No products in the cart.
Description
Pharmacodynamics
Antitumor drug. It has anti-estrogenic action, selectively inhibits aromatase (enzyme of estrogen synthesis) by a highly specific competitive binding to a subunit of this enzyme – cytochrome P450 heme. It blocks estrogen synthesis in both peripheral and tumor tissues.
In postmenopausal women, estrogens are produced mainly by the aromatase enzyme, which converts androgens synthesized in the adrenal glands (primarily androstenedione and testosterone) into estrone and estradiol.
Daily administration of letrozole at a daily dose of 0.1-5 mg leads to a decrease in plasma concentrations of estradiol, estrone and estrone sulfate by 75-95% of the initial content. Suppression of estrogen synthesis is maintained throughout treatment.
When Femara® is used in a dose range of 0.1 to 5 mg there is no disruption of steroid hormone synthesis in the adrenal glands, the ACTH test shows no disruption of aldosterone or cortisol synthesis. No additional prescription of glucocorticoids and mineralocorticoids is required.
Blockade of estrogen biosynthesis does not lead to the accumulation of androgens, which are precursors of estrogen. No changes in plasma concentrations of luteinizing and follicle stimulating hormones, changes in thyroid function, changes in lipid profile, and increased incidence of myocardial infarctions and strokes were observed during Femara treatment.
The incidence of osteoporosis slightly increased with Femara treatment (6.9% compared to 5.5% in the placebo group). However, the incidence of bone fractures in patients treated with Femara® does not differ from that in healthy individuals of the same age.
Adjuvant therapy with Femara for early breast cancer reduces the risk of progression, increases survival without signs of disease for 5 years, and reduces the risk of developing another breast tumor.
The extended adjuvant therapy with Femara reduces the risk of progression by 42%. A significant benefit in disease-free survival was observed in the Femara group regardless of lymph node involvement. Femara® treatment reduced mortality among patients with lymph node involvement by 40%.
Pharmacokinetics
Intake
Letrozole is quickly and completely absorbed from the GI tract (average bioavailability is 99.9%). Food intake slightly reduces the absorption rate. The average value of Tmax letrozole in blood is 1 h when Femara is taken on an empty stomach and 2 h when taken with food; the average value of Cmax is 129±20.3 nmol/L when taken on an empty stomach and 98.7±18.6 nmol/L when taken with food, but the absorption rate of letrozole (as assessed by AUC) is unchanged. Slight changes in absorption rate are considered to be of no clinical significance, so letrozole can be taken regardless of food intake.
Distribution
The binding of letrozole to plasma proteins is approximately 60% (predominantly to albumin – 55%). The concentration of letrozole in erythrocytes is about 80% of its level in blood plasma. The apparent Vd during equilibrium is approximately 1.87±0.47 L/kg. Css is achieved over 2-6 weeks of daily administration of a daily dose of 2.5 mg. Pharmacokinetics are nonlinear. No cumulation has been noted with long-term use.
Metabolism
Letrozole is largely metabolized by the CYP3A4 and CYP2A6 isoenzymes to form a pharmacologically inactive carbinol compound.
Extracted mainly by kidneys as metabolites, to a lesser extent – through intestine. The final T1/2 is 48 hours.
Pharmacokinetics in special clinical cases
The pharmacokinetic parameters of letrozole are independent of patient age.
In renal insufficiency pharmacokinetic parameters do not change.
In patients with moderate hepatic impairment (Child-Pugh class B) mean AUC values, although higher by 37%, remain within the range of values observed in persons without hepatic impairment. In patients with cirrhosis and severe liver dysfunction (grade C according to Child-Pugh scale) AUC is increased by 95% and T1/2 by 187%. However, given the good tolerability of high doses of the drug (5-10 mg/day) in these cases there is no need to change the dose of letrozole.
Indications
Indications
Early stages of breast cancer, the cells of which have hormone receptors, in postmenopausal women, as adjuvant therapy.
Early stages of breast cancer in postmenopausal women after completion of standard adjuvant therapy with tamoxifen as extended adjuvant therapy.
Common hormone-dependent forms of breast cancer in postmenopausal women (first-line therapy).
Common forms of breast cancer in postmenopausal women (natural or artificially induced) who have received previous antiestrogens therapy.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Antitumor drug. It has an antiestrogenic effect, selectively inhibits aromatase (the enzyme of estrogen synthesis) through highly specific competitive binding to the subunit of this enzyme – the heme of cytochrome P450. Blocks estrogen synthesis in both peripheral and tumor tissues.
In postmenopausal women, estrogens are formed mainly with the participation of the enzyme aromatase, which converts androgens synthesized in the adrenal glands (primarily androstenedione and testosterone) into estrone and estradiol.
Daily intake of letrozole in a daily dose of 0.1-5 mg leads to a decrease in the concentration of estradiol, estrone and estrone sulfate in the blood plasma by 75-95% of the initial content. Suppression of estrogen synthesis is maintained throughout treatment.
When using the drug Femara® in the dose range from 0.1 to 5 mg, disturbances in the synthesis of steroid hormones in the adrenal glands are not observed, and the ACTH test does not reveal disturbances in the synthesis of aldosterone or cortisol. Additional administration of glucocorticoids and mineralocorticoids is not required.
Blockade of estrogen biosynthesis does not lead to the accumulation of androgens, which are estrogen precursors. While taking Femara, there were no changes in the concentrations of luteinizing and follicle-stimulating hormones in the blood plasma, changes in thyroid function, changes in the lipid profile, or an increase in the frequency of myocardial infarction and strokes.
During treatment with Femara, the incidence of osteoporosis slightly increased (6.9% compared to 5.5% in the placebo group). However, the incidence of bone fractures in patients receiving Femara® does not differ from that in healthy people of the same age.
Adjuvant therapy with Femara in early stages of breast cancer reduces the risk of progression, increases disease-free survival for 5 years, and reduces the risk of developing a tumor in another breast.
Extended adjuvant therapy with Femara reduces the risk of progression by 42%. A significant advantage in disease-free survival in the Femara group was observed regardless of lymph node involvement. Treatment with Femara® reduces mortality among patients with lymph node involvement by 40%.
Pharmacokinetics
Suction
Letrozole is quickly and completely absorbed from the gastrointestinal tract (average bioavailability is 99.9%). Eating slightly reduces the rate of absorption. The average Tmax of letrozole in the blood is 1 hour when taking Femara on an empty stomach and 2 hours when taken with food; the average Cmax value is 129±20.3 nmol/l when taken on an empty stomach and 98.7±18.6 nmol/l when taken with food, but the degree of absorption of letrozole (as assessed by AUC) does not change. Minor changes in the rate of absorption are considered to be of no clinical significance, so letrozole can be taken with or without food.
Distribution
The binding of letrozole to plasma proteins is approximately 60% (mainly with albumin – 55%). The concentration of letrozole in erythrocytes is about 80% of its level in blood plasma. The apparent Vd during the equilibrium period is about 1.87 ± 0.47 l/kg. Css is achieved within 2-6 weeks of daily intake of a daily dose of 2.5 mg. Pharmacokinetics is nonlinear. No accumulation was observed with long-term use.
Metabolism
Letrozole is extensively metabolized by the isoenzymes CYP3A4 and CYP2A6 to form a pharmacologically inactive carbinol compound.
Removal
It is excreted primarily by the kidneys in the form of metabolites, and to a lesser extent through the intestines. The final T1/2 is 48 hours.
Pharmacokinetics in special clinical situations
The pharmacokinetic parameters of letrozole do not depend on the age of the patient.
In renal failure, pharmacokinetic parameters do not change.
With moderately severe liver dysfunction (Child-Pugh class B), the average AUC values, although 37% higher, remain within the range of values observed in individuals without liver dysfunction. In patients with cirrhosis of the liver and severe impairment of its function (class C on the Child-Pugh scale), AUC increases by 95% and T1/2 by 187%. However, given the good tolerability of high doses of the drug (5-10 mg/day), in these cases there is no need to change the dose of letrozole.
Special instructions
Special instructions
Patients with severely impaired liver function should be under constant supervision.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
Some side effects of the drug, such as general weakness and dizziness, may affect the ability to perform potentially hazardous activities that require concentration and quick reactions.
In this regard, care should be taken when operating vehicles and machinery.
Active ingredient
Active ingredient
Letrozole
Composition
Composition
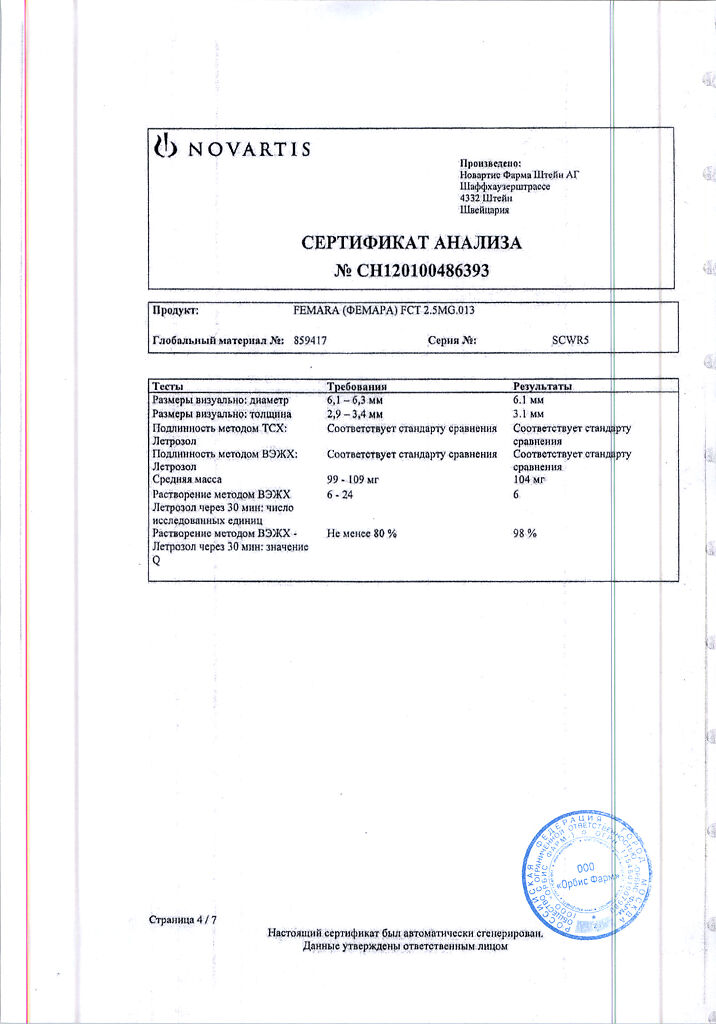
1 tablet contains:
Active ingredients:
letrozole 2.5 mg.
Excipients:
lactose monohydrate,
microcrystalline cellulose,
corn starch,
sodium carboxymethyl starch,
colloidal silicon dioxide,
magnesium stearate,
hypromellose,
talc,
macrogol 8000,
iron oxide dye yellow (17268),
titanium dioxide
There are 10 tablets in a blister.
There are 3 blisters in a cardboard package.
Pregnancy
Pregnancy
Femara® is contraindicated for use during pregnancy and lactation.
During Femara therapy, given the potential for pregnancy, perimenopausal and early postmenopausal women should use reliable methods of contraception until stable postmenopausal hormonal levels are established.
Contraindications
Contraindications
Endocrine status characteristic of the reproductive period;
pregnancy;
lactation period (breastfeeding);
children and adolescents up to 18 years of age;
hypersensitivity to letrozole or any other component of the drug.
there is no data on the use of Femara® in patients with creatinine clearance less than 10 ml/min. Before prescribing Femara, such patients should carefully weigh the balance between the potential risk and the expected effect of treatment.
Side Effects
Side Effects
The incidence of side effects is estimated as follows:
occurring very frequently (≥10%);
often (≥1, <10%);
sometimes (≥0.1%, <1%);
rare (≥0.01, <0.1%);
very rare (<0.01%, including isolated reports).
As a rule, adverse reactions were mild or moderate and were mainly associated with suppression of estrogen synthesis.
From the digestive system: often – nausea, vomiting, dyspepsia, constipation, diarrhea; sometimes – abdominal pain, stomatitis, dry mouth, increased activity of liver enzymes.
From the central nervous system and peripheral nervous system: often – headache, dizziness, depression; sometimes – anxiety, nervousness, irritability, drowsiness, insomnia, memory impairment, dysesthesia, paresthesia, hypoesthesia, taste disturbances, episodes of cerebrovascular accident.
From the hematopoietic system: sometimes – leukopenia.
From the cardiovascular system: sometimes – palpitations, tachycardia, thrombophlebitis of superficial and deep veins, increased blood pressure, coronary artery disease (angina pectoris, myocardial infarction, heart failure), thromboembolism; rarely – pulmonary embolism, arterial thrombosis, stroke.
From the respiratory system: sometimes – shortness of breath, cough.
Dermatological reactions: often – alopecia, increased sweating, skin rash (including erythematous, maculopapular, vesicular rash, psoriasis-like rash); sometimes – itching, dry skin, urticaria; very rarely – angioedema, anaphylactic reactions.
From the musculoskeletal system: very often – arthralgia; often – myalgia, bone pain, osteoporosis, bone fractures; sometimes – arthritis.
From the senses: sometimes – cataracts, eye irritation, blurred vision, impaired taste.
From the urinary system: sometimes – frequent urination, urinary tract infections.
From the reproductive system: sometimes – vaginal bleeding, vaginal discharge, vaginal dryness, pain in the mammary glands.
Other: very often – paroxysmal sensations of heat (hot flashes); often – increased fatigue, asthenia, malaise, peripheral edema, weight gain, hypercholesterolemia, anorexia, increased appetite; sometimes – weight loss, thirst, hyperthermia (pyrexia), dry mucous membranes, generalized edema, pain in tumor foci.
Interaction
Interaction
When letrozole is co-administered with cimetidine and warfarin, no clinically significant interaction is observed.
There is currently no clinical experience with the use of letrozole in combination with other antitumor agents.
According to the results of in vitro studies, letrozole suppresses the activity of cytochrome P450 isoenzymes 2A6 and 2C19 (the latter moderately). When deciding on the clinical significance of these data, it is necessary to take into account that the CYP2A6 isoenzyme does not play a significant role in the metabolism of drugs.
In vitro experiments have shown that letrozole, used at concentrations 100 times higher than equilibrium plasma values, does not have the ability to significantly inhibit the metabolism of diazepam (a substrate for CYP2C19).
Thus, clinically significant interactions with the CYP2C19 isoenzyme are unlikely. However, caution should be exercised when concomitantly using letrozole and drugs that are metabolized primarily with the participation of the above-mentioned isoenzymes and have a narrow therapeutic index.
Overdose
Overdose
There are isolated reports of cases of overdose of Femara®.
Treatment: There are no specific treatments for overdose.
Symptomatic and supportive therapy is indicated. Letrozole is eliminated from plasma during hemodialysis.
Storage conditions
Storage conditions
In a dry place, at a temperature not exceeding 30 °C
Shelf life
Shelf life
5 years
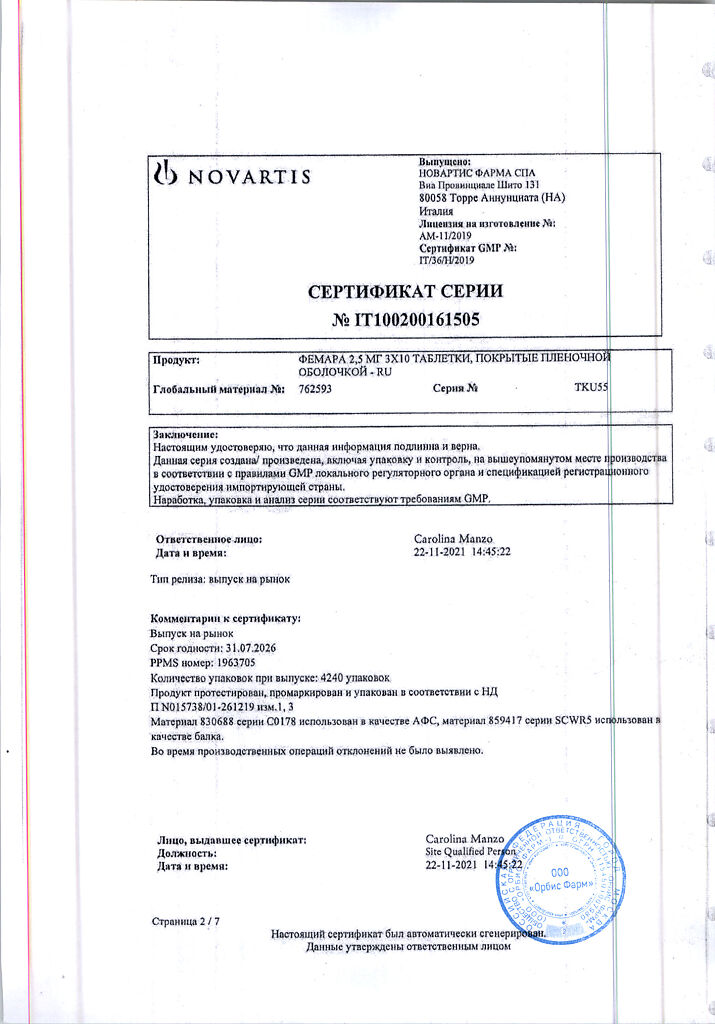
Manufacturer
Manufacturer
Novartis Pharma GmbH, Germany
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | In a dry place, at a temperature no higher than 30 °C |
| Manufacturer | Novartis Pharma GmbH, Germany |
| Medication form | pills |
| Brand | Novartis Pharma GmbH |
Related products
Buy Femara, 2,5mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.