No products in the cart.
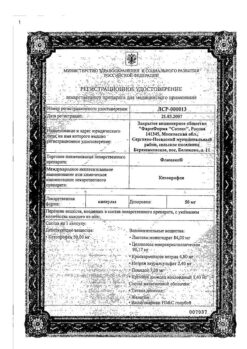
Etorelex, 120 mg 7 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: Non-steroidal anti-inflammatory drugs (NSAIDs).
TATX code: M01AN05
Pharmacological properties
Pharmacodynamics
Etoricoxib is a selective cyclooxygenase-2 (COX-2) inhibitor when taken orally in therapeutic concentrations. In clinical pharmacological studies, etoricoxib inhibited COX-2 in a dose-dependent manner, with no effect on COX-1 at a daily dose up to 150 mg. The drug does not inhibit the synthesis of prostaglandins in the gastric mucosa and does not affect platelet function.
Cyclooxygenase is responsible for the formation of prostaglandins. Two isoforms of cyclooxygenase, COX-1 and COX-2, have been identified. COX-2 is an isoenzyme that is induced by various proinflammatory mediators and is considered the main enzyme responsible for the synthesis of prostanoid mediators of pain, inflammation and fever. COX-2 is involved in the processes of ovulation, implantation and closure of the arterial duct, regulation of renal and CNS function (induction of fever, sensation of pain, cognitive function), and may also play a role in the process of ulcer healing. COX-2 has been detected in the tissues surrounding gastric ulcers in humans, but its importance in ulcer healing has not been established.
Efficacy
In patients with osteoarthritis (OA), etoricoxib, administered at a dose of 60 mg once daily, provided a significant reduction in pain and improvement in patients’ assessment of their condition. These favorable effects were observed on the second day of treatment and persisted for 52 weeks. Studies of etoricoxib at a dose of 30 mg once daily (using similar evaluation methods) demonstrated efficacy compared to placebo during the treatment period of 12 weeks. In a study conducted to determine the optimal dose, etoricoxib, when used at a dose of 60 mg, demonstrated significantly greater improvement than the 30 mg dose for all three primary endpoints after 6 weeks of treatment. The 30 mg dose has not been studied in hand osteoarthritis.
In patients with rheumatoid arthritis (RA), etoricoxib at a dose of 90 mg once daily provided a significant reduction in pain and inflammation and improved mobility. These favorable effects were maintained during the treatment period of 12 weeks.
In patients with acute gouty arthritis, etoricoxib, administered at a dose of 120 mg once daily for the entire treatment period of 8 days, reduced moderate to severe joint pain and inflammation. The efficacy was comparable to that of indomethacin when used in a dose of 50 mg 3 times/day. Decrease in pain was noted as early as 4 hours after the start of treatment.
In patients with ankylosing spondylitis, etoricoxib at a dose of 90 mg once daily provided a significant reduction in back pain, inflammation, stiffness, and improved function. The clinical efficacy of etoricoxib was observed as early as the second day of treatment and was maintained throughout the entire treatment period of 52 weeks.
In a clinical study of pain after dental surgery, etoricoxib at a dose of 90 mg was administered once daily for 3 days. In a subgroup of patients with moderate pain (at baseline assessment), etoricoxib had the same analgesic effect as ibuprofen at a dose of 90 mg (16.11 vs. 16.39 P=0.722), and was superior to the paracetamol/codeine combination at a dose of 600 mg/60 mg (11.00; P<0.001) and placebo (6.84; P<0.001) according to the overall pain reduction score, within the first 6 h (TOPAR6). The proportion of patients who required rapid-acting pain medication within the first 24 h after taking the study drugs was 40.8% with etoricoxib at 90 mg, 25.5% with ibuprofen at 600 mg every 6 h, and 46.7% with the paracetamol/codein combination at 600 mg/60 mg every 6 h, compared with 76.2% in the placebo group. In this study, the median onset of action (perceived pain reduction) with etoricoxib at a dose of 90 mg was 28 minutes after administration.
Pharmacokinetics
Absorption
Etoricoxib is rapidly absorbed when taken orally. Absolute bioavailability when taken orally is about 100%. After the drug is taken by adults on an empty stomach in a dose of 120 mg once a day the maximum concentration (Cmax) is 3.6 mcg/ml, time to reach Cmax – 1 hour after intake. Geometric mean AUC0-24h is 37.8 µg×h/ml. Pharmacokinetics of etoricoxib within therapeutic doses is linear.
When taking etoricoxib at a dose of 120 mg with meals (high-fat meals) there was no clinically significant effect on the degree of absorption. The rate of absorption was altered, resulting in a 36% decrease in Cmax and a 2 h increase in TCmax. These results are not considered clinically significant. In clinical trials, etoricoxib was used independently from food intake.
Distribution
Tericoxib is approximately 92% bound to human plasma proteins at concentrations of 0.05-5 µg/mL. The volume of distribution (Vdss) in the equilibrium state is about 120 l. Etoricoxib penetrates through the placental barrier and the blood-brain barrier.
Metabolism
Etoricoxib is extensively metabolized. Less than 1% of etoricoxib is excreted unchanged by the kidneys. The main route of metabolism is the formation of 6′-hydroxymethylethoricoxib, catalyzed by enzymes of the cytochrome system. CYP3A4 contributes to the metabolism of etoricoxib in vivo. In vitro studies indicate that the CYP2D6, CYP2C9, CYP1A2 and CYP2C19 isoenzymes can also catalyze the major metabolic pathway, but their quantitative effects in vivo have not been studied.
In humans, 5 metabolites of etoricoxib have been identified. The main metabolite is 6′-carboxyacetyl etoricoxib, which is formed by additional oxidation of 6′-hydroxymethyl etoricoxib. These major metabolites have no appreciable activity or are weak COX-2 inhibitors. None of these metabolites inhibits COX-1.
On a single intravenous administration of labeled radioactive etoricoxib at a dose of 25 mg to healthy volunteers, 70% of etoricoxib was excreted by the kidneys, 20% – through the intestine, mostly as metabolites. Less than 2% was found unchanged.
The excretion of etoricoxib is mainly by metabolism with subsequent excretion by the kidneys.
The equilibrium concentration is reached when 120 mg of etoricoxib is taken daily after 7 days with a cumulation coefficient of about 2, which corresponds to a half-life of about 22 hours. Plasma clearance after 25 mg by IV is approximately 50 ml/min.
Particular patient groups
Elderly
The pharmacokinetics in elderly patients (65 years and older) is comparable to that in younger patients.
Per sex
The pharmacokinetics of etoricoxib are similar in men and women.
Hepatic impairment
In patients with mild hepatic impairment (Child-Pugh score 5-6) taking etoricoxib at a dose of 60 mg once daily was associated with a 16% increase in AUC compared to healthy subjects taking the drug at the same dose.
In patients with moderate hepatic dysfunction (Child-Pugh score 7-9) taking etoricoxib at a dose of 60 mg every other day, the average AUC was the same as in healthy subjects taking etoricoxib daily at the same dose. Etoricoxib at a dose of 30 mg once daily has not been studied in this population.
There are no clinical or pharmacokinetic studies in patients with severe hepatic impairment (≥10 Child-Pugh score).
Renal Impairment
The pharmacokinetic parameters of a single dose of etoricoxib 120 mg in patients with moderate to severe renal impairment and with end-stage chronic renal failure (CKF) on hemodialysis were not significantly different from those in healthy subjects. Hemodialysis had little effect on excretion (dialysis clearance was about 50 ml/min).
Children
The pharmacokinetic parameters of etoricoxib in children younger than 12 years have not been studied.
. In a pharmacokinetic study (n=16) conducted in adolescents aged 12 to 17 years, the pharmacokinetics in adolescents weighing 40 to 60 kg when taking etoricoxib at a dose of 60 mg once daily and in those weighing more than 60 kg when taking etoricoxib at a dose of 90 mg once daily were similar to the pharmacokinetics in adults when taking etoricoxib at a dose of 90 mg once daily. The safety and efficacy of etoricoxib in children have not been established.
Indications
Indications
Symptomatic treatment of osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, pain and inflammation associated with acute gouty arthritis.
Short-term treatment of moderate acute pain after dental surgery.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: non-steroidal anti-inflammatory drugs (NSAIDs).
ATX code: M01AH05
Pharmacological properties
Pharmacodynamics
Etoricoxib, when administered orally at therapeutic concentrations, is a selective cyclooxygenase-2 (COX-2) inhibitor. In clinical pharmacological studies, etoricoxib dose-dependently inhibited COX-2 without affecting COX-1 at daily doses of up to 150 mg. The drug does not inhibit the synthesis of prostaglandins in the gastric mucosa and does not affect platelet function.
Cyclooxygenase is responsible for the formation of prostaglandins. Two isoforms of cyclooxygenase have been isolated – COX-1 and COX-2. COX-2 is an isoenzyme that is induced by various proinflammatory mediators and is considered as the main enzyme responsible for the synthesis of prostanoid mediators of pain, inflammation and fever. COX-2 is involved in the processes of ovulation, implantation and closure of the ductus arteriosus, regulation of kidney and central nervous system function (induction of fever, pain sensation, cognitive function), and may also play a role in the healing process of ulcers. COX-2 has been found in tissue surrounding human gastric ulcers, but its importance in ulcer healing has not been established.
Efficiency
In patients with osteoarthritis (OA), etoricoxib, when used at a dose of 60 mg 1 time/day, provided a significant reduction in pain and improved patient assessment of their condition. These beneficial effects were observed as early as the second day of treatment and persisted for 52 weeks. Studies of etoricoxib at a dose of 30 mg once daily (using similar assessment methods) demonstrated efficacy compared with placebo over a treatment period of 12 weeks. In an optimal dose determination study, etoricoxib 60 mg demonstrated significantly greater improvement than 30 mg for all three primary endpoints after 6 weeks of treatment. The 30 mg dose has not been studied in osteoarthritis of the hand joints.
In patients with rheumatoid arthritis (RA), etoricoxib, when used at a dose of 90 mg 1 time / day, provided a significant reduction in pain and inflammation and improved mobility. These beneficial effects were maintained over a 12-week treatment period.
In patients with acute gouty arthritis, etoricoxib, when administered at a dose of 120 mg 1 time / day for the entire treatment period of 8 days, reduced moderate to severe joint pain and inflammation. The effectiveness was comparable to the effectiveness of indomethacin when used at a dose of 50 mg 3 times a day. A decrease in pain was noted within 4 hours after the start of treatment.
In patients with ankylosing spondylitis, etoricoxib, when used at a dose of 90 mg 1 time/day, provided a significant reduction in back pain, inflammation, stiffness, and improvement in function. Clinical efficacy of etoricoxib was observed as early as the second day of treatment and was maintained throughout the 52-week treatment period.
In a clinical study examining pain after dental surgery, etoricoxib 90 mg was administered once a day for 3 days. In the subgroup of patients with moderate pain (at baseline), etoricoxib 90 mg had the same analgesic effect as ibuprofen 600 mg (16.11 vs. 16.39; P=0.722) and was superior to paracetamol/codeine 600 mg/60 mg (11.00; P<0.722). 0.001) and placebo (6.84; P < 0.001) according to the total pain reduction score during the first 6 hours (TOPAR6). The proportion of patients who required rapid-acting pain medications within the first 24 hours of study drug use was 40.8% with etoricoxib 90 mg, 25.5% with ibuprofen 600 mg every 6 hours, and 46.7% with paracetamol/codeine 600 mg/60 mg every 6 hours, compared with 76.2% in placebo group. In this study, the median onset of action (perceived pain relief) with etoricoxib 90 mg was 28 minutes after dosing.
Pharmacokinetics
Absorption
Etoricoxib is rapidly absorbed when taken orally. Absolute bioavailability when taken orally is about 100%. After taking the drug by adults on an empty stomach at a dose of 120 mg 1 time/day, the maximum concentration (Cmax) is 3.6 mcg/ml, the time to reach Cmax is 1 hour after administration. The geometric mean AUC0-24h is 37.8 mcg×h/ml. The pharmacokinetics of etoricoxib within therapeutic doses is linear.
When etoricoxib 120 mg was taken with food (high fat meal), no clinically significant effect on absorption was observed. The rate of absorption was altered, resulting in a 36% decrease in Cmax and an increase in TCmax by 2 hours. These results are not considered clinically significant. In clinical studies, etoricoxib was administered without regard to meals.
Distribution
Etoricoxib is approximately 92% bound to plasma proteins in humans at concentrations of 0.05-5 mcg/ml. The volume of distribution (Vdss) at equilibrium is approximately 120 l. Etoricoxib penetrates the placental barrier and the blood-brain barrier.
Metabolism
Etoricoxib is extensively metabolized. Less than 1% of etoricoxib is excreted unchanged by the kidneys. The main route of metabolism is the formation of 6′-hydroxymethyletoricoxib, catalyzed by enzymes of the cytochrome system. CYP3A4 contributes to the metabolism of etoricoxib in vivo. In vitro studies indicate that the isoenzymes CYP2D6, CYP2C9, CYP1A2 and CYP2C19 can also catalyze the major metabolic pathway, but their quantitative effects in vivo have not been studied.
Five metabolites of etoricoxib have been detected in humans. The main metabolite is 6′-carboxyacetyletoricoxib, formed by additional oxidation of 6′-hydroxymethylethoricoxib. These main metabolites do not have significant activity or are weak inhibitors of COX-2. None of these metabolites inhibit COX-1.
Removal
With a single intravenous administration of labeled radioactive etoricoxib to healthy volunteers at a dose of 25 mg, 70% of etoricoxib was excreted by the kidneys, 20% through the intestines, mainly in the form of metabolites. Less than 2% was found unchanged.
Elimination of etoricoxib occurs primarily through metabolism followed by renal excretion.
The equilibrium concentration is achieved with a daily dose of 120 mg of etoricoxib after 7 days with an accumulation coefficient of about 2, which corresponds to a half-life of about 22 hours. Plasma clearance after intravenous administration of 25 mg is approximately 50 ml/min.
Special patient groups
Elderly
Pharmacokinetics in elderly patients (65 years and older) are comparable to pharmacokinetics in young patients.
Floor
The pharmacokinetics of etoricoxib are similar in men and women.
Liver failure
In patients with mild liver dysfunction (5-6 points on the Child-Pugh scale), taking etoricoxib at a dose of 60 mg 1 time / day was accompanied by an increase in AUC by 16% compared with healthy individuals taking the drug at the same dose.
In patients with moderate hepatic impairment (Child-Pugh score 7 to 9) receiving etoricoxib 60 mg every other day, the mean AUC was the same as in healthy subjects receiving etoricoxib at the same dose daily. Etoricoxib 30 mg once daily has not been studied in this population.
Data from clinical and pharmacokinetic studies in patients with severe hepatic impairment (≥10 Child-Pugh points) are not available.
Kidney failure
The pharmacokinetic parameters of a single dose of etoricoxib 120 mg in patients with moderate to severe renal impairment and end-stage chronic renal failure (ESRD) on hemodialysis did not differ significantly from those in healthy individuals. Hemodialysis had little effect on excretion (dialysis clearance – about 50 ml/min).
Children
The pharmacokinetic parameters of etoricoxib have not been studied in children under 12 years of age.
In a pharmacokinetic study (n=16) conducted in adolescents aged 12 to 17 years, the pharmacokinetics in adolescents weighing from 40 to 60 kg when taking etoricoxib at a dose of 60 mg 1 time / day and in adolescents weighing more than 60 kg when taking etoricoxib at a dose of 90 mg 1 time / day were similar to the pharmacokinetics in adults when taking etoricoxib at a dose of 90 mg 1 time / day. The safety and effectiveness of etoricoxib in children has not been established.
Special instructions
Special instructions
Effect on the gastrointestinal tract
Cases of upper gastrointestinal complications (perforation, ulceration or bleeding), sometimes fatal, have been reported in patients receiving etoricoxib. It is recommended to exercise caution when treating patients at high risk of developing gastrointestinal complications when using NSAIDs, in particular in the elderly, patients who are simultaneously using other NSAIDs, incl. acetylsalicylic acid, as well as in patients with a history of gastrointestinal diseases such as ulcers or gastrointestinal bleeding.
There is an additional risk of developing gastrointestinal adverse reactions (gastrointestinal ulcers or other gastrointestinal complications) with concomitant use of etoricoxib and acetylsalicylic acid (even in low doses). In long-term clinical studies, there were no significant differences in gastrointestinal safety when using selective COX-2 inhibitors in combination with acetylsalicylic acid compared with the use of NSAIDs in combination with acetylsalicylic acid (see section “Pharmacological properties”, subsection “Pharmacodynamics”).
Effect on the cardiovascular system
The results of clinical studies indicate that the use of drugs in the class of selective COX-2 inhibitors is associated with an increased risk of thrombotic events (especially myocardial infarction and stroke) relative to placebo and some NSAIDs. Since the risk of developing cardiovascular disease when taking selective COX-2 inhibitors may increase with increasing dose and duration of use, it is necessary to choose the shortest possible duration of use and the lowest effective daily dose. It is necessary to periodically evaluate the patient’s need for symptomatic treatment and response to therapy, especially for patients with osteoarthritis (see section “Pharmacological properties”, subsection “Pharmacodynamics”, as well as sections “Contraindications”, “Dosage and Administration” and “Side Effects”).
Patients with known risk factors for the development of cardiovascular complications (such as arterial hypertension, hyperlipidemia, diabetes mellitus, smoking) should be prescribed etoricoxib only after a careful assessment of benefits and risks (see section “Pharmacological properties”, subsection “Pharmacodynamics”).
Selective COX-2 inhibitors are not a replacement for acetylsalicylic acid in the prevention of cardiovascular diseases, since they do not affect platelets. Therefore, you should not stop using antiplatelet drugs (see section “Pharmacological properties”, subsection “Pharmacodynamics”, as well as section “Interaction with other drugs”).
Effect on kidney function
Renal prostaglandins may play a compensatory role in maintaining renal perfusion. In the presence of conditions that adversely affect renal perfusion, the administration of etoricoxib may cause a decrease in prostaglandin formation and a decrease in renal blood flow, and thus reduce renal function. The greatest risk of developing this reaction is in patients with a significant decrease in renal function, decompensated heart failure, or a history of cirrhosis. In such patients, it is necessary to monitor renal function.
Fluid retention, edema and hypertension
As with other drugs that inhibit prostaglandin synthesis, fluid retention, edema, and hypertension have been reported in patients treated with etoricoxib. All NSAIDs, including etoricoxib, may be associated with the onset or recurrence of chronic heart failure. Information on the dose dependence of the effect of etoricoxib is given in the “Pharmacological properties” section, subsection “Pharmacodynamics”. Caution should be exercised when prescribing etoricoxib to patients with a history of heart failure, left ventricular dysfunction or hypertension, as well as to patients with pre-existing edema due to any other cause. If clinical signs of deterioration occur in such patients, appropriate measures should be taken, including discontinuation of etoricoxib.
The use of etoricoxib, especially at high doses, may be associated with more frequent and severe hypertension than with some other NSAIDs and selective COX-2 inhibitors. During treatment with etoricoxib, special attention should be paid to blood pressure control, which should be monitored for 2 weeks after the start of treatment and periodically thereafter. If there is a significant increase in blood pressure, alternative treatment should be considered.
Effect on liver function
In clinical studies lasting up to one year, approximately 1% of patients treated with etoricoxib at doses of 30 mg, 60 mg and 90 mg per day experienced an increase in alanine aminotransferase (ALT) and/or aspartate aminotransferase (AST) activity (approximately 3 or more times the upper limit of normal).
All patients with symptoms and/or signs of liver dysfunction, as well as patients with abnormal liver function tests, should be monitored. If persistent liver function abnormalities (three times the upper limit of normal) are detected, etoricoxib should be discontinued.
General instructions
If the patient experiences deterioration in the function of any of the organ systems listed above during treatment, appropriate measures should be taken and discontinuation of etoricoxib should be considered. When using etoricoxib in elderly patients and in patients with impaired renal, hepatic or cardiac function, appropriate medical supervision is required.
Caution should be exercised when initiating treatment with etoricoxib in patients with dehydration. Rehydration is recommended before starting etoricoxib.
During post-marketing surveillance, serious skin reactions have been reported very rarely with the use of NSAIDs and some selective COX-2 inhibitors. Some of them (including exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis) were fatal. The risk of developing such reactions is highest at the beginning of therapy, in most cases during the first month of treatment. Serious hypersensitivity reactions, such as anaphylaxis and angioedema, have been reported in patients receiving etoricoxib. The use of some selective COX-2 inhibitors has been associated with an increased risk of skin reactions in patients with a history of any drug allergies. Etoricoxib should be discontinued at the first appearance of skin rash, mucosal lesions, or any other sign of hypersensitivity.
The use of etoricoxib may mask fever or other signs of inflammation.
Caution should be exercised when concomitantly prescribing etoricoxib with warfarin or other oral anticoagulants (see section “Interactions with other drugs”).
The use of etoricoxib, like other drugs that inhibit COX and prostaglandin synthesis, is not recommended for women who are planning pregnancy (see section “Pharmacological properties”, subsection “Pharmacodynamics” and section “Use during pregnancy and breastfeeding, effects on fertility”).
Impact on the ability to drive vehicles and machinery
Patients who experience dizziness, drowsiness, or weakness while taking etoricoxib should avoid driving or operating machinery.
Active ingredient
Active ingredient
Etoricoxib
Composition
Composition
One film-coated tablet contains:
Active ingredient:
Etoricoxib 120.0 mg;
Excipients:
Core: hypromellose E15 – 4.00 mg; calcium hydrogen phosphate dihydrate – 120.00 mg; croscarmellose sodium – 8.00 mg; colloidal silicon dioxide – 2.00 mg; sodium stearyl fumarate – 6.00 mg; microcrystalline cellulose 200 – 140.00 mg.
Film coating: hypromellose E15 – 9.60 mg; copovidone (Kollidon VA64) – 1.28 mg; macrogol 6000 – 1.92 mg; red iron oxide dye – 0.32 mg; talc – 0.32 mg; titanium dioxide – 2.56 mg.
Pregnancy
Pregnancy
Pregnancy
There are no clinical data on the use of etoricoxib during pregnancy. Reproductive toxicity has been observed in animal studies. The potential risk in women during pregnancy is unknown. The use of etoricoxib, like other drugs that inhibit prostaglandin synthesis, during the last trimester of pregnancy can lead to suppression of uterine contractions and premature closure of the ductus arteriosus. Etoricoxib is contraindicated during pregnancy. If pregnancy occurs during treatment, etoricoxib should be discontinued.
Breast-feeding
In lactating rats, etoricoxib is excreted in milk. Studies have not been conducted to confirm the excretion of etoricoxib into breast milk in women. Women taking etoricoxib should stop breastfeeding (see Contraindications section).
Fertility
The use of etoricoxib, like other drugs that inhibit COX-2 and prostaglandin synthesis, is not recommended for women planning pregnancy.
Contraindications
Contraindications
· Hypersensitivity to any component of the drug;
· Peptic ulcer of the stomach and duodenum in the acute stage, active gastrointestinal bleeding;
· Complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses, and intolerance to acetylsalicylic acid or other NSAIDs (including a history).
· Pregnancy, breastfeeding period.
· Severe liver dysfunction (serum albumin <25 g/l or ≥10 points on the Child-Pugh scale);
· Severe renal failure (creatinine clearance less than 30 ml/min);
· Children under 16 years of age;
· Inflammatory bowel diseases;
· Chronic heart failure (NYHA functional class II-IV);
· Uncontrolled arterial hypertension, in which blood pressure levels persistently exceed 140/90 mmHg;
· Confirmed coronary heart disease, peripheral arterial disease and/or cerebrovascular disease;
· Lactase deficiency, lactose intolerance, glucose-galactose malabsorption;
Confirmed hyperkalemia;
· Progressive kidney diseases.
With caution
Caution should be exercised when using the drug in the following groups of patients:
– patients with an increased risk of developing gastrointestinal complications due to taking NSAIDs; elderly people simultaneously taking other NSAIDs, incl. acetylsalicylic acid, or patients with a history of gastrointestinal diseases such as peptic ulcers and gastrointestinal bleeding;
– patients with a history of risk factors for cardiovascular complications, such as dyslipidemia/hyperlipidemia, diabetes mellitus, hypertension, smoking, heart failure, left ventricular dysfunction, edema and fluid retention;
– patients with mild liver dysfunction (5-6 points on the Child-Pugh scale) should not exceed a dose of 60 mg 1 time / day, patients with moderate liver dysfunction (7-9 points on the Child-Pugh scale) – 30 mg 1 time / day;
– patients with dehydration;
– patients with impaired renal function who are simultaneously using ACE inhibitors and angiotensin II diuretics, especially the elderly;
– patients with creatinine clearance <60 ml/min;
– patients with a previous significant decrease in renal function, with weakened renal function, decompensated heart failure or cirrhosis, who are at risk with long-term use of NSAIDs.
Caution should be exercised during concomitant therapy with the following drugs:
– anticoagulants (for example, warfarin);
– antiplatelet agents (for example, acetylsalicylic acid, clopidogrel);
– drugs metabolized by sulfotransferases.
Side Effects
Side Effects
The safety of etoricoxib was assessed in clinical studies that included 9295 participants, incl. 6757 patients with OA, RA, chronic low back pain and ankylosing spondylitis (approximately 600 patients with OA or RA were treated for one year or longer).
In clinical studies, the adverse effect profile was similar in patients with OA or RA who took etoricoxib for 1 year or longer.
In a clinical trial of acute gouty arthritis, patients received etoricoxib 120 mg/day for 8 days. The adverse effect profile in this study was generally similar to that in the pooled studies of OA, RA, and chronic low back pain.
In the Cardiovascular Safety Program, which included data from three active-controlled studies, 17,412 patients with OA or RA received etoricoxib 60 mg or 90 mg for an average of 18 months (see Pharmacological Properties, Pharmacodynamics subsection).
In clinical studies of acute postoperative pain associated with dental surgery, in which 614 patients received etoricoxib 90 mg or 120 mg, the adverse effect profile was generally similar to that in the combined studies of OA, RA and chronic low back pain.
The following adverse reactions were reported at a higher frequency with the drug than with placebo in clinical studies that included patients with OA, RA, chronic low back pain or ankylosing spondylitis who received etoricoxib at a dose of 30 mg, 60 mg or 90 mg with a dose increase to the recommended dose over 12 weeks, in the MEDAL Program studies of up to 3.5 years, in short-term studies of acute pain, as well as during post-marketing use (definition of frequency recorded in the clinical trial database: very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1000 to <1/100), rare (≥1/10,000 to <1/1000), very rare (<1/10,000):
Infectious and parasitic diseases: often – alveolar osteitis; uncommon – gastroenteritis, upper respiratory tract infections, urinary tract infections.
Disorders of the blood and lymphatic system: infrequently – anemia (mainly as a result of gastrointestinal bleeding), leukopenia, thrombocytopenia.
Immune system disorders: uncommon – hypersensitivity reactions 1.3; rarely – angioedema, anaphylactic/anaphylactoid reactions, including shock 1.
Metabolic and nutritional disorders: often – swelling/fluid retention; uncommon – decreased or increased appetite, weight gain.
Mental disorders: infrequently – anxiety, depression, concentration problems, hallucinations1; rarely – confusion 1, anxiety 1.
Nervous system disorders: often – dizziness, headache; uncommon – taste disturbance, insomnia, paresthesia/hypesthesia, drowsiness.
Visual disorders: uncommon – blurred vision, conjunctivitis.
Hearing and labyrinthine disorders: uncommon – tinnitus, vertigo.
Cardiovascular system disorders: often – palpitations, arrhythmia1, arterial hypertension; uncommon – atrial fibrillation, tachycardia1, chronic heart failure, nonspecific changes on the ECG, angina1, myocardial infarction4, hot flashes, cerebrovascular accident 4, transient ischemic attack, hypertensive crisis 1, vasculitis 1.
Respiratory system disorders: often – bronchospasm1; infrequently – cough, shortness of breath, nosebleeds.
Gastrointestinal disorders: very often – abdominal pain; often – constipation, flatulence, gastritis, heartburn/gastroesophageal reflux, diarrhea, dyspepsia/epigastric discomfort, nausea, vomiting, esophagitis, ulcers of the oral mucosa; uncommon – abdominal bloating, changes in peristalsis, dry oral mucosa, gastroduodenal ulcer, stomach ulcer, including gastrointestinal perforation and bleeding, irritable bowel syndrome, pancreatitis1.
Disorders of the liver and biliary tract: often – increased ALT activity, increased AST activity; rarely – hepatitis1; rarely2 – liver failure1, jaundice1.
Disorders of the skin and subcutaneous tissues: often – ecchymosis; infrequently – swelling of the face, itching, rash, erythema1, urticaria1; rarely2 – Stevens-Johnson syndrome1, toxic epidermal necrolysis1, fixed drug-induced erythema1.
Musculoskeletal and connective tissue disorders: uncommon – muscle spasms/cramps, musculoskeletal pain/stiffness.
Renal and urinary tract disorders: uncommon – proteinuria, increased serum creatinine, renal failure1.
General disorders and disorders at the injection site: often – asthenia/weakness, flu-like syndrome; infrequently – chest pain.
Impact on the results of laboratory and instrumental studies: infrequently – increased blood urea nitrogen, increased creatine phosphokinase, hyperkalemia, increased uric acid; rarely – decreased sodium in the blood.
1 This adverse reaction was reported during post-marketing surveillance. Its reported frequency is estimated based on the highest frequency observed in clinical studies pooled by dose and indication.
2 The frequency category “rare” was determined based on the estimated upper limit of the 95% confidence interval for 0 events, considering the number of patients receiving etoricoxib in the analysis of phase III data pooled by dose and indication (n=15,470).
3 Hypersensitivity includes the terms “allergy”, “drug allergy”, “drug hypersensitivity”, “hypersensitivity”, “unspecified hypersensitivity”, “hypersensitivity reaction” and “non-specific allergy”.
4 Based on the results of an analysis of long-term placebo-controlled and active-controlled clinical studies, the use of selective COX-2 inhibitors increases the risk of developing serious arterial thrombotic events, including myocardial infarction and stroke. Based on available data, it is unlikely that the absolute risk of developing these events exceeds 1% per year (infrequent).
The following serious adverse events have been reported in association with NSAIDs and cannot be excluded for etoricoxib: nephrotoxicity, including interstitial nephritis and nephrotic syndrome.
Interaction
Interaction
Pharmacodynamic interaction
Oral anticoagulants (warfarin). In patients receiving warfarin, etoricoxib 120 mg/day was associated with an approximately 13% increase in MHO and prothrombin time. In patients receiving warfarin or similar drugs, MHO levels should be monitored when initiating therapy or changing the etoricoxib dosage regimen, especially in the first few days.
Diuretics, ACE inhibitors and angiotensin II antagonists. NSAIDs may reduce the effect of diuretics and other antihypertensive drugs. In some patients with impaired renal function (for example, patients with dehydration or elderly patients with impaired renal function), concomitant use of an ACE inhibitor or angiotensin II antagonist and drugs that inhibit cyclooxygenase may lead to a further deterioration of renal function, including the possible development of acute renal failure, which is usually reversible. The possibility of such interactions should be kept in mind in patients taking etoricoxib concomitantly with ACE inhibitors or angiotensin II antagonists. This combination should be prescribed with caution, especially in elderly patients. At the beginning of combined treatment, as well as at certain intervals in the future, fluid deficiency should be replenished and the issue of monitoring renal function should be considered.
Acetylsalicylic acid. In a study involving healthy volunteers, etoricoxib at a dose of 120 mg/day at steady state did not affect the antiplatelet activity of acetylsalicylic acid (81 mg 1 time/day). Etoricoxib can be used concomitantly with acetylsalicylic acid in low doses intended for the prevention of cardiovascular diseases. However, simultaneous administration of low doses of acetylsalicylic acid and etoricoxib may lead to an increased incidence of gastrointestinal ulcers and other complications compared to taking etoricoxib alone. The simultaneous use of etoricoxib with acetylsalicylic acid in doses exceeding those recommended for the prevention of cardiovascular complications, as well as with other NSAIDs, is not recommended.
Cyclosporine and tacrolimus. The interaction of etoricoxib with these drugs has not been studied, however, the simultaneous use of NSAIDs with cyclosporine and tacrolimus may increase the nephrotoxic effect of these drugs. Monitor renal function when etoricoxib is used concomitantly with any of these drugs.
Pharmacokinetic interaction
Effect of etoricoxib on other drugs
Lithium. NSAIDs reduce the renal excretion of lithium and, therefore, increase the concentration of lithium in the blood plasma. If necessary, frequently monitor the concentration of lithium in the blood and adjust the dose of lithium during simultaneous use with NSAIDs, as well as when NSAIDs are discontinued.
Methotrexate. Two studies examined the effects of etoricoxib at doses of 60, 90 and 120 mg once a day for 7 days in patients receiving once-weekly methotrexate at a dose of 7.5 to 20 mg for rheumatoid arthritis. Etoricoxib at doses of 60 and 90 mg had no effect on plasma concentrations and renal clearance of methotrexate. In one study, etoricoxib 120 mg had no effect on the pharmacokinetics of methotrexate. In another study, plasma methotrexate concentrations increased by 28% and renal clearance of methotrexate decreased by 13%. If etoricoxib and methotrexate are co-administered, patients should be monitored for possible toxic effects of methotrexate.
Oral contraceptives. Taking etoricoxib 60 mg for 21 days with oral contraceptives containing 35 mcg ethinyl estradiol (EE) and 0.5 to 1 mg norethindrone increased the AUC0-24h for EE by 37%. Taking etoricoxib at a dose of 120 mg with the above oral contraceptives (simultaneously or at intervals of 12 hours) increases the steady-state AUC0-24 hours for EE by 50-60%. This increase in EE concentrations should be taken into account when selecting the appropriate oral contraceptive for concomitant use with etoricoxib. This fact may lead to an increase in the incidence of adverse events associated with the use of oral contraceptives (for example, venous thromboembolism in women at risk).
Hormone replacement therapy (HRT). Administration of etoricoxib at a dose of 120 mg concomitantly with hormone replacement therapy drugs containing conjugated estrogens at a dose of 0.625 mg for 28 days increased the mean steady-state AUC0-24h of unconjugated estrone (41%), equilin (76%), and 17-P-estradiol (22%). The effects of etoricoxib doses recommended for long-term use (30, 60 and 90 mg) have not been studied. Etoricoxib at a dose of 120 mg changed the exposure (AUC0-24h) of these estrogenic components to less than half compared with monotherapy with a drug containing conjugated estrogens, when the dose of the latter was increased from 0.625 to 1.25 mg. The clinical significance of such increases is unknown. The combination of etoricoxib and a product containing higher doses of conjugated estrogens has not been studied. Increased estrogen concentrations should be taken into account when choosing a hormonal drug for postmenopausal use when administered concomitantly with etoricoxib, since increased estrogen exposure may increase the risk of HRT-related adverse events.
Prednisone/prednisolone. In drug interaction studies, etoricoxib did not have a clinically significant effect on the pharmacokinetics of prednisone/prednisolone.
Digoxin. When using etoricoxib at a dose of 120 mg 1 time / day for 10 days in healthy volunteers, there was no change in AUC0-24h at steady state or an effect on the excretion of digoxin by the kidneys. An increase in digoxin Cmax was noted (approximately 33%). This increase is usually not significant in most patients. However, when etoricoxib and digoxin are used concomitantly, patients at high risk for digoxin toxicity should be monitored.
Effect of etoricoxib on drugs metabolized by sulfotransferases. Etoricoxib is an inhibitor of human sulfotransferases (specifically SULT1E1) and may increase serum EE concentrations. Due to the fact that there is currently insufficient data on the effects of various sulfotransferases, and their clinical relevance for the use of many drugs is still being studied, it is advisable to use caution when prescribing etoricoxib concomitantly with other drugs metabolized primarily by human sulfotransferases (for example, oral salbutamol and minoxidil).
The effect of etoricoxib on drugs metabolized by isoenzymes of the cytochrome system. Based on the results of in vitro studies, etoricoxib is not expected to inhibit cytochrome P450 isoenzymes 1A2, 2C9, 2C19, 2D6, 2E1 and 3A4. In a study of healthy volunteers, daily administration of etoricoxib 120 mg had no effect on hepatic CYP3A4 activity as measured by the erythromycin breath test.
Effect of other drugs on the pharmacokinetics of etoricoxib
The main pathway of metabolism of etoricoxib depends on enzymes of the cytochrome system. The CYP3A4 isoenzyme promotes the metabolism of etoricoxib in vivo. In vitro studies suggest that the isoenzymes CYP2D6, CYP2C9, CYP1A2 and CYP2C19 can also catalyze the main metabolic pathway, but their quantitative characteristics in vivo have not been studied.
Ketoconazole. Ketoconazole is a potent inhibitor of the CYP3A4 isoenzyme. When ketoconazole was administered to healthy volunteers at a dose of 400 mg once a day for 11 days, it did not have a clinically significant effect on the pharmacokinetics of a single dose of etoricoxib 60 mg (43% increase in AUC).
Voriconazole and miconazole. Co-administration of strong CYP3A4 inhibitors (oral voriconazole or topical miconazole oral gel) and etoricoxib caused a slight increase in etoricoxib exposure, which was not considered clinically significant based on published data.
Rifampicin. The simultaneous administration of etoricoxib and rifampicin (a powerful inducer of the cytochrome system) led to a decrease in the concentration of etoricoxib in the blood plasma by 65%. This interaction may be accompanied by a relapse of symptoms when etoricoxib is co-administered with rifampicin. These data may indicate a need for dose escalation, but etoricoxib should not be used in doses higher than those recommended for each indication as the combination of rifampicin and etoricoxib at such doses has not been studied.
Antacids. Antacids do not have a clinically significant effect on the pharmacokinetics of etoricoxib.
Overdose
Overdose
In clinical studies, single doses of etoricoxib up to 500 mg or multiple doses of up to 150 mg/day for 21 days did not cause significant toxic effects. There have been reports of acute overdose with etoricoxib, but in most cases no adverse reactions were reported.
Symptoms: The most common adverse reactions were consistent with the safety profile of etoricoxib (eg, gastrointestinal disorders, cardiorenal events).
Treatment: in case of overdose, it is advisable to apply the usual supportive measures, such as removal of unabsorbed drug from the gastrointestinal tract, clinical observation and, if necessary, supportive therapy. Etoricoxib is not eliminated by hemodialysis, and the elimination of etoricoxib by peritoneal dialysis has not been studied.
Storage conditions
Storage conditions
Store in a place protected from light at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
Store in a place protected from light at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Manufacturer
Manufacturer
Pharmasintez JSC, Russia
Additional information
| Shelf life | Store in the dark place at a temperature not exceeding 25 °С. Store out of the reach of children. |
|---|---|
| Conditions of storage | Store in the dark place at a temperature not exceeding 25 °С. Store out of the reach of children. |
| Manufacturer | Pharmasintez JSC, Russia |
| Medication form | pills |
| Brand | Pharmasintez JSC |
Related products
Buy Etorelex, 120 mg 7 pcs. with delivery to USA, UK, Europe and over 120 other countries.