No products in the cart.
Esmia, tablets 5 mg, 28 pcs.
€290.00 €274.00
Description
Ulipristal is a synthetic selective progesterone receptor modulator characterized by a tissue-specific partial antiprogesterone effect, active when taken orally.
Endometrium
Ulypristal has a direct effect on the endometrium. When the drug is started daily at a dose of 5 mg during the menstrual cycle, most women (including patients with myoma) end their next menstrual bleeding and the next bleeding does not occur. When the drug is discontinued, the menstrual cycle usually resumes within 4 weeks.
Direct action on the endometrium results in endometrial changes specific to this class of drugs due to antagonistic action on progesterone receptors (Progesterone Receptor Modulator Associated Endometrial Changes (PAEC)). As a rule, histological changes are represented by inactive and weakly proliferating epithelium, accompanied by asymmetric growth of stroma and epithelium, pronounced cystic expansion of glands with mixed estrogenic (mitotic) and progestagenic (secretory) effects on epithelium. These changes were noted in about 60% of patients who received ulipristal acetate for 3 months. These changes are reversible and disappear after discontinuation of treatment and should not be mistaken for endometrial hyperplasia.
About 5% of patients of childbearing age with severe menstrual bleeding have an endometrial thickness greater than 16 mm. In 10-15% of patients receiving ulipristal acetate, the endometrium may thicken (>16 mm) during treatment. This thickening disappears when the drug is discontinued and menstrual bleeding resumes. If endometrial thickening remains for 3 months after the end of treatment and recovery of menstrual periods, further evaluation should be performed to rule out other diseases.
Leiomyoma
Ulipristal has a direct effect on leiomyomas, inhibiting cell proliferation and inducing apoptosis, which leads to a reduction in their size.
Pituitary
The daily administration of ulipristal at a dose of 5 mg suppresses ovulation in most patients, as evidenced by maintaining progesterone concentrations at about 0.3 ng/mL.
Daily administration of ulipristal at a dose of 5 mg partially reduces FSH concentrations, but serum estradiol concentrations in most patients are maintained at mid-follicular phase levels and correspond to those in the placebo group.
Ulipristal does not affect plasma thyroxine-binding globulin (TSH), ACTH and prolactin concentrations for 3 months of treatment.
Preclinical safety data
Preclinical studies of pharmacological safety, multiple dose toxicity and genotoxicity have not identified any potential threats to humans.
The main findings in general toxicity studies are related to effects on progesterone receptors (as well as on GCS receptors when the drug is used in higher concentrations), with antiprogesterone activity at exposures close to therapeutic in humans. A 39-week study in monkeys using low doses showed changes similar to RAES. Due to its mechanism of action, ulipristal causes fetal death in rats, rabbits (at multiple doses above 1 mg/kg), guinea pigs, and monkeys. The safety of the drug against the human embryo has not been established.
In doses low enough to maintain pregnancy in animals, teratogenic potential has not been identified. Reproduction studies in rats using doses that provide the same exposure as in humans found no evidence of effects on the reproductive capacity of animals receiving ulipristal or their offspring.
In studies conducted in mice and rats, no carcinogenic effects of ulipristal have been identified.
Clinical efficacy and safety
The efficacy of fixed-dose ulipristal 5 mg and 10 mg once daily was evaluated in two phase 3 studies involving patients with very severe menstrual bleeding caused by uterine myoma.
Compared with placebo, there was a clinically significant reduction in menstrual bleeding volume in patients taking ulipristal. This allowed quicker and more effective correction of anemia than when only iron preparations were prescribed. The reduction in menstrual blood loss in patients in the ulipristal group was comparable to the group receiving the GnRH agonist (leuprorelin). In most patients receiving ulipristal, bleeding stopped within the first week of use (amenorrhea developed).
In MRI data, there was a significantly greater reduction in uterine myoma size in the ulipristal group than in the placebo group. In patients who did not undergo hysterectomy or myomectomy, a decrease in uterine myoma size was assessed at ultrasound follow-up at the end of treatment (week 13). This was generally maintained through 25 weeks of follow-up in patients in the ulipristal group, whereas a slight increase in uterine myoma size was noted in the group receiving leuprorelin.
In another Phase 3 study in which patients received 2 courses of 10-mg ulipristal therapy for 3 months each, the incidence of amenorrhea was comparable at the end of both courses of therapy. The reduction in leiomyoma volume recorded during the first course was maintained during the second course. Based on previous studies, the efficacy of 5 mg in the first course would be the same in the second course, similar to the 10 mg dose.
In spite of the limited number of patients who completed four 3-month courses of therapy, the safety data are sufficient to justify one additional 3-month course of therapy in the preoperative period.
Pharmacokinetics
Absorption
After a single oral dose of 5 mg or 10 mg, ulipristal is rapidly absorbed, reaching a Cmax of 23±14.2 ng/mL approximately 1 h after ingestion.5±14.2 ng/mL and 50.0±34.4 ng/mL, respectively. The AUC0-∞ is 61.3±31.7 and 134.0±83.8 ng×h/mL, respectively. Ulipristal is rapidly converted to a pharmacologically active metabolite, with a Cmax of 9.0±4.4 ng/mL and 20.6±10.9 ng/mL 1 hour after administration and an AUC0-∞ of 26.0±12.0 and 63.6±30.1 ng×h/mL, respectively. Administration of ulipristal at a dose of 30 mg together with a high-fat breakfast resulted in a decrease in mean Cmax of approximately 45%, a prolongation of time to reach Cmax (from a median of 0.75 hours to 3 hours), and a 25% increase in AUC0-∞, compared with fasting administration. The same results were obtained for the active mono-N-demethylated metabolite. This kinetic effect of food is not considered significant for daily ulipristal tablets.
Distribution
Ulipristal is highly (>98%) bound to plasma proteins, including albumin, α-1-acid glycoprotein, high-density lipoproteins and low-density lipoproteins.
Ulipristal and its active N-demethylated metabolite penetrate into breast milk; the average AUCt ratio for milk/plasma is 0.74±0.32 for ulipristal.
Metabolism
Ulipristal acetate is rapidly converted to mono-N-demethylated and then to di-N-demethylated metabolites. In vitro data show that this process occurs in the cytochrome P450 system involving isoenzyme 3A4 (CYP3A4). Based on the fact that metabolism of ulipristal acetate is mediated by cytochrome P450, the effect of hepatic insufficiency on excretion of ulipristal acetate is expected to increase exposure. </Excretion
The main route of excretion is through the intestine, less than 10% of the substance is excreted by the kidneys. The final T1/2 of ulipristal acetate after a single dose of 5 mg or 10 mg is approximately 38 h, the average clearance is about 100 l/h.
In vitro data show that at clinically relevant concentrations, ulipristal acetate and its active metabolite do not inhibit CYP1A2, 2A6, 2C9, 2C19, 2D6, 2E1 and 3A4 isoenzymes and do not induce CYP1A2 isoenzyme. Thus, the use of ulipristal acetate should not affect the clearance of drugs that are metabolized with the participation of these isoenzymes.
In vitro data show that ulipristal acetate and its active metabolite are not substrates of P-glycoprotein (ABCB1).
Indications
Indications
Preoperative treatment of symptoms of moderate and severe uterine fibroids in adult women of reproductive age over 18 years of age (duration of therapy – no more than 2 courses).
Pharmacological effect
Pharmacological effect
Ulipristal is a synthetic selective modulator of progesterone receptors, characterized by a tissue-specific partial antiprogesterone effect, active when taken orally.
Endometrium
Ulipristal has a direct effect on the endometrium. When starting a daily dose of 5 mg of the drug during the menstrual cycle, most women (including patients with fibroids) end up with one menstrual bleeding, and the next one does not occur. When the drug is stopped, the menstrual cycle usually resumes within 4 weeks.
Direct action on the endometrium leads to class-specific changes in the endometrium associated with an antagonistic effect on progesterone receptors (Progesterone Receptor Modulator Associated Endometrial Changes (PAEC)). As a rule, histological changes are represented by an inactive and weakly proliferating epithelium, accompanied by asymmetry of growth of the stroma and epithelium, pronounced cystic expansion of the glands with mixed estrogenic (mitotic) and progestogenic (secretory) effects on the epithelium. Such changes were observed in approximately 60% of patients receiving ulipristal acetate for 3 months. These changes are reversible and disappear after cessation of treatment and should not be mistaken for endometrial hyperplasia.
In approximately 5% of patients of childbearing age with severe forms of menstrual bleeding, the thickness of the endometrium is more than 16 mm. In 10-15% of patients receiving ulipristal acetate, the endometrium may thicken (>16 mm) during treatment. This thickening disappears after stopping the drug and resuming menstrual bleeding. If endometrial thickening remains for 3 months after the end of treatment and the return of menstruation, additional examination should be performed to exclude other diseases.
Leiomyoma
Ulipristal has a direct effect on leiomyomas, suppressing cell proliferation and inducing apoptosis, which leads to a decrease in their size.
Pituitary
When taking ulipristal daily at a dose of 5 mg, ovulation is suppressed in most patients, as evidenced by maintaining progesterone concentrations at about 0.3 ng/ml.
When taking ulipristal daily at a dose of 5 mg, the concentration of FSH is partially reduced, but the concentration of estradiol in the blood serum in most patients is maintained at the level of the mid-follicular phase and corresponds to that in the placebo group.
Ulipristal does not affect the concentration of thyroxine-binding globulin (TBG), ACTH and prolactin in the blood plasma during 3 months of treatment.
Preclinical safety data
Preclinical studies of pharmacological safety, repeated dose toxicity and genotoxicity have not identified potential threats to humans.
The main findings in studies of general toxicity are associated with the effect on progesterone receptors (as well as on GCS receptors when using the drug in higher concentrations), with antiprogesterone activity at exposures close to therapeutic in humans. A 39-week low-dose study in monkeys showed changes similar to RAEC. Due to its mechanism of action, ulipristal causes fetal death in rats, rabbits (at repeated doses above 1 mg/kg), guinea pigs and monkeys. The safety of the drug in relation to the human embryo has not been established.
At doses small enough to maintain pregnancy in animals, no teratogenic potential has been identified. Reproduction studies in rats using doses equivalent to human exposures showed no evidence of effects on the reproductive capacity of animals treated with ulipristal or their offspring.
In studies conducted on mice and rats, the carcinogenic effect of ulipristal was not revealed.
Clinical efficacy and safety
The effectiveness of fixed doses of ulipristal 5 mg and 10 mg once daily was evaluated in two phase 3 studies in patients with very heavy menstrual bleeding caused by uterine fibroids.
Compared with placebo, a clinically significant reduction in the volume of menstrual blood loss was detected in patients taking ulipristal. This made it possible to quickly and more effectively correct anemia than when prescribing iron supplements alone. The reduction in menstrual blood loss in patients in the ulipristal group was comparable to the group receiving the GnRH agonist (leuprorelin). In most patients receiving ulipristal, bleeding stopped during the first week of treatment (amenorrhea developed).
According to MRI, there was a significantly greater reduction in uterine fibroid size in the ulipristal group than in the placebo group. In patients who did not undergo hysterectomy or myomectomy, a decrease in the size of uterine fibroids was assessed by ultrasound control at the end of treatment (week 13). As a rule, it persisted throughout the 25-week follow-up in patients in the ulipristal group, while in the group receiving leuprorelin there was a slight increase in the size of uterine fibroids.
In another Phase 3 study, in which patients received 2 courses of ulipristal 10 mg for 3 months, the incidence of amenorrhea was comparable at the end of both courses of therapy. The reduction in leiomyoma volume recorded during the first course was maintained during the second course. Taking into account the results of previous studies, the effectiveness of the drug at a dose of 5 mg during the first course of therapy will be the same during the second course of therapy, similar to a dose of 10 mg.
Despite the limited number of patients completing four 3-month courses of treatment, the safety data obtained were sufficient to justify one additional 3-month course of therapy in the preoperative period.
Pharmacokinetics
Suction
After a single oral dose of 5 mg or 10 mg, ulipristal is rapidly absorbed, reaching Cmax of 23.5 ± 14.2 ng/ml and 50.0 ± 34.4 ng/ml, respectively, approximately 1 hour after administration. AUC0-∞ is 61.3±31.7 and 134.0±83.8 ng×h/ml, respectively. Ulipristal is quickly transformed into a pharmacologically active metabolite, and 1 hour after administration, Cmax is 9.0±4.4 ng/ml and 20.6±10.9 ng/ml, AUC0-∞ – 26.0±12.0 and 63.6±30.1 ng×h/ml, respectively. Taking ulipristal 30 mg with a high-fat breakfast resulted in an approximately 45% decrease in mean Cmax, a prolongation of time to Cmax (from a median of 0.75 hours to 3 hours) and a 25% increase in AUC0-∞, compared with administration on an empty stomach. The same results were obtained for the active mono-N-demethylated metabolite. This kinetic effect of food is not considered significant for daily use of ulipristal tablets.
Distribution
Ulipristal is highly (>98%) bound to plasma proteins, including albumin, α-1-acid glycoprotein, high-density lipoprotein and low-density lipoprotein.
Ulipristal and its active N-demethylated metabolite are excreted in breast milk; The average AUCt ratio for milk/plasma is 0.74±0.32 for ulipristal.
Metabolism
Ulipristal acetate is rapidly converted to mono-N-demethylated and then di-N-demethylated metabolites. In vitro data indicate that this process occurs in the cytochrome P450 system involving isoenzyme 3A4 (CYP3A4). Based on the fact that the metabolism of ulipristal acetate is mediated by cytochrome P450, the effect of hepatic impairment on the elimination of ulipristal acetate is expected to increase its exposure.
Removal
The main route of elimination is through the intestines, less than 10% of the substance is excreted by the kidneys. The final T1/2 of ulipristal acetate after a single dose of 5 mg or 10 mg is approximately 38 hours, the average clearance is about 100 l/h.
In vitro data show that at clinically relevant concentrations of ulipristal acetate and its active metabolite do not inhibit the isoenzymes CYP1A2, 2A6, 2C9, 2C19, 2D6, 2E1 and 3A4 and do not induce the CYP1A2 isoenzyme. Thus, the use of ulipristal acetate should not affect the clearance of drugs that are metabolized with the participation of these isoenzymes.
In vitro data indicate that ulipristal acetate and its active metabolite are not substrates of P-glycoprotein (ABCB1).
Special instructions
Special instructions
Ulipristal acetate is prescribed only after a thorough examination. Before starting treatment, pregnancy should be excluded.
Contraception
Due to the possibility of undesirable interactions, the concomitant use of only gestagen-containing drugs, gestagen-releasing systems or combined oral contraceptives is not recommended. Although anovulation was observed in the majority of women receiving therapeutic doses of ulipristal, additional use of a non-hormonal method of contraception during treatment is recommended.
Kidney failure
There is no reason to believe that renal failure may significantly affect the elimination of ulipristal. It is not recommended to use ulipristal acetate without constant monitoring in patients with severe renal failure, since special studies have not been conducted.
Liver failure
There is no experience with the therapeutic use of ulipristal acetate in patients with liver failure. It is expected that hepatic impairment may interfere with the elimination of ulipristal acetate, resulting in increased drug exposure. This is not significant for patients with mild liver failure. It is not recommended to prescribe ulipristal acetate to patients with moderate or severe hepatic impairment unless constant monitoring is possible.
Concomitant therapy
Concomitant use of ulipristal and moderate-potent CYP3A4 inhibitors (eg, erythromycin, grapefruit juice, verapamil) or potent inhibitors (eg, ketoconazole, ritonavir, nefazodone, itraconazole, telithromycin, clarithromycin) is not recommended.
The combined use of ulipristal and strong inducers of CYP3A4 (for example, rifampicin, rifabutin, carbamazepine, oxcarbazepine, phenytoin, fosphenytoin, phenobarbital, primidone, St. John’s wort, efavirenz, nevirapine, ritonavir – during long-term use) is not recommended.
Endometrial changes
Ulipristal acetate has a specific pharmacodynamic effect on the endometrium. There may be an increase in endometrial thickness. If endometrial thickening persists for 3 months after the end of treatment and the resumption of menstruation, additional examination should be performed to exclude other diseases.
In patients receiving ulipristal, histological examination may show changes in the structure of the endometrium. Such changes are reversible after completion of treatment. These histological changes are referred to as progesterone receptor antagonist-associated endometrial changes (PAEC) and should not be misdiagnosed as endometrial hyperplasia. It is recommended to carry out no more than two courses of therapy. The duration of each course should not exceed 3 months, since the risk of undesirable effects on the endometrium during longer therapy is unknown.
Bleeding
Patients should be informed that treatment with ulipristal acetate usually results in a significant reduction in menstrual blood loss or amenorrhea within the first 10 days of treatment. If excessive bleeding continues, the patient should consult a doctor. As a rule, the menstrual cycle resumes within 4 weeks after the end of treatment.
Fertility
The majority of women taking ulipristal acetate in therapeutic doses experienced anovulation. However, fertility with long-term use of ulipristal acetate has not been studied.
Impact on the ability to drive vehicles and operate machinery
Ulipristal may have a minimal effect on the ability to drive vehicles and machinery, because Mild dizziness may occur after taking ulipristal.
Active ingredient
Active ingredient
Ulipristal
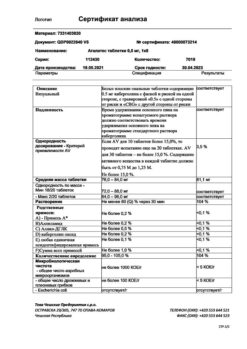
Composition
Composition
1 tablet contains:
active ingredient:
ulipristal acetate 5 mg,
excipients:
microcrystalline cellulose – 93.5 mg,
mannitol – 43.5 mg, talc – 4 mg,
croscarmellose sodium – 2.5 mg,
magnesium stearate – 1.5 mg.
Pregnancy
Pregnancy
Ulipristal acetate is contraindicated during pregnancy. There are no or limited data on the use of ulipristal acetate in pregnant women. Although animal studies have not demonstrated teratogenic potential, data regarding reproductive toxicity are insufficient.
Animal studies have shown that ulipristal acetate is excreted in breast milk. It is not known whether ulipristal acetate is excreted in human breast milk, so a risk to infants during breastfeeding cannot be excluded. Ulipristal acetate is contraindicated during breastfeeding.
Contraindications
Contraindications
hypersensitivity to ulipristal acetate or any of the excipients of Esmya;
bleeding from the vagina of unknown etiology or for reasons not related to uterine fibroids;
cancer of the uterus, cervix, ovary or breast;
duration of therapy over 3 months (due to the lack of safety data for longer use);
bronchial asthma, severe form, not amenable to correction with oral corticosteroids;
pregnancy;
lactation period;
age up to 18 years.
The drug should be prescribed with caution in case of renal and/or liver failure, bronchial asthma.
Side Effects
Side Effects
The safety of ulipristal acetate was assessed in 393 women with uterine fibroids who received 5 mg or 10 mg ulipristal acetate in phase III studies. The most common observed event in clinical trials was amenorrhea (82.2%), which is considered a desirable outcome.
The most common adverse reaction was hot flashes. The vast majority of adverse reactions were mild or moderate (94.9%), did not lead to discontinuation of drug treatment (99.3%) and resolved independently.
In two phase III studies in patients with uterine fibroids receiving the drug for 3 months, the following adverse reactions were reported. Adverse adverse reactions are presented by systemic and organ classes in accordance with the MedDRA classification and with the frequency of occurrence: very often (≥1/10); often (from ≥1/100 to
Within each frequency group, adverse reactions are presented in descending order of severity.
From the mental side: often – emotional disorders; infrequently – anxiety.
From the nervous system: often – headache* (* – see Description of individual adverse reactions); infrequently – dizziness.
From the side of metabolism: infrequently – weight gain.
On the part of the organ of hearing and balance: often – vertigo.
From the respiratory system: infrequently – nosebleeds.
From the digestive system: often – abdominal pain, nausea; uncommon – dyspepsia, dry mouth, flatulence, constipation.
From the skin and subcutaneous tissue: often – acne, increased sweating; infrequently – skin lesions.
From the musculoskeletal system: often – pain in bones and muscles; infrequently – back pain.
From the urinary system: infrequently – urinary incontinence.
From the reproductive system and mammary glands: very often – amenorrhea, thickening of the endometrium*, hot flashes*; often – metrorrhagia*, ovarian cyst*, breast tenderness/tenderness, pelvic pain; infrequently – rupture of an ovarian cyst, vaginal discharge, enlargement and discomfort in the mammary glands.
From the body as a whole: often – swelling, increased fatigue; infrequently – asthenia.
From laboratory parameters: often – increased concentration of cholesterol in the blood; infrequently – increased concentration of triglycerides in the blood.
Description of selected adverse reactions
Thickening of the endometrium
In 10-15% of patients receiving ulipristal acetate, thickening of the endometrium (>16 mm according to ultrasound or MRI at the end of treatment) may occur. This phenomenon is reversible after cessation of treatment and resumption of the menstrual cycle.
In addition, reversible changes in the endometrium, referred to as PAEC, are distinguished from endometrial hyperplasia. The pathologist should be informed that the patient is taking ulipristal acetate when conducting histological examination for hysterectomy or endometrial biopsy.
Tides
Hot flashes were reported in 12.7% of patients, but their frequency varied between studies. In the active control study, the incidence was 24% (10.5% moderate or severe) for the ulipristal acetate group and 60.4% (39.6% moderate or severe) for the leuprorelin group. In a placebo-controlled study, the incidence of hot flashes was 1.0% for ulipristal acetate and 0% for placebo.
Headache
Mild or moderate headache was observed in 6.4% of patients.
Ovarian cyst
In 1.5% of patients, functional ovarian cysts were discovered during treatment, which spontaneously disappeared within a few weeks.
Uterine bleeding
Patients with heavy menstrual bleeding due to uterine leiomyomas are at risk for increased blood loss, which may require surgery. There were several such reports, both during therapy and 2-3 months after the end of treatment with ulipristal acetate.
Interaction
Interaction
Possible influence of other drugs on the effect of ulipristal acetate
Hormonal contraceptives
Ulipristal acetate has a steroidal structure and acts as a selective progesterone receptor modulator with a predominant inhibitory effect on progesterone receptors. Thus, hormonal contraceptives and progestins may reduce the effectiveness of ulipristal acetate by competitively acting on the progesterone receptor. Therefore, the simultaneous use of drugs containing gestagens is not recommended.
CYP3A4 isoenzyme inhibitors
After the use of a moderate-potency inhibitor of the CYP3A4 isoenzyme – erythromycin propionate (500 mg 2 times / day for 9 days) in healthy female volunteers, the Cmax and AUC of ulipristal increased by 1.2 and 2.9 times, respectively; the AUC value of the active metabolite of ulipristal acetate increased by 1.5 times, while the Cmax of the active metabolite decreased (0.52 times). During the use of ketoconazole (400 mg 1 time/day, 7 days), a powerful inhibitor of CYP3A4, healthy female volunteers showed an increase in Cmax and AUC of ulipristal by 2 and 5.9 times, respectively.
There was an increase in AUC values for the active metabolite of ulipristal by 2.4 times with a decrease in its Cmax (a change of 0.53 times). No dose adjustment is required when using ulipristal in patients receiving weak inhibitors of the CYP3A4 isoenzyme. Concomitant use of moderate-potency inhibitors or strong inhibitors of the CYP3A4 isoenzyme with ulipristal is not recommended.
Inducers of the isoenzyme CYP3A4
During the use of the powerful CYP3A4 inducer rifampicin (300 mg 2 times / day, 9 days), healthy female volunteers showed a pronounced decrease in the Cmax and AUC of ulipristal and its active metabolite by more than 90%. A 2.2-fold decrease in T1/2 of ulipristal was also noted, which corresponds to a decrease in its exposure by approximately 10 times. Concomitant use of ulipristal and strong CYP3A4 inducers (for example, rifampicin, rifabutin, carbamazepine, oxcarbazepine, phenytoin, fosphenytoin, phenobarbital, primidone, St. John’s wort, efavirenz, nevirapine, ritonavir – during long-term use) is not recommended.
Drugs that affect gastric pH
The use of ulipristal (10 mg/day) together with the proton pump inhibitor esomeprazole (20 mg 1 time/day for 6 days) leads to a decrease in mean Cmax by 65%, an extension of Tmax (from a median of 0.75 hours to 1.0 hours) and an increase in mean AUC by 13%. This effect of drugs that increase gastric pH is not considered clinically significant for daily use of ulipristal acetate tablets.
Possible effect of ulipristal acetate on the action of other drugs
Hormonal contraceptives
Ulipristal may interfere with the action of hormonal contraceptives (gestagen-containing tablets only, progestogen-releasing systems or combined oral contraceptives) and progestin preparations used for other indications. Therefore, the concomitant use of drugs containing gestagen is not recommended. Progestin-containing drugs should not be used within 12 days after stopping treatment with ulipristal.
P-glycoprotein substrates
In vitro data indicate that, at clinically relevant concentrations, ulipristal acetate may act as an inhibitor of P-glycoprotein (P-gp) when absorbed into the gastrointestinal wall. Concomitant use of ulipristal and a P-gp substrate has not been studied and the possibility of interactions cannot be ruled out. In vivo data indicate that administration of ulipristal (10 mg tablet) 1.5 hours before administration of the P-gp substrate fexofenadine (60 mg) does not have a clinically significant effect on the pharmacokinetics of fexofenadine. Therefore, it is recommended to maintain an interval of at least 1.5 hours between taking ulipristal and P-gp substrates (for example, dabigatran etexilate, digoxin, fexofenadine). The patient should tell her doctor about all medications she is taking, even if they are over-the-counter.
Overdose
Overdose
Data on overdose of ulipristal acetate are limited.
Single doses of up to 200 mg and daily doses of 50 mg for 10 days have been administered to a limited number of volunteers with no severe or serious adverse reactions observed.
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 30 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Gedeon Richter, Hungary
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a light-protected place, at a temperature not exceeding 30 °C |
| Manufacturer | Gedeon Richter, Hungary |
| Medication form | pills |
| Brand | Gedeon Richter |
Related products
Buy Esmia, tablets 5 mg, 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.