No products in the cart.
Enalapril, tablets 10 mg 20 pcs
€2.01 €1.68
Description
Pharmgroup:
A ACE inhibitor.
Pharm action:
The ACE inhibitor is a hypotensive drug; its mechanism of action is related to reduction of formation from angiotensin I of angiotensin II, reduction of concentration of which leads to direct reduction of aldosterone secretion.
This decreases RPS, systolic and diastolic BP, post- and preload on myocardium.
Dilates arteries to a greater extent than veins, and there is no reflex increase in HR.
Decreases bradykinin degradation, increases Pg synthesis. Hypotensive effect is more pronounced at high plasma renin concentration than at normal or reduced concentration.
The decrease of BP within therapeutic limits has no effect on cerebral blood flow; blood flow in cerebral vessels is maintained at a sufficient level even against the background of reduced BP.
Enhances coronary and renal blood flow. With prolonged use it decreases LV myocardial hypertrophy and myofibrillar resistance arterial walls, prevents the progression of CHF and slows the development of LV dilatation.
It improves blood supply to ischemic myocardium.
Limits platelet aggregation. Prolongs survival in patients with CHF and slows the progression of LV dysfunction in patients who had myocardial infarction without clinical manifestations of CHF.
It has some diuretic effect. It reduces intracolumnar hypertension, slowing down the development of glomerulosclerosis and the risk of CKD.
Enalapril is a “prodrug”: its hydrolysis produces enalaprilate, which inhibits ACE.
The time of onset of hypotensive effect with oral administration is 1 hour, it reaches a maximum after 4-6 hours and lasts up to 24 hours.
In some patients, therapy for several weeks is necessary to achieve optimal BP levels. In patients with CHF, a significant clinical effect is seen with long-term treatment of 6 months or more.
Pharmacokinetics:
After oral administration absorption is 60%. Food intake has no effect on absorption.
In the liver it is metabolized to form the active metabolite enalaprilat, which is a more effective ACE inhibitor than enalapril.
The binding to plasma proteins of enalaprilat is 50-60%. TCmax of enalapril is 1 h, of enalaprilat 3-4 h. Enalaprilat easily passes through the histohematic barriers, excluding the BBB, a small amount passes through the placenta and into breast milk.
The T1/2 of enalaprilat is 11 h. It is excreted mainly by the kidneys – 60% (20% as enalapril and 40% as enalaprilat), through the intestine – 33% (6% as enalapril and 27% as enalaprilat).
Removable by hemodialysis (rate 62 ml/min) and peritoneal dialysis.
Indications
Indications
Arterial hypertension (symptomatic, renovascular, including with scleroderma, etc.), CHF I-III stages; prevention of coronary ischemia in patients with LV dysfunction, asymptomatic LV dysfunction.
Pharmacological effect
Pharmacological effect
Pharmgroup:
ACE inhibitor.
Pharmaceutical action:
An ACE inhibitor is an antihypertensive drug, the mechanism of action is associated with a decrease in the formation of angiotensin II from angiotensin I, a decrease in the concentration of which leads to a direct decrease in aldosterone secretion.
At the same time, peripheral resistance, systolic and diastolic blood pressure, post- and preload on the myocardium decrease.
Dilates arteries to a greater extent than veins, while no reflex increase in heart rate is observed.
Reduces bradykinin degradation, increases Pg synthesis. The hypotensive effect is more pronounced at high plasma renin concentrations than at normal or reduced levels.
A decrease in blood pressure within therapeutic limits does not affect cerebral circulation; blood flow in the vessels of the brain is maintained at a sufficient level even against the background of reduced blood pressure.
Strengthens coronary and renal blood flow. With long-term use, hypertrophy of the LV myocardium and myofibril of the walls of resistive arteries decreases, prevents the progression of CHF and slows down the development of LV dilatation.
Improves blood supply to ischemic myocardium.
Reduces platelet aggregation. Extends life expectancy in patients with CHF, slows the progression of LV dysfunction in patients who have had myocardial infarction without clinical manifestations of HF.
Has some diuretic effect. Reduces intraglomerular hypertension, slowing the development of glomerulosclerosis and the risk of chronic renal failure.
Enalapril is a “prodrug”: as a result of its hydrolysis, enalaprilat is formed, which inhibits ACE.
The onset of the hypotensive effect when taken orally is 1 hour, it reaches a maximum after 4-6 hours and lasts up to 24 hours.
In some patients, therapy for several weeks is necessary to achieve optimal blood pressure levels. In CHF, a noticeable clinical effect is observed with long-term treatment – 6 months or more.
Pharmacokinetics:
After oral administration, absorption is 60%. Eating does not affect absorption.
It is metabolized in the liver to form the active metabolite enalaprilat, which is a more effective ACE inhibitor than enalapril.
The binding of enalaprilat to plasma proteins is 50-60%. TCmax of enalapril – 1 hour, enalaprilat – 3-4 hours. Enalaprilat easily passes through histohematic barriers, excluding the BBB, a small amount penetrates the placenta and into breast milk.
T1/2 of enalaprilat – 11 hours. Excreted mainly by the kidneys – 60% (20% – in the form of enalapril and 40% – in the form of enalaprilat), through the intestines – 33% (6% – in the form of enalapril and 27% – in the form of enalaprilat).
It is removed by hemodialysis (rate 62 ml/min) and peritoneal dialysis.
Special instructions
Special instructions
Caution must be exercised when prescribing to patients with reduced blood volume (as a result of diuretic therapy, limiting salt intake, hemodialysis, diarrhea and vomiting) – the risk of a sudden and pronounced decrease in blood pressure is increased after using even the initial dose of an ACE inhibitor.
Transient hypotension is not a contraindication for continuing treatment with the drug after stabilization of blood pressure. In case of a repeated pronounced decrease in blood pressure, the dose should be reduced or the drug discontinued.
If an excessive decrease in blood pressure develops, the patient is transferred to a horizontal position with a low head, and, if necessary, a 0.9% NaCl solution and plasma-substituting drugs are administered.
The use of high-flow dialysis membranes (including AN69) increases the risk of developing an anaphylactic reaction. Adjustment of the dosage regimen on days free from dialysis should be carried out depending on blood pressure.
Before and during treatment with ACE inhibitors, it is necessary to monitor blood pressure, blood parameters (Hb, K+ concentration, creatinine, urea, liver enzyme activity), and protein in the urine.
Patients with decompensated CHF, ischemic heart disease and cerebral vascular diseases, in whom a sharp decrease in blood pressure can lead to myocardial infarction, stroke or impaired renal function, should be carefully monitored.
Sudden cessation of treatment does not lead to withdrawal syndrome (a sharp rise in blood pressure).
Patients with a history of angioedema have an increased risk of developing it when taking ACE inhibitors.
For newborns and infants who have been exposed in utero to ACE inhibitors, it is recommended to conduct careful monitoring for timely detection of a pronounced decrease in blood pressure, oliguria, hyperkalemia and neurological disorders that may be due to a decrease in renal and cerebral blood flow with a decrease in blood pressure caused by ACE inhibitors.
With oliguria, it is necessary to maintain blood pressure and renal perfusion by administering appropriate fluids and vasoconstrictor drugs.
In patients with reduced renal function, the single dose should be reduced or the intervals between doses should be increased.
Before studying the functions of the parathyroid glands, enalapril should be discontinued.
Caution should be exercised when performing physical exercise or in hot weather (risk of dehydration and excessive reduction in blood pressure due to a decrease in blood volume).
Before surgery (including dentistry), the surgeon/anesthesiologist must be warned about the use of ACE inhibitors.
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions (dizziness is possible, especially after taking the initial dose of an ACE inhibitor in patients taking diuretic drugs).
Active ingredient
Active ingredient
Enalapril
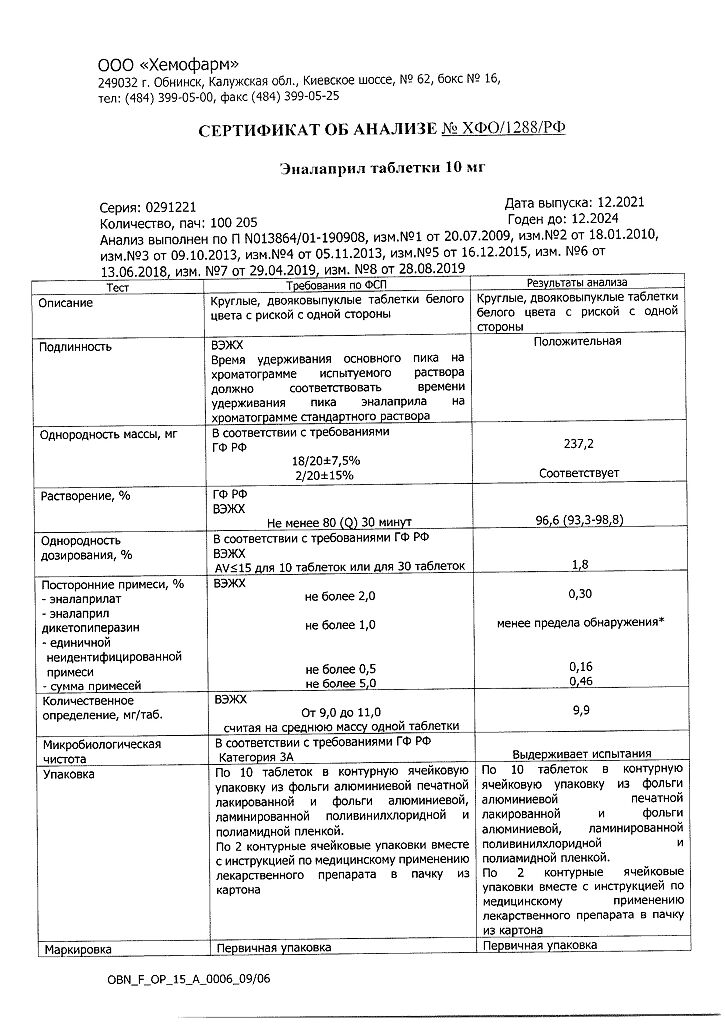
Composition
Composition
1 tablet 10 mg contains:
Active substance:
Enalapril maleate – 10 mg.
Excipients:
Lactose monohydrate – 125,000 mg,
Magnesium carbonate – 84,600 mg,
Gelatin – 9,200 mg,
Crospovidone – 9,200 mg,
Magnesium stearate – 2,000 mg.
Contraindications
Contraindications
Hypersensitivity to enalapril and other ACE inhibitors, a history of angioedema associated with treatment with ACE inhibitors, porphyria, pregnancy, lactation, age under 18 years (efficacy and safety have not been established).
Use with caution in case of primary hyperaldosteronism, bilateral renal artery stenosis, stenosis of the artery of a single kidney, hyperkalemia, condition after kidney transplantation; aortic stenosis,
mitral stenosis (with hemodynamic disturbances), idiopathic hypertrophic subaortic stenosis, systemic connective tissue diseases, coronary heart disease, cerebrovascular diseases,
diabetes mellitus, renal failure (proteinuria – more than 1 g/day), liver failure, in patients on a salt-restricted diet or on hemodialysis, while taking immunosuppressants and saluretics, in elderly people (over 65 years).
Side Effects
Side Effects
From the cardiovascular system: excessive decrease in blood pressure, orthostatic collapse, rarely – chest pain, angina pectoris, myocardial infarction (usually associated with a pronounced decrease in blood pressure), arrhythmias (atrial brady- or tachycardia, atrial fibrillation), palpitations, thromboembolism of the branches of the pulmonary artery.
From the nervous system: dizziness, fainting, headache, weakness, insomnia, anxiety, confusion, fatigue, drowsiness (2-3%), very rarely when used in high doses – nervousness, depression, paresthesia.
From the senses: disorders of the vestibular apparatus, hearing and vision impairment, tinnitus.
From the digestive system: dryness of the oral mucosa, loss of appetite, dyspeptic disorders (nausea, diarrhea or constipation, vomiting, abdominal pain), intestinal obstruction, pancreatitis, impaired liver function and biliary excretion, hepatitis, jaundice.
From the respiratory system: nonproductive “dry” cough, interstitial pneumonitis, bronchospasm, shortness of breath, rhinorrhea, pharyngitis.
Allergic reactions: skin rash, angioedema of the face, small intestine (very rarely), limbs, lips, tongue, glottis and/or larynx, dysphonia, exfoliative dermatitis, exudative erythema multiforme (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome), pemphigus (pemphigus), cutaneous itching, urticaria, photosensitivity, serositis, vasculitis, myositis, arthralgia, arthritis, stomatitis, glossitis.
From laboratory parameters: hypercreatininemia, increased urea concentration, increased activity of “liver” transaminases, hyperbilirubinemia, hyperkalemia, hyponatremia, decreased Hb and hematocrit, increased ESR, thrombocytopenia, neutropenia, agranulocytosis (in patients with autoimmune diseases), eosinophilia.
From the urinary system: impaired renal function, proteinuria.
Other: alopecia, decreased libido, flushing of the face. Cases of hypoglycemia have been reported in patients with diabetes mellitus who took insulin and oral hypoglycemic drugs.
Interaction
Interaction
Enhances the effect of ethanol, slows down the excretion of Li+.
Weakens the effect of drugs containing theophylline.
The hypotensive effect is reduced by NSAIDs, incl. selective COX-2 inhibitors, estrogens; enhance – diuretics, other antihypertensive drugs (beta-blockers, methyldopa, nitrates, BMCA, hydralazine, prazosin), drugs for general anesthesia, ethanol.
Potassium-sparing diuretics and potassium-containing drugs increase the risk of developing hyperkalemia.
Drugs that cause bone marrow suppression increase the risk of developing neutropenia and/or agranulocytosis.
With the simultaneous use of ACE inhibitors and gold preparations for parenteral use (sodium aurothiomalate), a symptom complex has been described, including facial flushing, nausea, vomiting and decreased blood pressure.
Concomitant use with insulin and oral hypoglycemic drugs increases the risk of hypoglycemia.
Immunosuppressants, allopurinol, cytostatics increase hematotoxicity.
Overdose
Overdose
Symptoms:
excessive decrease in blood pressure, up to the development of collapse, myocardial infarction, acute cerebrovascular accident or thromboembolic complications; convulsions, stupor.
Treatment:
the patient is transferred to a horizontal position with a low headboard. In mild cases, gastric lavage and ingestion of saline solution are indicated; in more serious cases, measures aimed at stabilizing blood pressure are indicated:
intravenous administration of 0.9% NaCl solution, plasma expanders, if necessary, intravenous administration of angiotensin II, hemodialysis (enalaprilat excretion rate – 62 ml/min).
Storage conditions
Storage conditions
In a place protected from moisture, at a temperature of 15–25 °C
Shelf life
Shelf life
3 years
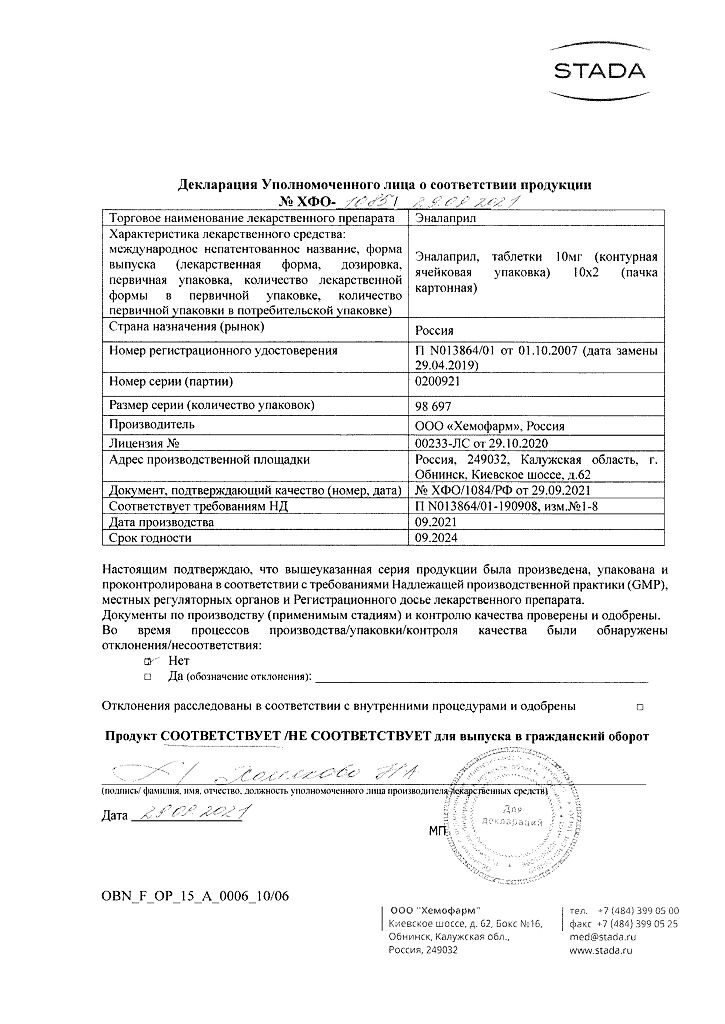
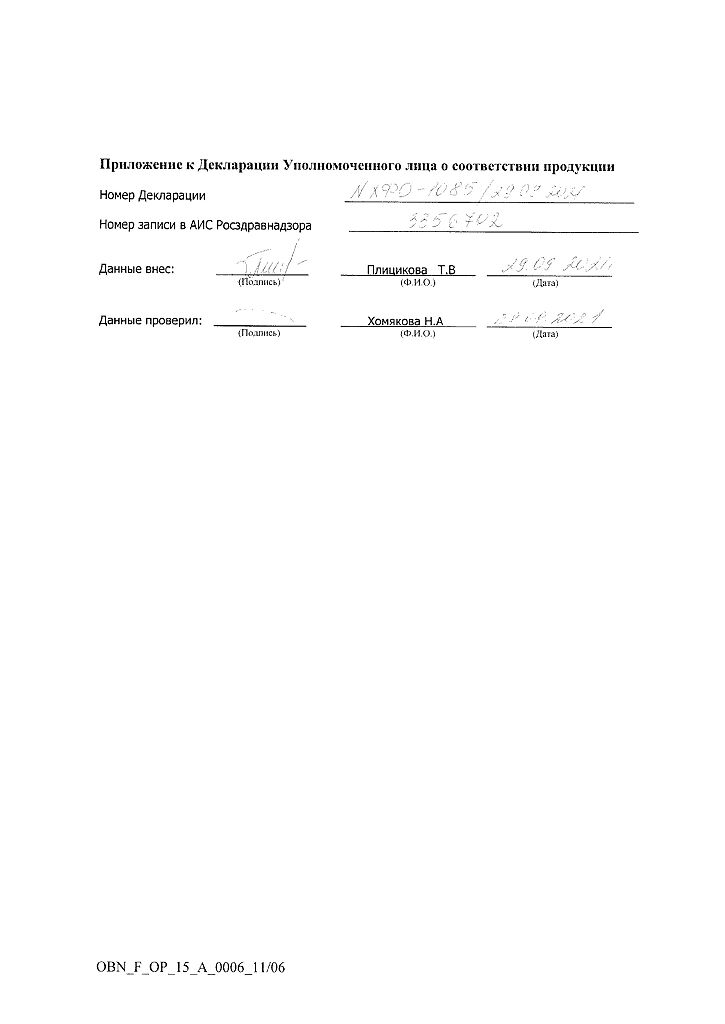
Manufacturer
Manufacturer
Hemofarm LLC, Russia
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a moisture-proof place, at 15-25 °C |
| Manufacturer | Chemopharm LLC, Russia |
| Medication form | pills |
| Brand | Chemopharm LLC |
Other forms…
Related products
Buy Enalapril, tablets 10 mg 20 pcs with delivery to USA, UK, Europe and over 120 other countries.