No products in the cart.
Fervex, 8 pcs.
€11.94 €9.95
Description
Pharmacological properties
Pharmacodynamics
Fervex® is a combination drug that contains paracetamol, pheniramine and ascorbic acid. Paracetamol is a non-narcotic analgesic; it blocks cyclooxygenase, mainly in the central nervous system, affecting the centers of pain and thermoregulation; it has analgesic and antipyretic effects.
Pheniramine is a blocker of H1-histamine receptors, it reduces rhinorrhea and lacrimation, eliminates spasticity, edema and hyperemia of the nasal cavity mucosa, nasopharynx and sinus cavities. Ascorbic acid is involved in the regulation of redox processes, carbohydrate metabolism, blood coagulation, tissue regeneration, the synthesis of steroid hormones, reduces vascular permeability, reduces the need for vitamins B1, B2, A, E, folic acid, pantothenic acid. Improves tolerance of paracetamol and prolongs its action (associated with prolongation of T1/2).
Pharmacokinetics
Paracetamol
After oral administration is quickly absorbed from the gastrointestinal tract. Maximum plasma concentrations of the drug are reached 10-60 minutes after ingestion. It is rapidly distributed throughout the body tissues and penetrates through the blood-brain barrier. Binding to plasma proteins is insignificant and has no therapeutic value, but increases with increasing dose.
Metabolism occurs in the liver, 80% of the taken dose reacts with glucuronic acid and sulfates to form inactive metabolites; 17% undergoes hydroxylation to form 8 active metabolites, which conjugate with glutathione to form inactive metabolites. One of the hydroxylated metabolic intermediates exhibits hepatotoxic effects. This metabolite is neutralized by conjugation with glutathione, but it can cumulate and in case of paracetamol overdose (150 mg paracetamol/kg or 10 g oral paracetamol) cause hepatocyte necrosis. It is excreted by the kidneys as metabolites, mainly as conjugates. Less than 5% of the administered dose is excreted unchanged. The elimination half-life is 1 to 3 hours.
Pheniramine:
It is well absorbed in the digestive tract. The elimination half-life from blood plasma is one to one and a half hours. It is eliminated from the body mainly through the kidneys.
Ascorbic acid:
It is well absorbed in the digestive tract. Time of maximum therapeutic concentration (TCmax ) after oral administration – 4 hours. It is metabolized mainly in liver. It is excreted by the kidneys, through the intestine, with sweat, unchanged and as metabolites.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
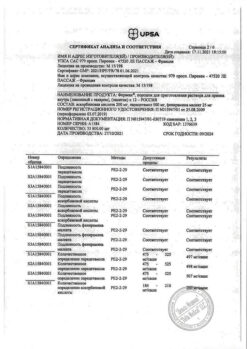
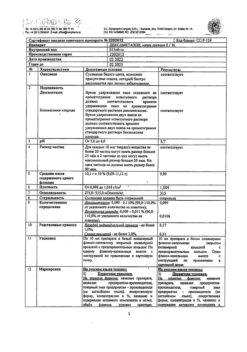
1 sachet contains
The active ingredients:
paracetamol 500 mg,
pheniramine maleate 25 mg,
ascorbic acid 200 mg;
Excipients:
sucrose – 11.555 g,
citric acid – 0.2 g,
acacia gum – 0.1 g,
Sodium saccharinate dihydrate – 0.02 g,
Raspberry flavoring* – 0.15 g.
* composition of raspberry flavoring: ethyl acetate, isoamyl acetate, acetic acid, benzyl alcohol, triacetin, vanillin, p-hydroxy-benzylacetone, maltodextrin, E1450 modified corn starch, E129 dye red charming, E133 dye diamond blue, E110 dye sunset yellow, permastabil 505528 RI, raspberry 054428 A, sodium chloride and/or sodium sulfate.
How to take, the dosage
How to take, the dosage
Inhaled, 1 sachet 2-3 times a day. Before use, the contents of the sachet should be dissolved in a glass (200 ml) of warm water. Maximum duration of treatment is 5 days.
The maximum daily dose of paracetamol in patients weighing more than 50 kg should not exceed 4 g (or 8 sachets of Feverex®); in children or patients weighing 40-50 kg the maximum daily dose of paracetamol should not exceed 3 g; if body weight is less than 40 kg – not more than 2 g.
The interval between doses of the drug should be at least 4 hours.
In patients with impaired renal function (creatinine clearance (CK) <10 ml/min) the interval between doses of the drug should be at least 8 hours.
In patients with chronic or decompensated liver disease, in patients with hepatic insufficiency, chronic alcoholism, in emaciated patients and in patients with dehydration the daily dose of paracetamol should not exceed 3 g.
The drug should not be taken more than 3 days as an antipyretic and more than 5 days as a pain reliever.
If there is no relief of symptoms within 5 days of starting the drug, the fever persists, or after an initial decrease the fever suddenly rises again, the patient should see a doctor.
Interaction
Interaction
Ethanol increases the sedative effect of antihistamines (pheniramine), therefore its intake during treatment with the drug Feverex® should be avoided. In addition, ethanol in concomitant use with pheniramine promotes the development of acute pancreatitis.
Pheniramine increases the effect of sedatives: Morphine derivatives, barbiturates, benzodiazepine and other tranquilizers, neuroleptics (meprobamate, phenothiazine derivatives), antidepressants (amitriptyline, mirtazapine, mianserine), hypotensive drugs of central action, sedatives belonging to the group of blockers of histamine H1-receptors, and baclofen, which not only increase sedation, but also increase the risk of side effects of the drug (urinary retention, dry mouth, constipation).
The possibility of increased central m-cholin-blocking effects when used in combination with other drugs with m-cholin-blocking activity (other histamine Hsub>1 receptors, tricyclic antidepressants, phenothiazine neuroleptics, antispasmodics and antiparkinsonics with m-cholinoblocking activity, disopyramide).
When the drug is used with microsomal oxidation inducers: barbiturates, tricyclic antidepressants, anticonvulsants (phenytoin), flumecinol, phenylbutazone, rifampicin and ethanol, the risk of hepatotoxic effects increases significantly (due to the included paracetamol).
The use of GCS at the same time increases the risk of glaucoma.
Concomitant use with salicylates increases the risk of nephrotoxic effects.
Concomitant use with chloramphenicol (levomycetin) increases the toxicity of the latter.
Paracetamol increases the effect of indirect anticoagulants and decreases the effectiveness of uricosuric drugs.
Ascorbic acid increases the blood concentration of benzylpenicillin and tetracyclines; at a dose of 1 g/day it increases the bioavailability of ethinylestradiol (including those included in oral contraceptives).
Ascorbic acid improves intestinal absorption of iron preparations (converts trivalent to divalent iron); it may increase iron excretion if used concomitantly with deferoxamine.
Ascorbic acid reduces the effectiveness of heparin and indirect anticoagulants.
Concomitant use with acetylsalicylic acid (ASA) increases urinary excretion of ascorbic acid and decreases excretion of ASA. Asc reduces the absorption of ascorbic acid by about 30%. It increases the risk of crystalluria during treatment with short-acting salicylates and sulfonamides, slows renal excretion of acids, increases excretion of drugs with alkaline reaction (including alkaloids), reduces the blood concentration of oral contraceptives.
Ascorbic acid increases total clearance of ethanol, which in turn reduces the concentration of ascorbic acid in the body.
The quinoline-type drugs, calcium chloride, salicylates, GCS deplete ascorbic acid reserves with long-term use.
Askorbic acid decreases the chronotropic effect of isoprenaline when used concomitantly.
Askorbic acid may interfere with the interaction between disulfiram and ethanol when used long-term or in high doses.
In high doses ascorbic acid increases excretion of mexiletine by the kidneys.
Barbiturates and primidone increase excretion of ascorbic acid in the urine.
Ascorbic acid reduces the therapeutic effects of neuroleptics – phenothiazine derivatives, tubal reabsorption of amphetamine and tricyclic antidepressants.
Special Instructions
Special Instructions
Contraindications
Contraindications
Side effects
Side effects
The drug is well tolerated in the recommended doses. The following side effects have been reported with the use of the drug (frequency has not been determined).
Hematopoietic system disorders: anemia, leukopenia, agranulocytosis, thrombocytopenia.
Immune system disorders: allergic reactions (erythema, skin rash, pruritus, Quincke’s edema, anaphylactic shock).
Nervous system disorders: somnolence, mental confusion, hallucinations, concentration disorders (more often in elderly patients), agitation, nervousness, insomnia, coordination dysfunction, tremor.
With the visual organ: impaired accommodation.
Cardiovascular system: palpitations, orthostatic hypotension, dizziness.
Gastrointestinal system: dry mouth, nausea, vomiting, abdominal pain, constipation.
Urinary system disorders: impaired urination.
In case of adverse reactions, the patient should stop taking the drug and see a physician.
Overdose
Overdose
Symptoms due to the action of paracetamol
. In overdose, intoxication is possible, especially in elderly patients, children, patients with liver disease (caused by chronic alcoholism), in patients with malnutrition, as well as in patients taking microsomal liver enzyme inducers, which may develop fulminant hepatitis, liver failure, cholestatic hepatitis, in the above cases – sometimes with a fatal outcome. The threshold of overdose in these categories of patients may be lower. The clinical picture of acute overdose develops within 24 hours after taking paracetamol.
Symptoms: gastrointestinal disorders (nausea, vomiting, decreased appetite, abdominal discomfort and (or) abdominal pain), pale skin. When administered to adults 7.5 g or more or children more than 140 mg/kg at a time, cytolysis of hepatocytes with complete irreversible liver necrosis, development of liver failure, metabolic acidosis and encephalopathy occurs, which may lead to coma and death. 12-48 hours after paracetamol administration there is an increase in the activity of microsomal liver enzymes, lactate dehydrogenase, bilirubin concentration and decrease in prothrombin concentration. Clinical symptoms of liver damage appear 2 days after overdose of the drug and reach their maximum on the 4th-6th day.
Treatment: immediate hospitalization. Determination of the quantitative content of paracetamol in blood plasma before treatment as soon as possible after overdose. Administration of SH-group donators and precursors of glutathione synthesis – methionine and acetylcystine – is most effective during the first 8 hours. The need for additional therapeutic measures (further methionine administration, IV administration of acetylcysteine) is determined depending on the concentration of paracetamol in the blood, as well as the time elapsed after its administration. Symptomatic treatment. Laboratory tests of microsomal liver enzyme activity should be performed at the beginning of treatment and then every 24 hours. In most cases, microsomal liver enzyme activity normalizes within 1-2 weeks. In very severe cases, a liver transplant may be required.
Symptoms caused by the action of ascorbic acid
Symptoms: nausea, diarrhea, irritation of gastrointestinal mucosa, flatulence, abdominal pain of spastic nature, frequent urination, nephrolithiasis, insomnia, irritability, hypoglycemia.
Treatment: immediately stop using the drug and consult a physician. Treatment is symptomatic, forced diuresis.
Pheniramine-related symptoms
Symptoms: seizures, impaired consciousness, coma.
Treatment: stop using the drug immediately and seek medical attention. Gastric lavage, enterosorbents (activated charcoal, lignin hydrolysis), intravenous or oral administration of antidote acetylcysteine (if possible, in the first 10 hours after overdose), symptomatic treatment are recommended.
Pregnancy use
Pregnancy use
An adequate and well-controlled study of Fervex® in pregnant women has not been conducted, therefore it is not recommended to use the drug in this group of patients.
It is unknown whether the active ingredients of the drug penetrate into breast milk. The drug should not be used during lactation.
Similarities
Similarities
Additional information
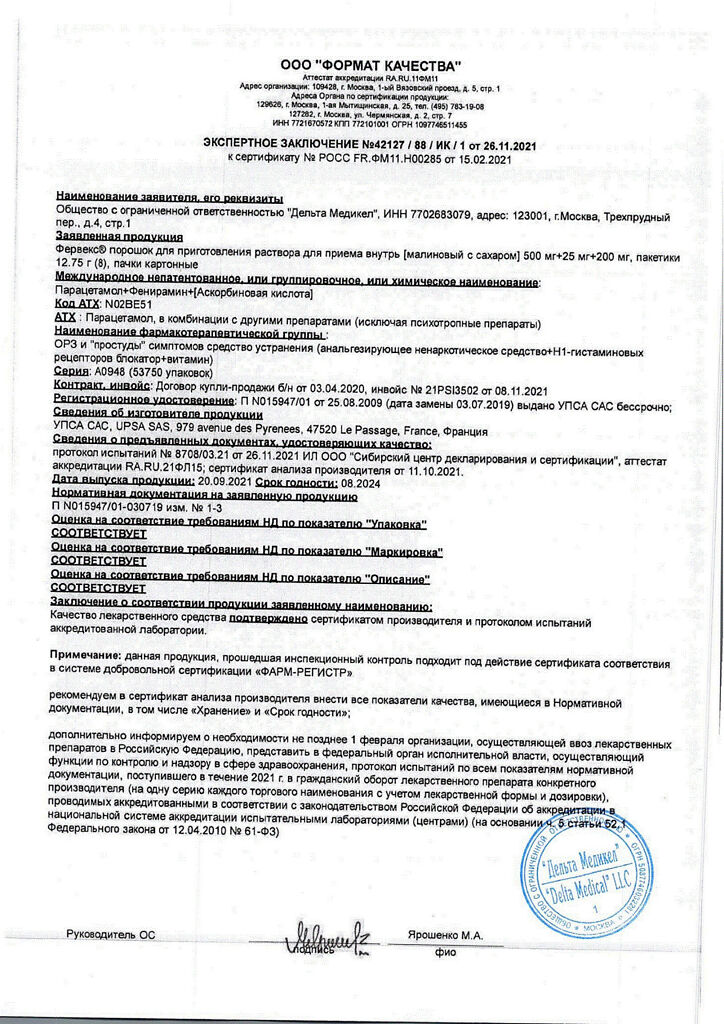
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store at the temperature from 15 to 25 oC. Keep out of reach of children. |
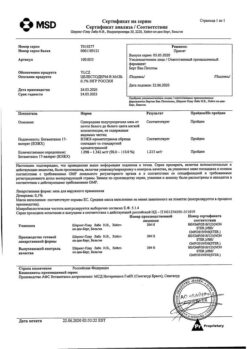
| Manufacturer | UTSA SAS, France |
| Medication form | Powder for preparation of solution for oral administration |
| Brand | UTSA SAS |
Other forms…
Related products
Buy Fervex, 8 pcs. with delivery to USA, UK, Europe and over 120 other countries.