No products in the cart.
Fevarin, 50 mg 15 pcs.
€29.70 €24.75
Out of stock
(E-mail when Stock is available)
Description
Pharmacodynamics
The mechanism of action of Fevarin is associated with selective inhibition of serotonin reuptake by brain neurons and is characterized by minimal effect on the noradrenergic system. Phevarin has a weak ability to bind to a-adrenergic, b-adrenergic, histaminergic, m-cholinoreceptors, dopaminergic or serotoninergic receptors.
Pharmacokinetics
Intake:
After oral administration, fluvoxamine is completely absorbed from the gastrointestinal tract. Maximum plasma concentrations of the drug are noted 3-8 hours after ingestion. Absolute bioavailability is 53% after primary metabolism in the liver. Concomitant administration of fluvoxamine with food has no effect on pharmacokinetics.
Distribution:
The binding of fluvoxamine to plasma proteins is 80% (in vitro). The volume of distribution is 25 l/kg.
Metabolism:
Metabolism of fluvoxamine occurs primarily in the liver. Although cytochrome P 450 isoenzyme 2D6 is major in the metabolism of fluvoxamine, plasma concentrations of the drug are not much higher in persons with decreased function of this isoenzyme than in those with normal metabolism. The average plasma elimination half-life, which is 13-15 hours for a single dose, is slightly longer with multiple doses (17-22 hours), and the equilibrium plasma concentration is usually reached within 10-14 days. Fluvoxamine undergoes biotransformation in the liver (mainly by oxidative demethylation) to at least nine metabolites, which are excreted through the kidneys.
The two major metabolites have negligible pharmacological activity. The other metabolites are probably pharmacologically inactive. Fluvoxamine significantly inhibits cytochrome P450 1A2, moderately inhibits cytochromes P450 2C and P450 WA4, and slightly inhibits cytochrome P450 2D6. Pharmacokinetics of a single dose of fluvoxamine is linear. The equilibrium concentration of fluvoxamine is higher than that of single dose and is disproportionately higher at higher daily doses.
Special patient groups:
The pharmacokinetics of fluvoxamine are similar in healthy subjects, the elderly, and patients with renal impairment. The metabolism of fluvoxamine is reduced in patients with liver disease. Equilibrium plasma concentrations of fluvoxamine are twice as high in children (ages 6-11 years) than in adolescents (ages 12-17 years). Plasma concentrations of the drug in adolescents are similar to those in adults.
Indications
Indications
Depression of various origins; obsessive-compulsive disorders.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
The mechanism of action of Fevarin is associated with selective inhibition of serotonin reuptake by brain neurons and is characterized by minimal effects on the noradrenergic system. Fevarin has a weak ability to bind to a-adrenergic, b-adrenergic, histaminergic, m-cholinergic, dopaminergic or serotonergic receptors.
Pharmacokinetics
Suction:
After oral administration, fluvoxamine is completely absorbed from the gastrointestinal tract. Maximum concentrations of the drug in blood plasma are observed 3-8 hours after administration. Absolute bioavailability is 53% after primary metabolism in the liver. Concomitant use of fluvoxamine with food does not affect pharmacokinetics.
Distribution:
The binding of fluvoxamine to plasma proteins is 80% (in vitro). Volume of distribution – 25 l/kg.
Metabolism:
Metabolism of fluvoxamine occurs primarily in the liver. Although the 2D6 isoenzyme of cytochrome P 450 is the main one in the metabolism of fluvoxamine, the concentration of the drug in the blood plasma in individuals with reduced function of this isoenzyme is not much higher than in individuals with normal metabolism. The average elimination half-life from the blood plasma, which is 13-15 hours for a single dose, increases slightly with repeated doses (17-22 hours), and the equilibrium concentration in the blood plasma is usually achieved within 10-14 days. Fluvoxamine undergoes biotransformation in the liver (mainly by oxidative demethylation) to at least nine metabolites, which are excreted through the kidneys.
The two main metabolites have little pharmacological activity. Other metabolites are probably pharmacologically inactive. Fluvoxamine significantly inhibits cytochrome P450 1A2, moderately inhibits cytochromes P450 2C and P450 ZA4, and slightly inhibits cytochrome P450 2D6. The pharmacokinetics of a single dose of fluvoxamine is linear. The steady-state concentration of fluvoxamine is higher than that of a single dose and is disproportionately higher at higher daily doses.
Special patient groups:
The pharmacokinetics of fluvoxamine are similar in healthy people, the elderly and patients with renal failure. The metabolism of fluvoxamine is reduced in patients with liver disease. The steady-state plasma concentration of fluvoxamine is twice as high in children (aged 6–11 years) than in adolescents (aged 12–17 years). Plasma concentrations of the drug in adolescents are similar to those in adults.
Special instructions
Special instructions
During treatment with the drug, drinking alcohol is not recommended.
Patients suffering from depression generally have a high risk of attempting suicide, which may persist until sufficient remission is achieved. Such patients should be monitored.
Treatment of patients suffering from liver or kidney failure should begin with the minimum effective doses of Fevarin under strict medical supervision. In rare cases, treatment with Fevarin may lead to an increase in the level of liver transaminases, most often accompanied by corresponding clinical symptoms. In these cases, Fevarin should be discontinued.
Blood glucose control may be impaired, especially in the early stages of treatment. Dosage adjustments of antidiabetic medications may be necessary.
Caution should be exercised when prescribing the drug to patients with a history of seizures. Prescribing Fevarin to patients with unstable epilepsy should be avoided, and patients with stable epilepsy should be under strict medical supervision. Treatment with Fevarin should be discontinued if epileptic seizures develop or their frequency increases.
Rare cases of the development of serotonergic syndrome or a condition similar to neuroleptic malignant syndrome have been described, which may be associated with taking fluvoxamine in combination with other serotonergic antidepressants and antipsychotics. Because these syndromes can lead to potentially life-threatening conditions manifested by hyperthermia, muscle rigidity, myoclonus, autonomic lability with possible rapid changes in vital signs, changes in mental status including irritability, agitation, confusion, delirium and coma, treatment with fluvoxamine should be discontinued. If necessary, appropriate treatment should be started.
As with the use of other selective serotonin reuptake inhibitors, in rare cases, while taking fluvoxamine, hyponatremia may occur, which reverses after discontinuation of the drug. Some cases have been caused by antidiuretic hormone deficiency syndrome. These cases were mainly observed in elderly patients.
There are reports of intradermal hemorrhages such as ecchymosis and purpura, as well as hemorrhagic manifestations (eg gastrointestinal bleeding) observed with the use of selective serotonin reuptake inhibitors. Caution should be exercised when prescribing these drugs in elderly patients and patients concomitantly receiving drugs that affect platelet function (atypical antipsychotics and phenothiazines, many tricyclic antidepressants, aspirin, NSAIDs) or drugs that increase the risk of bleeding, as well as in patients with a history of bleeding and prone to bleeding (for example, patients with thrombocytopenia).
When combined with fluvoxamine, plasma concentrations of terfenadine, astemizole or cisapride may increase, increasing the risk of QT prolongation. Therefore, fluvoxamine should not be given with these drugs.
Data obtained from the treatment of elderly patients and younger patients indicate the absence of clinically significant differences between the daily doses usually used in them. However, increasing doses of the drug in elderly patients should always be done more slowly and with greater caution. Fevarin may lead to a slight decrease in heart rate (by 2–6 beats per minute).
Due to the lack of clinical experience, Fevarin is not recommended for the treatment of depression in children.
Fevarin, administered to healthy volunteers in doses up to 150 mg, had no or negligible effect on the ability to drive a car or control machines. At the same time, there are reports of drowsiness noted during treatment with the drug. In this regard, caution is recommended until the individual response to the drug is definitively determined.
Active ingredient
Active ingredient
Fluvoxamine
Composition
Composition
1 film-coated tablet contains:
active ingredient:
fluvoxamine maleate – 50 mg
excipients:
mannitol – 152.0 mg,
corn starch – 40.0 mg,
pregelatinized starch – 6.0 mg,
sodium stearyl fumarate – 1.8 mg,
colloidal silicon dioxide – 0.8 mg
shell:
hypromellose – 4.1 mg,
macrogol 6000 – 1.5 mg,
talc – 0.3 mg,
titanium dioxide (E171) – 1.5 mg.
Pregnancy
Pregnancy
Small observational data do not indicate any adverse effects of fluvoxamine during pregnancy. To date, no other epidemiological data are available.
The potential risk to humans is unknown. The drug should be prescribed to pregnant women with caution.
Isolated cases of withdrawal syndrome in newborns have been described following the use of fluvoxamine late in pregnancy.
Some neonates exposed to selective serotonin reuptake inhibitors in the third trimester of pregnancy experienced feeding and/or breathing difficulties, seizure disorders, unstable body temperature, hypoglycemia, tremors, abnormal muscle tone, hyperexcitability syndrome and continuous crying, which may require longer hospitalization. Fluvoxamine passes into breast milk. In this regard, the drug should not be used during lactation.
Contraindications
Contraindications
hypersensitivity to fluvoxamine maleate or to one of the excipients included in the drug;
simultaneous use of tizanidine and MAO inhibitors.
Treatment with fluvoxamine can be started 2 weeks after stopping an irreversible MAO inhibitor or the day after taking a reversible MAO inhibitor. The time interval between stopping fluvoxamine and starting therapy with any MAO inhibitor should be at least a week.
With caution:
liver and kidney failure;
history of seizures, epilepsy;
old age;
patients with a tendency to bleed (thrombocytopenia);
pregnancy.
Not recommended for the treatment of depression in children (no clinical experience).
Side Effects
Side Effects
The most commonly observed symptom associated with the use of Fevarin is nausea, sometimes accompanied by vomiting. This side effect usually disappears in the first 2 weeks of treatment.
Some side effects observed in clinical trials were often related to symptoms of depression rather than to treatment with Fevarin.
General: often (1–10%) – asthenia, headache, malaise.
From the cardiovascular system: often (1–10%) – palpitations, tachycardia; sometimes (less than 1%) – postural hypotension.
From the gastrointestinal tract: often (1–10%) – abdominal pain, anorexia, constipation, diarrhea, dry mouth, dyspepsia; rarely (less than 0.1%) – impaired liver function (increased levels of liver transaminases).
From the side of the central nervous system: often (1–10%) – nervousness, anxiety, agitation, dizziness, insomnia or drowsiness, tremor; sometimes (less than 1%) – ataxia, confusion, extrapyramidal disorders, hallucinations; rarely (less than 0.1%) – convulsions, manic syndrome.
On the skin: often (1–10%) – sweating; sometimes (less than 1%) – skin hypersensitivity reactions (rash, itching, angioedema); rarely (less than 0.1%) – photosensitivity.
From the musculoskeletal system: sometimes (less than 1%) – arthralgia, myalgia.
From the reproductive system: sometimes (less than 1%) – delayed ejaculation; rarely (less than 0.1%) – galactorrhea.
Other: rarely (less than 0.1%) – change in body weight; serotonergic syndrome, neuroleptic malignant syndrome-like condition, hyponatremia and antidiuretic hormone deficiency syndrome; very rarely – paresthesia, anorgasmia and taste perversion.
When you stop taking fluvoxamine, withdrawal symptoms may develop – dizziness, paresthesia, headache, nausea, anxiety (most symptoms are mild and self-limiting). When discontinuing the drug, a gradual dose reduction is recommended.
Hemorrhagic manifestations – ecchymosis, purpura, gastrointestinal bleeding.
Interaction
Interaction
Fevarin should not be used in combination with MAO inhibitors.
Fluvoxamine is a potent inhibitor of cytochrome P450 1A2, and to a lesser extent, P450 2C and P450 3A4. Drugs that are extensively metabolized by these isoenzymes are eliminated more slowly and may have higher plasma concentrations when coadministered with fluvoxamine. This is especially important for drugs that are characterized by a narrow breadth of therapeutic action. Patients require careful monitoring, and dosage adjustments are recommended if necessary.
Fluvoxamine has minimal inhibitory effects on cytochrome P450 2D6 and appears to have no effect on non-oxidative metabolism or renal excretion.
Cytochrome P450 1A2. With simultaneous use of Fevarin, an increase in previously stable levels of tricyclic antidepressants (clomipramine, imipramine, amitriptyline) and antipsychotics (clozapine, olanzapine), which are largely metabolized by cytochromes P450 1A2, was observed. In this regard, a reduction in the dose of these drugs may be recommended.
Patients concomitantly taking fluvoxamine and drugs with a low therapeutic effect that are metabolized by cytochrome P450 1A2 (such as tacrine, theophylline, methadone, mexiletine) should be closely monitored. If necessary, the dosages of these drugs should be adjusted.
When used in combination with warfarin, a significant increase in warfarin plasma concentrations and prolongation of PT were observed.
Isolated cases of cardiotoxicity have been reported with concomitant use of fluvoxamine with thioridazine.
In studies examining the interactions of Fevarin, an increase in propranolol concentrations was noted after administration of Fevarin. In this regard, it is possible to recommend reducing the dose of propranolol in case of additional administration of Fevarin.
Plasma caffeine levels may increase while taking fluvoxamine. Therefore, if you consume large quantities of drinks containing caffeine and if you develop adverse effects of caffeine such as tremor, palpitations, nausea, anxiety, insomnia, it is necessary to reduce your caffeine intake while taking fluvoxamine.
When taking fluvoxamine and ropinirole simultaneously, the plasma concentration of the latter may increase, thereby increasing the risk of developing an overdose. In such cases, it is recommended to control the dosage of ropinirole or reduce it during treatment with fluvoxamine.
Cytochrome P450 2C. Patients concomitantly taking fluvoxamine and drugs characterized by a low breadth of therapeutic action and undergoing metabolism by cytochrome P450 2C (phenytoin) should be closely monitored, and dosage adjustment of these drugs is recommended.
Patients concomitantly taking fluvoxamine and drugs characterized by a low breadth of therapeutic action and undergoing metabolism by cytochrome P450 3A4 (such as carbamazepine, cyclosporine) should be closely monitored, and dosage adjustment of these drugs is recommended.
When administered concomitantly with fluvoxamine, benzodiazepines that undergo oxidative metabolism, such as triazolam, midazolam, alprazolam and diazepam, may increase their plasma concentrations. The dosage of these benzodiazepines should be reduced while taking fluvoxamine.
Glucuronidation. Fluvoxamine has no effect on plasma digoxin concentrations.
Renal excretion. Fluvoxamine has no effect on plasma concentrations of atenolol.
Pharmacodynamic reactions. In the case of combined use of fluvoxamine with serotonergic drugs (triptans, serotonin reuptake inhibitors), tramadol, the serotonergic effects of fluvoxamine may be enhanced.
Fluvoxamine is used with lithium preparations to treat severely ill patients who respond poorly to pharmacotherapy. Lithium and possibly tryptophan enhance the serotonergic effects of Fevarin and therefore treatment with this combination should be carried out with caution.
When taking oral anticoagulants and fluvoxamine simultaneously, the risk of hemorrhage may increase. Such patients should be under medical supervision.
Overdose
Overdose
Symptoms: The most characteristic symptoms include gastrointestinal disorders (nausea, vomiting and diarrhea), drowsiness and dizziness. In addition, there are reports of cardiac abnormalities (tachycardia, bradycardia, hypotension), liver dysfunction, seizures and coma.
Treatment: There is no specific antidote for fluvoxamine. In case of overdose, gastric lavage is recommended, which should be carried out as soon as possible after taking the drug, as well as symptomatic treatment. In addition, repeated intake of activated carbon is recommended, and, if necessary, the appointment of osmotic laxatives. Forced diuresis or dialysis are not effective.
Storage conditions
Storage conditions
In a dry place, protected from direct sunlight, at a temperature not exceeding 20 °C.
Shelf life
Shelf life
1 year
Manufacturer
Manufacturer
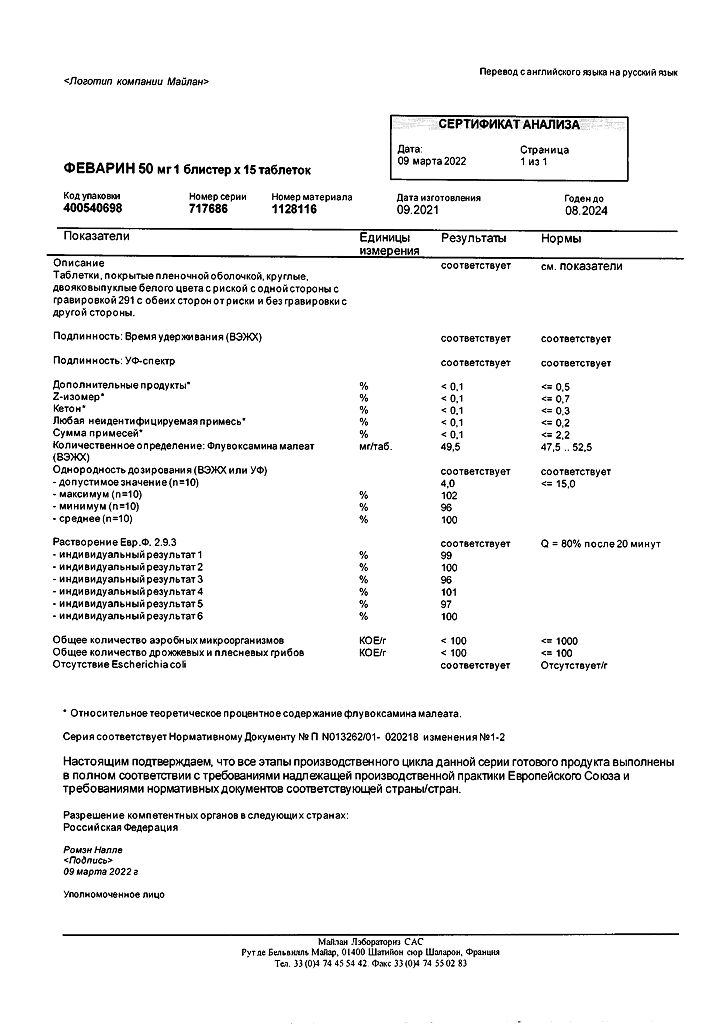
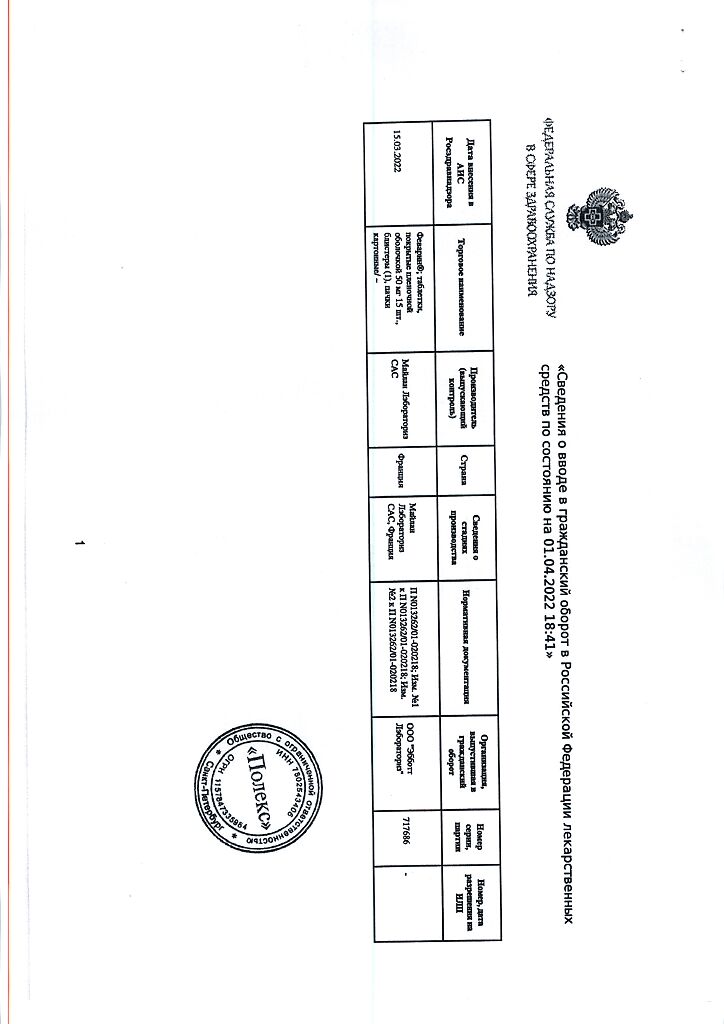
Mylan Laboratories SAS, France
Additional information
| Shelf life | 1 year |
|---|---|
| Conditions of storage | In a dry place, protected from direct sunlight, at a temperature not exceeding 20 °C. |
| Manufacturer | Mylan Laboratories SAS, France |
| Medication form | pills |
| Brand | Mylan Laboratories SAS |
Related products
Buy Fevarin, 50 mg 15 pcs. with delivery to USA, UK, Europe and over 120 other countries.