No products in the cart.
Enap, tablets 5 mg 60 pcs
€4.45 €3.96
Description
An antihypertensive drug, ACE inhibitor. The mechanism of action is associated with inhibition of ACE activity, which leads to reduction of angiotensin II formation.
Enalapril is a derivative of two amino acids: L-alanine and L-proline. After absorption, enalapril taken orally is hydrolyzed to enalarylate, which inhibits ACE. Its mechanism of action is related to the reduction of angiotensin I angiotensin II formation, the decrease of which in plasma leads to the increase of plasma renin activity (due to the elimination of negative feedback on renin production) and to the decrease of aldosterone secretion. Since ACE is identical with the enzyme kininase II, enalapril can also block the degradation of bradykinin, a peptide with a powerful vasopressor effect. The significance of this effect in the mechanism of action of enalapril has not been definitively established.
The antihypertensive effect of enalapril is primarily associated with inhibition of RAAS activity, which plays an important role in BP regulation. Despite this fact, enalapril has antihypertensive effect even in patients with arterial hypertension and low concentration of renin.
Enalapril decreases BP regardless of body position (both lying and standing) without a significant increase in HR. Symptomatic orthostatic hypotension is rare. In some patients, it may take several weeks of therapy to achieve optimal BP reduction. Abrupt withdrawal of enalapril has not been accompanied by a rise in BP.
Effective inhibition of ACE activity usually occurs 2-4 hours after a single oral administration of enalapril. Time of onset of antihypertensive action when taken orally is usually 1 h and reaches a maximum of 4-6 h. Duration of action depends on the dose. When used in recommended doses, the antihypertensive effect and hemodynamic effects are maintained for at least 24 h.
In patients with essential hypertension, a decrease in BP is accompanied by a decrease in PPS and an increase in cardiac output, while HR does not change or changes insignificantly. Renal blood flow increases, but glomerular filtration rate does not change. However, in patients with a baseline low glomerular filtration rate, it usually increased.
In patients with diabetic/nondiabetic nephropathy, albuminuria/proteinuria and renal IgG excretion decreased with enalapril.
In patients with chronic heart failure (CHF) on therapy with cardiac glycosides and diuretics
administration of enalapril is accompanied by a decrease in PPS and BP, an increase in cardiac output, with a decrease in HR (usually in patients with chronic heart failure HR is increased). Pulmonary capillary congestion pressure also decreases. With long-term use, enalapril increases exercise tolerance and reduces the severity of heart failure (evaluated according to NYHA criteria). Enalapril in patients with mild to moderate heart failure slows its progression and also slows down the development of left ventricular dilatation. At left ventricular dysfunction enalapril decreases risk of development of major ischemic outcomes (including frequency of myocardial infarction and number of hospitalizations for unstable angina).
Indications
Indications
— essential hypertension;
— chronic heart failure (as part of combination therapy);
– prevention of the development of clinically significant heart failure in patients with asymptomatic left ventricular dysfunction (as part of combination therapy);
— prevention of coronary ischemia in patients with left ventricular dysfunction in order to reduce the incidence of myocardial infarction and reduce the frequency of hospitalizations for unstable angina.
Pharmacological effect
Pharmacological effect
Antihypertensive drug, ACE inhibitor. The mechanism of action is associated with inhibition of ACE activity, which leads to a decrease in the formation of angiotensin II.
Enalapril is a derivative of two amino acids: L-alanine and L-proline. After absorption, enalapril taken orally is hydrolyzed to enalalrylate, which inhibits ACE. The mechanism of its action is associated with a decrease in the formation of angiotensin II from angiotensin I, a decrease in the content of which in the plasma blood leads to an increase in the activity of plasma renin (by eliminating the negative feedback to changes in renin production) and a decrease in aldosterone secretion. Since ACE is identical to the enzyme kininase II, enalapril can also block the destruction of bradykinin, a peptide that has a powerful vasopressor effect. The significance of this effect in the mechanism of action of enalapril has not been definitively established.
The antihypertensive effect of enalapril is associated primarily with the suppression of the activity of the RAAS, which plays an important role in the regulation of blood pressure. Despite this, enalapril has an antihypertensive effect even in patients with arterial hypertension and low renin concentrations.
With the use of enalapril, blood pressure levels decrease regardless of body position (both in a supine and standing position) without a significant increase in heart rate. Symptomatic orthostatic hypotension is rare. In some patients, achieving optimal blood pressure reduction may require several weeks of therapy. Abrupt withdrawal of enalapril was not accompanied by an increase in blood pressure.
Effective inhibition of ACE activity usually occurs 2-4 hours after a single oral dose of enalapril. The onset of antihypertensive action when taken orally is usually 1 hour, reaching a maximum after 4-6 hours. The duration of action depends on the dose. When used in recommended doses, the antihypertensive effect and hemodynamic effects are maintained for at least 24 hours.
In patients with essential hypertension, a decrease in blood pressure is accompanied by a decrease in peripheral vascular resistance and an increase in heart rate
ejection, while the heart rate does not change or changes slightly. Renal blood flow increases, but the speed
glomerular filtration rate does not change. However, in patients with an initially low glomerular filtration rate, its level usually increased.
In patients with diabetic/nondiabetic nephropathy, albuminuria/proteinuria and renal excretion of IgG decreased while taking enalapril.
In patients with chronic heart failure (CHF) during therapy with cardiac glycosides and diuretics
the use of enalapril is accompanied by a decrease in peripheral vascular resistance and blood pressure, an increase in cardiac output, while the heart rate decreases (usually in patients with chronic heart failure, the heart rate is increased). The pulmonary capillary wedge pressure is also reduced. With long-term use, enalapril increases exercise tolerance and reduces the severity of heart failure (assessed by NYHA criteria). Enalapril in patients with mild to moderate heart failure slows down its progression, and also slows down the development of left ventricular dilatation. In case of left ventricular dysfunction, enalapril reduces the risk of major ischemic outcomes (including the incidence of myocardial infarction and the number of hospitalizations for unstable angina).
Special instructions
Special instructions
Arterial hypotension
Symptomatic hypotension rarely occurs in patients with uncomplicated hypertension. Arterial hypotension with all clinical manifestations can be observed after the first dose of Enap® in patients with hypovolemia, as a result of diuretic therapy, a salt-free diet, diarrhea, vomiting or hemodialysis. The development of symptomatic hypotension is more likely in patients with severe heart failure due to the use of high doses of diuretics, hyponatremia or impaired renal function. In such patients, treatment should begin under the supervision of a physician until the optimal dose adjustment of Enap® and/or diuretic. Similar tactics can be applied to patients with coronary artery disease or cerebrovascular diseases, in whom a sharp excessive decrease in blood pressure can lead to the development of myocardial infarction or cerebrovascular accident.
If severe arterial hypotension develops, it is necessary to transfer the patient to a horizontal position with a low head and, if necessary, administer a 0.9% sodium chloride solution intravenously.
Transient arterial hypotension is not a contraindication for further treatment with Enap®. After stabilization of blood pressure and blood volume, therapy can be continued.
In some patients with heart failure and normal or low blood pressure, it may be further reduced when taking Enap®. This effect is predictable and is not a reason to discontinue therapy. If arterial hypotension is accompanied by clinical symptoms, the dose should be reduced and/or discontinued the diuretic and/or Enap®.
Aortic or mitral stenosis, HOCM
Like all vasodilators, ACE inhibitors should be used with caution in patients with valvular obstruction and left ventricular outflow tract hypertrophy. Should not be used in patients with cardiogenic shock and hemodynamically significant left ventricular obstruction.
Renal dysfunction
In patients with renal insufficiency (CC® should be selected, first of all, taking into account CC and, then, the clinical response to treatment. In such patients, potassium levels and serum creatinine concentrations should be regularly monitored.
In patients with severe heart failure and kidney disease, including renal artery stenosis, renal failure may develop when treated with Enap®. The changes were usually reversible after discontinuation of the drug Enap®.
In some patients with arterial hypertension who did not have renal disease before treatment, there was a slight and transient increase in serum urea and creatinine concentrations when using Enap®. In such cases, it may be necessary to reduce the dose of Enap® and/or discontinue the diuretic. This situation indicates the possibility of hidden renal artery stenosis.
Renovascular hypertension
In patients with bilateral renal artery stenosis or arterial stenosis of a single functioning kidney, when treated with ACE inhibitors, the risk of developing arterial hypotension and renal failure is increased. Only slight changes in serum creatinine concentration may indicate a decrease in renal function. In such patients, treatment should be started with small doses under close medical supervision. The dose should be titrated carefully and renal function monitored.
Kidney transplant
There is no experience with the use of Enap® in patients who have recently undergone kidney transplantation. Therefore, treatment of such patients with Enap® is not recommended.
Liver dysfunction
In rare cases, therapy with ACE inhibitors was accompanied by the development of a syndrome starting with cholestatic jaundice and hepatitis up to the development of fulminant liver necrosis. The mechanism of development of this syndrome is unknown. If jaundice appears or a significant increase in liver enzyme activity, treatment with the ACE inhibitor should be stopped immediately, the patient’s condition should be carefully monitored and, if necessary, treatment should be administered.
Neutropenia/agranulocytosis
Cases of neutropenia/agranulocytosis, thrombocytopenia and anemia have been described in patients using ACE inhibitors. In patients with normal renal function in the absence of other complications, neutropenia rarely develops. The drug Enap® should be used with great caution in patients with connective tissue diseases (including systemic lupus erythematosus, scleroderma) who are simultaneously receiving immunosuppressive therapy, allopurinol or procainamide, as well as a combination of these factors, especially with existing renal dysfunction. These patients may develop severe infections that do not respond to intensive antibiotic therapy. If patients still take Enap®, it is recommended to periodically monitor the number of leukocytes in the blood. The patient should be warned that if any signs of infection appear, they should consult a doctor immediately.
Hypersensitivity/angioedema
In patients receiving ACE inhibitors, including Enap®, there have been reports of the development of angioedema of the face, extremities, lips, vocal folds and/or larynx at any time after the start of treatment. You should immediately discontinue Enap® and monitor the patient until symptoms disappear completely. Even in the case of tongue swelling, when there is only difficulty swallowing without respiratory distress, patients may require long-term observation, because the use of antihistamines and corticosteroids may be insufficient.
Angioedema of the larynx or tongue can be fatal in very rare cases. Swelling of the tongue, vocal folds, or larynx can lead to airway obstruction, especially after a history of airway surgery. If there is swelling of the tongue, vocal folds or larynx, appropriate therapy is indicated, which may include: subcutaneous administration of a 0.1% solution of epinephrine (adrenaline) (0.3 ml-0.5 ml) and/or measures aimed at restoring airway patency (intubation or tracheostomy).
Among black patients receiving ACE inhibitor therapy, the incidence of angioedema is higher than among patients of other races.
Patients with a history of angioedema not associated with ACE inhibitors are at increased risk of developing angioedema when using any ACE inhibitor.
Anaphylactoid reactions during desensitization with Hymenoptera (Hymenoptera) venom
Patients taking ACE inhibitors during hymenoptera venom desensitization have rarely developed life-threatening anaphylactoid reactions. To prevent such reactions, it is necessary to temporarily stop taking the ACE inhibitor during desensitization procedures.
Anaphylactoid reactions during LDL apheresis
Life-threatening anaphylactoid reactions have occurred in rare cases in patients receiving ACE inhibitors during LDL apheresis with dextran sulfate. The drug should be temporarily replaced with drugs from another group.
Hemodialysis
Due to the increased risk of anaphylactoid reactions, the drug should not be used in patients undergoing hemodialysis using high-flow polyacrylonitrile membranes (AN69®). If hemodialysis is necessary, it is advisable to use dialysis membranes of a different type or antihypertensive drugs of a different group.
Hypoglycemia
In patients with diabetes mellitus receiving oral hypoglycemic agents or insulin, blood glucose concentrations should be carefully monitored during the first month of treatment with an ACE inhibitor.
Cough
When using the drug Enap®, a dry, unproductive, prolonged cough may occur, which disappears after stopping the use of ACE inhibitors, which must be taken into account in the differential diagnosis of cough during the use of an ACE inhibitor.
Surgery/general anesthesia
Before surgery (including dental procedures), you must warn the surgeon/anesthesiologist about the use of Enap®. During major surgery or general anesthesia with the use of drugs that cause arterial hypotension, ACE inhibitors may block the formation of angiotensin II in response to compensatory release of renin. If a pronounced decrease in blood pressure develops, explained by a similar mechanism, it can be corrected by introducing plasma substitutes.
Hyperkalemia
May develop during treatment with ACE inhibitors, incl. drug Enap®. Risk factors for the development of hyperkalemia are renal failure, old age (over 70 years), diabetes mellitus, some concomitant conditions (decrease in blood volume, acute heart failure in the stage of decompensation, metabolic acidosis), simultaneous use of potassium-sparing diuretics (spironolactone, eplerenone, triamterene, amiloride), as well as potassium or potassium-containing drugs substitutes and the use of other drugs that help increase potassium levels in the blood plasma (for example, heparin).
The use of potassium supplements, potassium-sparing diuretics and table salt substitutes containing potassium can lead to a significant increase in serum potassium levels, especially in patients with impaired renal function. Hyperkalemia can cause serious heart rhythm problems, sometimes fatal. The simultaneous use of the above drugs should be carried out with caution under the control of potassium levels in the blood serum.
Lithium
The simultaneous use of lithium salts and Enap® is not recommended.
Ethnic characteristics
The drug Enap®, like other ACE inhibitors, has a less pronounced antihypertensive effect in patients of the Negroid race compared to representatives of other races.
Special information on excipients
The drug Enap® contains lactose, therefore the drug is contraindicated in patients with lactase deficiency, lactose intolerance, and glucose-galactose malabsorption syndrome.
Impact on the ability to drive vehicles and operate machinery
When using the drug Enap®, you must be careful when driving vehicles and performing other potentially dangerous types of work that require increased concentration and speed of psychomotor reactions (dizziness may develop due to a sharp decrease in blood pressure, especially after taking the initial dose of the drug Enap® in patients taking diuretics).
Active ingredient
Active ingredient
Enalapril
Composition
Composition
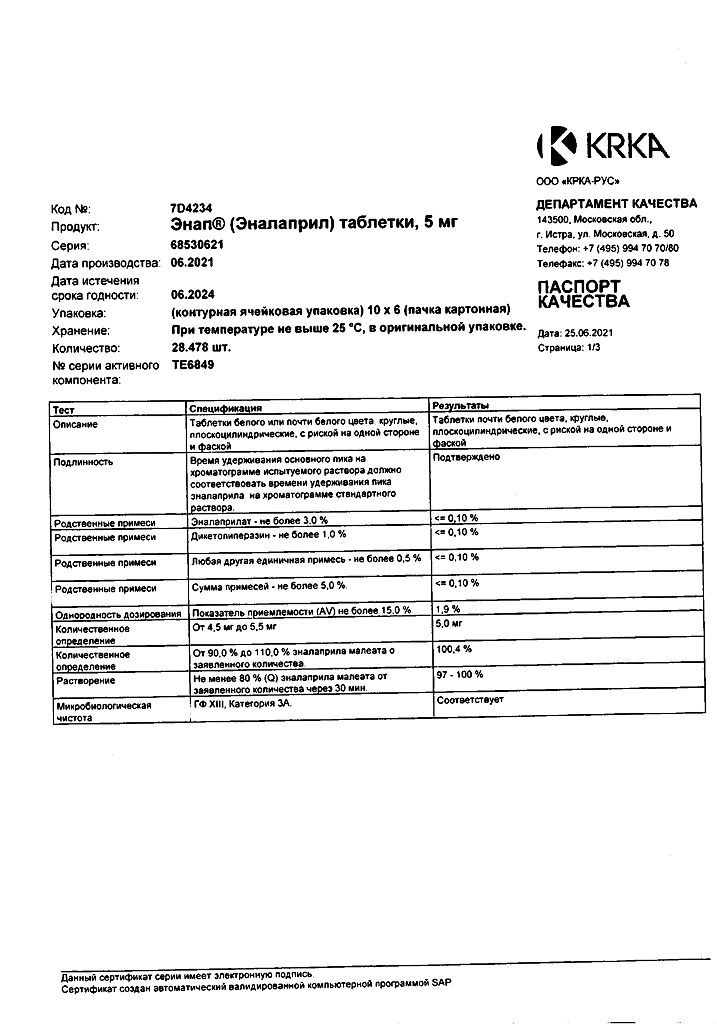
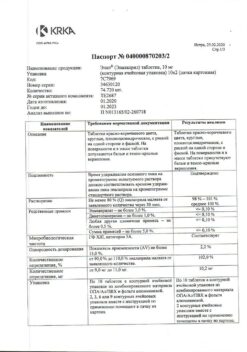
1 tab. enalapril maleate 5 mg
Excipients: sodium bicarbonate – 2.6 mg, lactose monohydrate – 129.8 mg, corn starch – 22.4 mg, hyprolose – 2.5 mg, talc – 6 mg, magnesium stearate – 1.7 mg.
Contraindications
Contraindications
– history of angioedema associated with the use of ACE inhibitors;
– hereditary angioedema or idiopathic angioedema;
– simultaneous use with aliskiren in patients with diabetes mellitus or impaired renal function (CR
– porphyria;
– pregnancy;
– lactation period (breastfeeding);
– age under 18 years (efficacy and safety have not been established);
– lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome;
– hypersensitivity to enalapril and other components of the drug;
– increased sensitivity to other ACE inhibitors.
The drug should be used with caution in patients with bilateral renal artery stenosis or stenosis of the artery of a single kidney; with primary hyperaldosteronism; hyperkalemia; after kidney transplantation; with aortic stenosis and/or mitral stenosis (with hemodynamic disorders); hypertrophic obstructive cardiomyopathy (HOCM); with reduced blood volume (including with diarrhea, vomiting); with systemic connective tissue diseases (including scleroderma, systemic lupus erythematosus); IHD; with inhibition of bone marrow hematopoiesis; cerebrovascular diseases (including cerebrovascular insufficiency); with diabetes; renal failure (proteinuria – more than 1 g/day); liver failure; in patients on a salt-restricted diet or on hemodialysis; simultaneously with immunosuppressants and diuretics; in elderly patients (over 65 years old).
Side Effects
Side Effects
Classification of the frequency of side effects (WHO): very often (≥1/10), often (≥1/100 and
From the hematopoietic system: infrequently – anemia (including aplastic and hemolytic), rarely – neutropenia, decreased hemoglobin and hematocrit, thrombocytopenia, agranulocytosis, inhibition of bone marrow hematopoiesis, pancytopenia, lymphadenopathy, autoimmune diseases.
From the side of metabolism: infrequently – hypoglycemia.
From the nervous system: very often – dizziness; often – headache, depression; infrequently – confusion, insomnia, drowsiness, paresthesia, increased excitability, vertigo; rarely – changes in the nature of dreams, sleep disturbances.
From the senses: often – a change in taste perception; infrequently – tinnitus; very rarely – blurred vision.
From the cardiovascular system: often – marked decrease in blood pressure (including orthostatic hypotension), syncope, chest pain, cardiac arrhythmias, angina pectoris; uncommon – palpitations, myocardial infarction or stroke (due to a sharp decrease in blood pressure in high-risk patients); rarely – Raynaud’s syndrome.
From the respiratory system: very often – cough; uncommon – rhinorrhea, sore throat and hoarseness, bronchospasm/bronchial asthma; rarely – shortness of breath, pulmonary infiltrates, rhinitis, allergic alveolitis/eosinophilic pneumonia.
From the digestive system: very often – nausea; often – diarrhea, abdominal pain, flatulence; uncommon – ileitis, intestinal obstruction, pancreatitis, vomiting, constipation, anorexia, dry oral mucosa, peptic ulcer; rarely – impaired liver function and bile secretion, hepatitis (hepatocellular or cholestatic), including liver necrosis, cholestatic jaundice, stomatitis/aphthous ulcers, glossitis; very rarely – angioedema of the intestine.
From the skin: often – skin rash; uncommon – increased sweating, itching, alopecia; rarely – erythema multiforme, Stevens-Johnson syndrome, exfoliative dermatitis, toxic epidermal necrolysis, pemphigus, erythroderma.
A symptom complex has been described that may include fever, myalgia/myositis, arthralgia/arthritis, serositis, vasculitis, increased ESR, leukocytosis and eosinophilia, and a positive test for antinuclear antibodies. Skin rash, photosensitivity reactions, or other skin manifestations may occur.
From the urinary system: infrequently – impaired renal function, proteinuria, renal failure; rarely – oliguria.
From the reproductive system: infrequently – decreased potency; rarely – gynecomastia.
From the musculoskeletal system: infrequently – muscle cramps.
From laboratory parameters: often – hyperkalemia, increased concentration of creatinine in the blood serum; infrequently – hyponatremia, increased concentration of urea in the blood serum; rarely – increased activity of liver transaminases and bilirubin concentration.
Allergic reactions: often – hypersensitivity reactions/angioedema of the face, lips, tongue, pharynx and/or larynx; infrequently – skin itching, urticaria.
Other: frequency unknown – syndrome of inappropriate ADH secretion.
Adverse events identified during post-marketing use of the drug Enap®, but no causal relationship with the drug has been established: urinary tract infections, upper respiratory tract infections, bronchitis, cardiac arrest, atrial fibrillation, herpes zoster, melena, ataxia, thromboembolism of the branches of the pulmonary artery and pulmonary infarction, hemolytic anemia, including cases of hemolysis in patients with deficiency glucose-6-phosphate dehydrogenase.
Interaction
Interaction
The risk of developing arterial hypotension, hyperkalemia and renal dysfunction (including acute renal failure) is higher in the case of double blockade of the RAAS, i.e. with simultaneous use of angiotensin II receptor antagonists, ACE inhibitors or aliskiren, compared with the use of a drug from one of the listed groups. If simultaneous use of drugs is necessary, it is recommended to monitor blood pressure, renal function and water and electrolyte balance.
Concomitant use of enalapril with aliskiren in patients with diabetes mellitus or renal impairment (KR
ACE inhibitors reduce potassium loss caused by diuretics. The simultaneous use of enalapril and potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene, amiloride), potassium supplements or potassium-containing salt substitutes, as well as the use of other drugs that increase the content of potassium in the blood plasma (for example, heparin) can lead to hyperkalemia. If concomitant use is necessary, use caution and regularly monitor serum potassium levels.
Previous therapy with diuretics in high doses may lead to a decrease in blood volume and an increased risk of developing arterial hypotension during the initiation of enalapril therapy. Excessive antihypertensive effects can be reduced by discontinuing the diuretic, increasing water or table salt intake, and by starting treatment with enalapril at a low dose.
Concomitant use of beta-blockers, alpha-blockers, ganglion-blocking agents, methyldopa, slow calcium channel blockers, nitroglycerin or other nitrates with enalapril can further reduce blood pressure.
With the simultaneous use of ACE inhibitors with lithium preparations, a transient increase in serum lithium concentration and the development of lithium intoxication were observed. The use of thiazide diuretics may lead to an additional increase in serum lithium concentrations and the risk of lithium toxicity with simultaneous use of ACE inhibitors. Concomitant use of enalapril with lithium is not recommended. If this combination is necessary, serum lithium concentrations should be carefully monitored.
The simultaneous use of certain anesthetics, tricyclic antidepressants and antipsychotics (neuroleptics) with ACE inhibitors may lead to an additional decrease in blood pressure.
Concomitant use of NSAIDs (including selective COX-2 inhibitors) may weaken the antihypertensive effect of ACE inhibitors or angiotensin II receptor antagonists. NSAIDs and ACE inhibitors have an additive effect on increasing serum potassium, which may lead to a reversible deterioration of renal function, especially in patients with existing renal impairment.
In rare cases, acute renal failure may develop, especially in patients with impaired renal function (for example, in elderly patients or with severe hypovolemia, including while using diuretics). Before starting therapy, it is necessary to replenish the blood volume. During treatment, it is recommended to monitor renal function.
Epidemiological studies suggest that the simultaneous use of ACE inhibitors and hypoglycemic agents (insulin and oral hypoglycemic drugs) may lead to an increased hypoglycemic effect with a risk of developing hypoglycemia. More often, hypoglycemia develops in the first weeks of therapy in patients with impaired renal function.
Ethanol enhances the antihypertensive effect of ACE inhibitors.
Sympathomimetics may reduce the antihypertensive effects of ACE inhibitors.
It is safe to use enalapril simultaneously with acetylsalicylic acid (as an antiplatelet agent), thrombolytics and beta-blockers.
Weakens the effect of medications containing theophylline.
Concomitant use of allopurinol, cytostatics and immunosuppressants (including methotrexate, cyclophosphamide) with ACE inhibitors may increase the risk of developing leukopenia. When used simultaneously with allopurinol, the risk of developing an allergic reaction increases, especially in patients with impaired renal function.
Concomitant use of cyclosporine with ACE inhibitors may increase the risk of developing hyperkalemia.
Antacids may reduce the bioavailability of ACE inhibitors.
When using ACE inhibitors, incl. enalapril, in patients receiving intravenous gold preparations (sodium aurothiomalate), a symptom complex was described, including facial flushing, nausea, vomiting, and arterial hypotension.
There were no clinically significant pharmacokinetic interactions of enalapril with hydrochlorothiazide, furosemide, digoxin, timolol, methyldopa, warfarin, indomethacin, sulindac and cimetidine.
When used simultaneously with propranolol, the concentration of enalaprilat in the blood serum decreases, but this effect is clinically insignificant.
Overdose
Overdose
Symptoms: approximately 6 hours after ingestion – a pronounced decrease in blood pressure up to the development of collapse, water-electrolyte imbalance, renal failure, hyperventilation, tachycardia, palpitations, bradycardia, dizziness, anxiety, cough, convulsions, stupor. After oral administration of enalapril at a dose of 300 and 440 mg, serum concentrations of enalaprilat in blood plasma exceeded the usual therapeutic concentrations by 100 and 200 times, respectively.
Treatment: the patient should be placed in a horizontal position with a low headboard. In mild cases, gastric lavage and ingestion of activated carbon are indicated; in more serious cases – intravenous infusion of 0.9% sodium chloride solution, plasma expanders, and, if necessary, intravenous administration of catecholamines. It is possible to remove enalaprilat by hemodialysis, the elimination rate is 62 ml/min. In patients with bradycardia that is resistant to therapy, pacemaker placement is indicated. Serum electrolytes and serum creatinine concentrations should be carefully monitored.
Storage conditions
Storage conditions
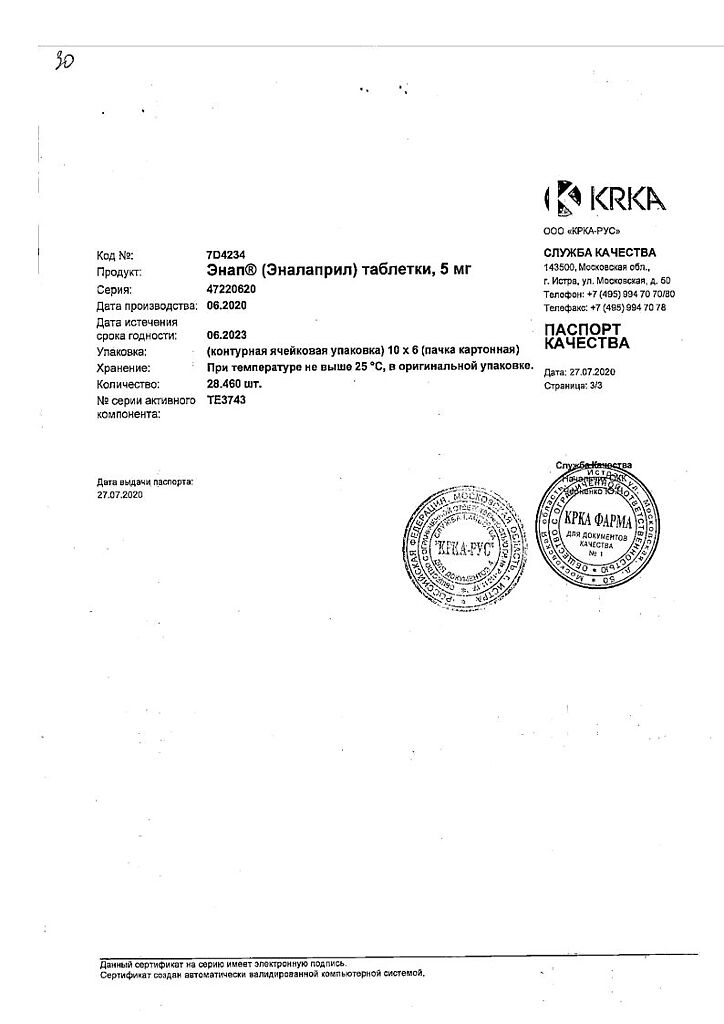
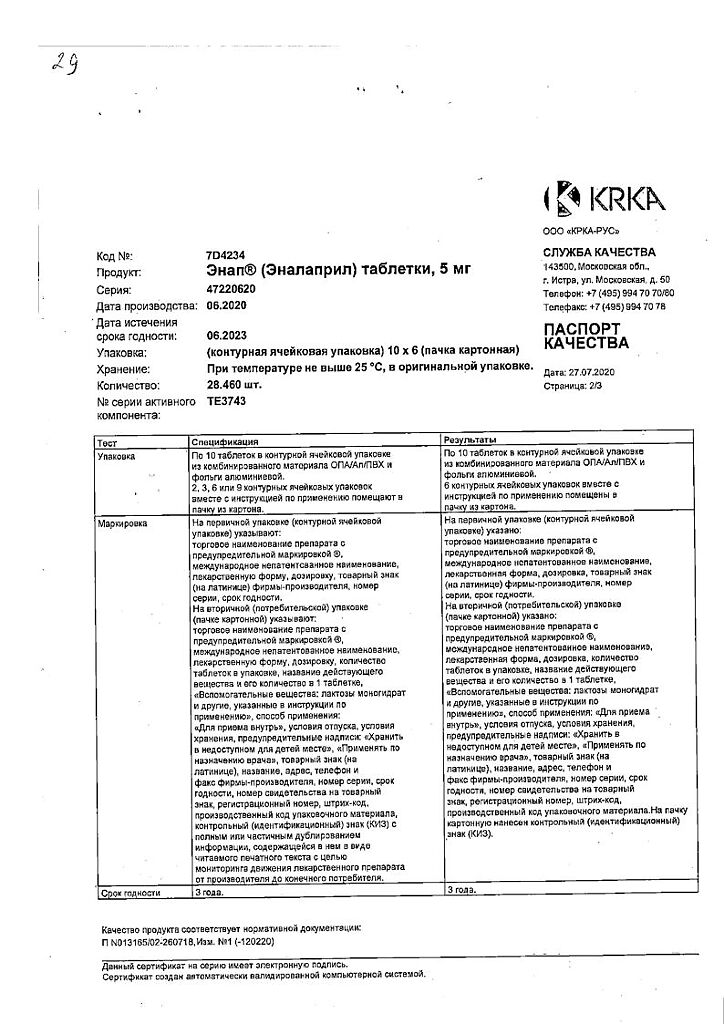
The drug should be stored out of the reach of children, protected from moisture at a temperature not exceeding 25°C.
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
KRKA-RUS/KRKA, Russia
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | The drug should be kept out of reach of children, protected from moisture at a temperature not exceeding 25°C. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Enap, tablets 5 mg 60 pcs with delivery to USA, UK, Europe and over 120 other countries.