No products in the cart.
Egolanza, 10 mg 28 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Egolanza is an antipsychotic (neuroleptic).
Olanzapine is an antipsychotic (neuroleptic) with a wide pharmacological spectrum of effects on a number of receptor systems. It has an affinity for serotonin (5-NT2A/C 5NTZ, 5NT6), dopamine (D1, D2, D3, D4, D5), muscarinic (M1-5), adrenergic (alpha1) and histamine (H1) receptors.
Antagonism to serotonin (5NT), dopamine and cholinergic receptors was detected. It has a more pronounced affinity and activity towards serotonin 5NTt receptors compared to dopamine D2 receptors.
It selectively decreases excitability of meulimbic (A10) dopaminergic neurons and has a slight effect on striatal (A9) nerve pathways involved in the regulation of motor functions.
Limits conditioned protective reflex at lower doses than catalepsy-inducing doses. Enhances the anti-anxiety effect of the “anxiolytic” test. Significantly reduces productive (including delirium, hallucinations) and negative symptoms.
Indications
Indications
Schizophrenia (exacerbation, maintenance and long-term antiretroviral therapy). Bipolar affective disorder (monotherapy or in combination with Li+ drugs or valproic acid): acute manic or mixed episodes with/without psychotic manifestations and with/without rapid phase change.
Bipolar relapse and prevention of bipolar relapse (if the drug is effective in treating the manic phase).
Active ingredient
Active ingredient
How to take, the dosage
How to take, the dosage
Ingestion, regardless of meals, once, 5-20 mg/day. In schizophrenia in adults, the recommended initial dose is 10 mg/day. In acute mania associated with bipolar disorders in adults, 15 mg/day (1 time) as monotherapy or 10 mg/day (1 time) in combination with Li+ or valproic acid (maintenance therapy at the same dose).
Prevention of recurrence of bipolar disorder: The recommended starting dose is 10 mg daily. Patients who previously received olanzapine for treatment of a manic episode should continue treatment at the same dose to prevent relapse. In the presence of a new manic, mixed or depressive episode, olanzapine should be continued (adjusting the dose if necessary); if clinically indicated, mood medications should be prescribed additionally.
In the treatment of schizophrenia, manic episode, and for the prevention of recurrence of bipolar disorder, the daily dose may subsequently be adjusted between 5 and 20 mg, taking into account the clinical condition of the individual patient. Dose adjustments beyond the value recommended as the starting dose are recommended only after careful clinical review, and should generally occur at intervals of at least 24 hours.
The dose should be gradually reduced before discontinuing olanzapine. The maximum daily dose of olanzapine is 20 mg.
Smokers should be prescribed the drug in the same doses as non-smoking patients. If there is more than one factor that may cause metabolic retardation (female sex, older age, nonsmoking patients), consideration should be given to reducing the initial dose to 5 mg/day. If necessary, the dose may be further increased with caution.
Interaction
Interaction
CYP1A2 isoenzyme inducers or inhibitors may alter the metabolism of olanzapine. CYP1A2 isoenzyme inducers: clearance of olanzapine is increased in smoking patients and with concomitant use of carbamazepine, which leads to decreased plasma concentration of olanzapine. It may be necessary to increase the dose of the drug. CYP1A2 isoenzyme inhibitors: fluvoxamine significantly inhibits metabolism of olanzapine. By reducing clearance of olanzapine, it increases Csh of olanzapine by 54% in non-smoking women and by 77% in smoking men, AUC by 52% and 108%, respectively, so patients taking fluvoxamine or any other CYP1A2 inhibitor (such as ciprofloxacin) should consider using a lower starting dose of olanzapine.
Activated charcoal reduces the bioavailability of olanzapine by 50-60% and should be taken at least 2 hours before or 2 hours after olanzapine.
Fluoxetine (a CYP2D6 inhibitor), as well as single administration of antacids (aluminum or magnesium) or cimetidine, had no significant effect on the pharmacokinetics of olanzapine.
Ethanol had no effect on the pharmacokinetics of olanzapine in equilibrium; however, administration of ethanol together with olanzapine may be accompanied by an increase in the pharmacological effects of olanzapine (sedation).
Olanzanine slightly inhibits the formation of valproic acid glucuronide (the main metabolic pathway). Valproic acid slightly affects the metabolism of olanzapine. A clinically significant pharmacokinetic interaction between olanzapine and valproic acid is unlikely.
Caution is necessary when using olanzapine with drugs that prolong the QTc interval (amitriptyline, chlorpromazine. droperidol, thioridazine, pimozide, quinidine, procainamide, sotalol, ephedrine, adrenaline, terbutaline, erythromycin, trimethoprim/sulfamethoxazole, ketoconazole, fluconazole, etc) that disrupt electrolyte balance or inhibit hepatic metabolism of olanzapine.
The concomitant use of olanzapine and antiparkinsonian drugs in patients with Parkinson’s disease and dementia is not recommended.
Olanzapine is antagonistic to dopamine and may, in theory, inhibit the effects of levodopa and dopamine agonists.
Olanzapine does not inhibit the major CYP450 isoenzymes in vitro (e.g., 1A2, 2D6, 2C9, 2C19, ZA4), a clinically significant interaction is unlikely. No inhibition of metabolism of the following active substances has been found: tricyclic antidepressants (representing mainly CYP2D6 pathway), warfarin (CYP2C9), theophylline (CYP1A2) or diazepam (CYP3A4 and 2C19).
No interaction has been found with lithium or biperiden when used concomitantly.
Special Instructions
Special Instructions
An improvement in the clinical condition of patients may occur over a period of days or weeks while on antipsychotic medication. During this period, patients need close monitoring.
Psychosis and/or behavioral disorders associated with dementia
Olanzapine is not approved for the treatment of psychosis and/or behavioral disorders associated with dementia, and this medication is not recommended for use in such patients because of increased mortality and risk of cerebrovascular events. Cerebrovascular disorders (stroke, transient ischemic attack), including fatal outcomes, have been reported in elderly patients with psychosis with dementia. These patients had previous risk factors (cerebrovascular disorders (history), transient ischemic attacks, arterial hypertension, smoking), as well as concomitant diseases and/or drug intake, in time associated with cerebrovascular disorders.
The use of olanzapine is not recommended for the treatment of psychosis associated with dopamine agonist administration in patients with Parkinson’s disease.
Malignant neuroleptic syndrome (MNS)
Malignant neuroleptic syndrome may develop during treatment with neuroleptics (including olanzapine). Clinical manifestations of MNS are fever, muscle rigidity, mental changes, instability of autonomic functions (unstable levels of heart rate and blood pressure, tachycardia, sweating, cardiac arrhythmia). Additional signs may include elevated levels of creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure. If a patient develops symptoms and signs of MNS or unexplained fever without additional clinical manifestations of MNS, all antipsychotics, including olanzapine, should be discontinued.
Hyperglycemia and diabetes mellitus
A higher prevalence of diabetes mellitus has been noted in patients with schizophrenia. Very rare cases of hyperglycemia, development of diabetes mellitus or exacerbation of pre-existing diabetes mellitus, ketoacidosis and diabetic coma have been reported. A causal relationship between antipsychotic medications and these conditions has not been established. Clinical monitoring of patients with diabetes mellitus or with risk factors for its development is recommended.
Changes in lipid levels
If lipid levels change with olanzapine, appropriate treatment should be prescribed, especially in patients with dyslipidemia or risk factors for fat metabolism disorders.
Anticholinergic activity
Although olanzapine has anticholinergic activity in vitro, due to limited clinical experience with olanzapine in patients with comorbidities, caution is recommended when prescribing this drug in patients with prostatic hypertrophy, paralytic ileus and other similar conditions.
Hepatic function
Particular caution is required when hepatic transaminases, ALT and/or ACT are elevated in patients with hepatic insufficiency or receiving treatment with potentially hepatotoxic drugs. Monitoring of the patient and, if necessary, dose reduction is required. If hepatitis (including hepatocellular, cholestatic or mixed liver disease) is detected, olanzapine should be discontinued.
Neutropenia
Olanzapine should be used with caution in patients with decreased number of leukocytes including neutrophils; with signs of inhibition or toxic dysfunction of bone marrow under the influence of drugs (in anamnesis); with suppression of bone marrow function due to concomitant disease, radio- or chemotherapy (history); with hypereosinophilia or myeloproliferative disease. Neutropenia is often seen with the combined use of olanzapine and valproate. The use of olanzapine in patients with clozapine-dependent neutropenia or agranulocytosis (history) was not accompanied by recurrence of these disorders.
The discontinuation of the drug
When olanzapine is discontinued abruptly in very rare cases (
The OT interval
As with other antipsychotic medications, caution should be exercised during treatment with olanzapine if this medication is prescribed concomitantly with QTc interval prolonging medications, especially in elderly patients, patients with congenital QT prolongation syndrome, congestive heart failure, cardiac hypertrophy, hypokalemia, hypomagnesemia, or a family history of QT prolongation.
The concomitant use of other neuroleptics or drugs that also prolong the QT interval or cause hypokalemia should be avoided.
Thromboembolism
Coincidence in the timing of taking olanzapine and venous thromboembolism has been reported in rare cases (less than 0.01%). A causal link between the symptoms of venous thromboembolism and olanzapine administration has not been established. However, because schizophrenic patients often have acquired risk factors for venous thromboembolism, all possible risk factors for venous thromboembolism, such as patient immobility, should be identified and preventive measures taken.
Convulsive seizures
Olanzapine should be used with caution in patients who have a history of seizures or are exposed to factors that lower the seizure threshold. Seizures in patients receiving olanzapine are rare. Most of these cases have a history of seizures or risk factors for seizures.
Late dyskinesia
If signs of tardive dyskinesia develop, dose reduction or withdrawal of olanzapine is recommended. Symptoms of tardive dyskinesia may increase or manifest after drug withdrawal.
Ortostatic hypotension
In clinical trials of olanzapine, orthostatic hypotension was infrequently observed in elderly patients. As with other antipsychotic medications, periodic BP measurements are recommended in patients over 65 years of age.
Pediatric use
Olanzapine is not recommended for the treatment of children and adolescents. Studies in patients aged 13-17 years have found a variety of adverse reactions, including increased body weight, altered metabolic parameters, and increased prolactin levels. The long-term outcomes of these events have not been studied and remain unknown.
Lactose
This drug contains lactose, so it should not be prescribed in patients with rare hereditary galactose tolerance disorders, hereditary Sami lactase deficiency or glucose-galactose malabsorption. Caution should be exercised when using olanzapine in combination with other centrally acting drugs and ethanol.
Contraindications
Contraindications
Hypersensitivity to the active ingredient or any of the ingredients of the drug. Closed angle glaucoma. Psychosis and/or behavioral disorders associated with dementia. Period of lactation. Childhood (under 18 years of age due to insufficient clinical data). Lactose intolerance, lactase deficiency or glucose-galactose malabsorption (the drug contains lactose).
With caution
Liver failure, renal failure, prostatic hyperplasia, epilepsy, seizure syndrome in anamnesis, myelosuppression (including leukopenia, neutropenia). myeloproliferative diseases, hypereosinophilic syndrome, paralytic intestinal obstruction, pregnancy, cardiovascular and cerebrovascular diseases or other conditions predisposing to arterial hypotension, congenital increased QT interval on electrocardiogram (ECG) (increased corrected QT interval (QTc) on ECG), or in presence of conditions that may potentially cause QT interval prolongation (e.g., concomitant administration of QT interval prolongers, congestive heart failure, hypokalemia, hypomagnesemia), elderly age, as well as concomitant administration of other centrally acting drugs; immobilization.
Side effects
Side effects
Nervous system: very often – somnolence; often – dizziness, akathisia, parkinsonism, asthenia, dyskinesia; rarely – seizure syndrome (more often against a background of seizure syndrome in anamnesis); very rarely – dystonia (including oculogyric crisis) and tardive dyskinesia. Very rarely malignant neuroleptic syndrome (MNS) may develop. Clinical manifestations of MNS are fever, muscle stiffness, altered mental status, and instability of autonomic functions (erratic levels of heart rate and blood pressure, tachycardia, sweating, cardiac arrhythmia). Additional signs may include elevated levels of creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure. If a patient develops symptoms and signs of MNS or unexplained fever without additional clinical manifestations of MNS, all antipsychotics, including olanzapine, should be discontinued.
Symptoms such as increased sweating, insomnia, tremors, anxiety, nausea, or vomiting have very rarely been reported with abrupt withdrawal of the drug.
Cardiovascular system disorders: frequently – arterial hypotension (including orthostatic); infrequently – bradycardia with or without collapse; very rarely – prolongation of QTc interval on ECG, ventricular tachycardia/fibrillation and sudden death, very rarely – thromboembolism (including pulmonary embolism and deep vein thrombosis).
The digestive system: often – transient anticholinergic effects, including constipation and dry mouth; rarely – hepatitis; very rarely – pancreatitis.
Mechanisms: very often – weight gain; often – increase of appetite, hypertriglyceridemia; very rarely – hyperglycemia and/or decompensation of diabetes, sometimes manifested by ketoacidosis or coma, including lethal outcome; hypercholesterolemia, hypothermia.
Digestive system disorders: often – transient, asymptomatic increased activity of “liver” transaminases (alanine aminotransferase (ALT), aspartate aminotransferase (ACT), especially in treatment start; rarely – hepatitis (including hepatocellular, cholestatic or mixed liver damage).
Hematopoietic organs: often – eosinophilia; rarely – leukopenia; very rarely – thrombocytopenia, neutropenia.
Musculoskeletal system: very rare – rhabdomyolysis.
Urogenital system disorders: very rare – urinary retention, priapism.
The skin: rare – skin rash, infrequent – photosensitization reactions; very rare – alopecia.
Allergic reactions: rare – skin rash; very rare – anaphylactoid reactions, angioedema, pruritus or urticaria.
Others: frequent – asthenia, peripheral edema; very rare – withdrawal syndrome.
Laboratory findings: very common – hyperprolactinemia, but clinical manifestations (e.g., gynecomastia, galactorrhea and breast enlargement) are rare. Most patients have spontaneous normalization of prolactin levels without therapy withdrawal. Rarely – transient, asymptomatic increase in ALT, ACT. Infrequent – increase in creatine phosphokinase (CPK) activity; very rare – increase in alkaline phosphatase (ALP) activity and total bilirubin. In single cases, increases in plasma glucose concentrations, triglycerides, cholesterol, and asymptomatic eosinophilia have been observed.
In elderly patients with dementia, a higher incidence of death and cerebrovascular disorders (stroke, transient ischemic attacks) has been registered in studies. Gait disturbances and falls were very frequent in this category of patients. Pneumonia, elevated body temperature, lethargy, erythema, visual hallucinations, and urinary incontinence were also common.
Worsening of Parkinsonian symptoms and the development of hallucinations were frequently reported among patients with drug-induced (on dopamine agonists) psychosis in the background of Parkinson’s disease.
There are data about development of neutropenia (4.1%) against the background of combined therapy with valproic acid in patients with bipolar mania. Concomitant therapy with valproic acid or lithium contributes to an increased frequency (more than 10%) of tremor, dry mouth, increased appetite or increased body weight. Speech disorders (1 to 10%) have also been reported.
Overdose
Overdose
Symptoms: tachycardia, agitation/aggression, articulation disorder, extrapyramidal disorders, depression of consciousness of varying severity (from sedation to coma), delirium, seizures, malignant neuroleptic syndrome, respiratory depression, aspiration, high or low BP, arrhythmias, cardiac and respiratory arrest.
The minimum dose in acute fatal overdose was 450 mg, the maximum dose with a favorable outcome (survival) was 1500 mg.
Treatment: gastric lavage, administration of activated charcoal, symptomatic treatment, maintenance of respiratory function.
Do not use sympathomimetics (including norepinephrine, dopamine) that are beta-adrenoreceptor agonists (stimulation of these receptors may exacerbate BP decrease). Close medical observation and monitoring should continue until the patient is well.
Similarities
Similarities
Additional information
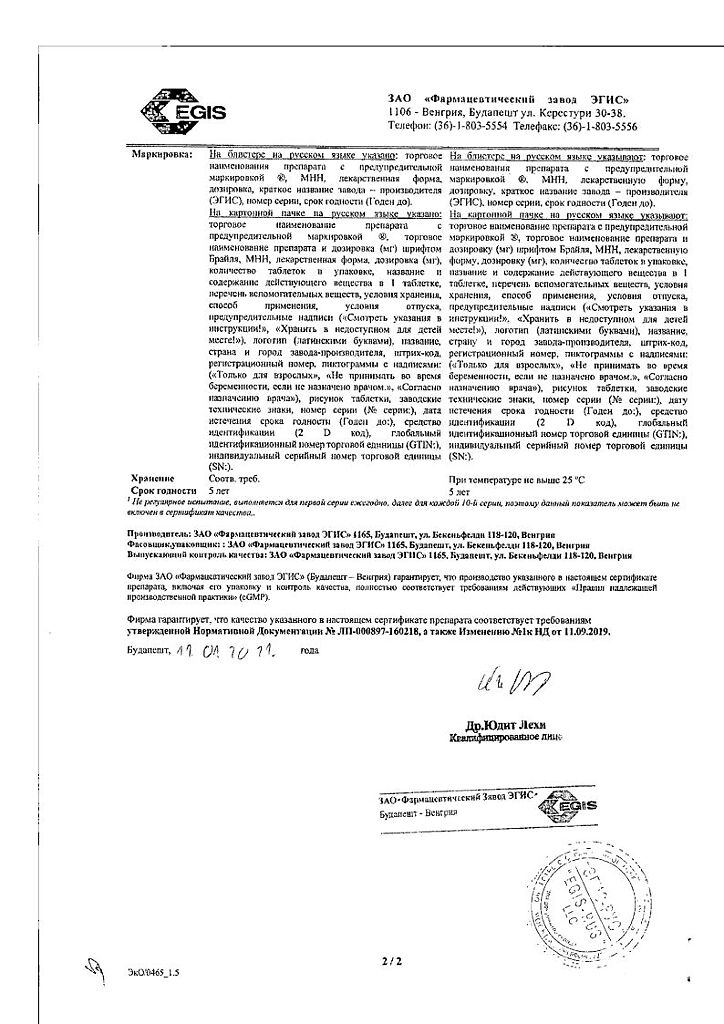
| Shelf life | 3 years |
|---|---|
| Conditions of storage | Store at the temperature not more than 30 °С. Keep the drug out of reach of children! |
| Manufacturer | EGIS, Hungary |
| Medication form | pills |
| Brand | EGIS |
Related products
Buy Egolanza, 10 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.