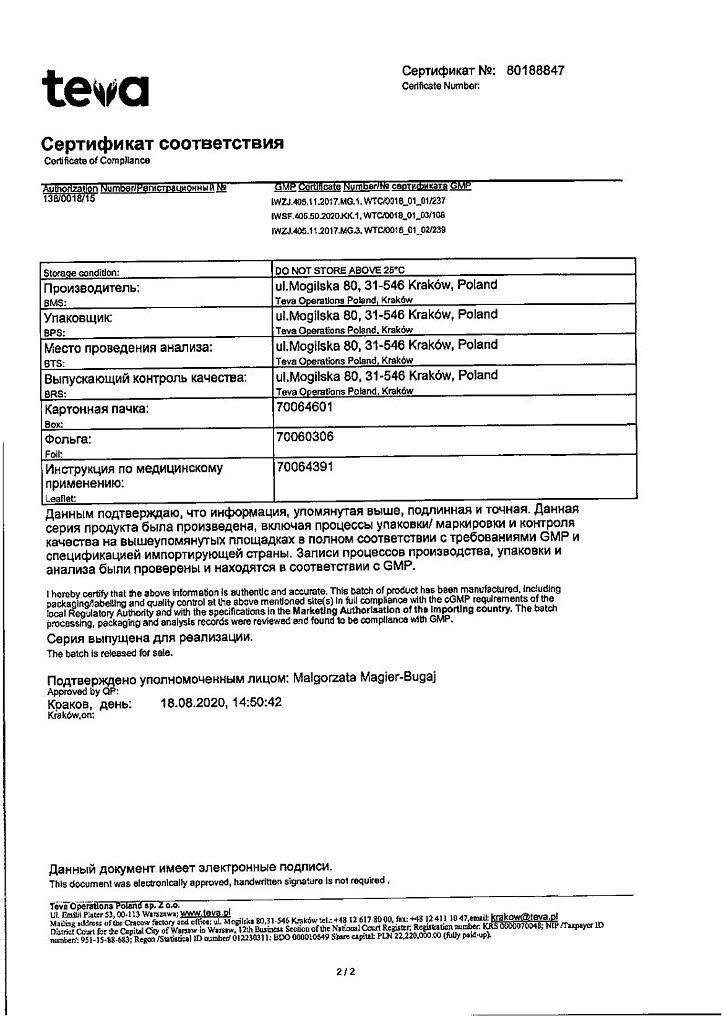
| Manufacturer | Teva Operations Poland Sp. z o.o., Poland |
| Medication form | slow-release tablets |
| Brand | Teva Operations Poland Sp. z o.o. |
Related products
Buy Finlepsin retard, 400 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.